Back to Journals » Journal of Inflammation Research » Volume 15
Low Level FLT3LG is a Novel Poor Prognostic Biomarker for Cervical Cancer with Immune Infiltration
Authors chen L , Huang Y, Dong B, Gu Y, Li Y, Cang W, Sun P , Xiang Y
Received 29 August 2022
Accepted for publication 13 October 2022
Published 19 October 2022 Volume 2022:15 Pages 5889—5904
DOI https://doi.org/10.2147/JIR.S384908
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Lihua chen,1,2,* Yuxuan Huang,3,4,* Binhua Dong,3,4 Yu Gu,1,2 Ye Li,3,4 Wei Cang,1,2 Pengming Sun,3,4 Yang Xiang1,2
1Department of Obstetrics and Gynecology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing, People’s Republic of China; 2National Clinical Research Center for Obstetric & Gynecologic Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing, People’s Republic of China; 3Laboratory of Gynecologic Oncology, Department of Gynecology, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, People’s Republic of China; 4Fujian Key Laboratory of Women and Children’s Critical Diseases Research, Fuzhou, People’s Republic of China
*These authors contributed equally to work
Correspondence: Yang Xiang, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College, No. 1 Shuai Fu Yuan Wang Fu Jing, Dong Cheng District, Beijing, 100730, People’s Republic of China, Tel +86-1065296068, Fax +86-1065296218, Email [email protected] Pengming Sun, Fujian Provincial Maternity and Child Hospital, Affiliated Hospital of Fujian Medical University, 18 Daoshan Road, Fuzhou, Fujian, 350001, People’s Republic of China, Tel +86-591-87558732 ; +86-591-97279671, Fax +86-591-87551247, Email [email protected]
Introduction: The FMS-related tyrosine kinase 3 (FLT3) ligand (FLT3LG), a growth factor, binds to FLT3 on dendritic cell (DCs) to enhance their differentiation and expansion. It has shown great potential as an immunotherapy target for cancers. However, the expression and function of FLT3LG in cervical cancer remain largely unknown.
Materials and Methods: In this study, we obtained the expression of FLT3LG, the clinical prognosis in cervical cancer, via multiple databases, including The Cancer Genome Atlas (TCGA), the TISIDB database, and Tumor Immune Estimate Resource (TIMER). The results were further investigated using real-time quantitative PCR (qPCR) cytology specimens in 489 patients. Furthermore, Kaplan-Meier Cox regression and prognostic nomogram analyses were used to assess FLT3LG’s clinical significance in cervical cancer patients. All calculations used the R package.
Results: As a result, FLT3LG expression decreased in cervical cancer compared with standard samples. And the low expression of FLT3LG was associated with a poor prognosis. Furthermore, Receiver Operating Characteristics (ROC) analysis indicated that FLT3LG might serve as a valuable diagnostic biomarker for cervical cancer. Additionally, it indicated that the FLT3LG had the highest odds ratio (OR=10.519; (7.371– 27.071)) for detecting CIN 2+. In addition, our result also demonstrated that expression of FLT3LG was closely related to immune cells, immune inhibitors, immunostimulators, receptors, and chemokines in CESC.
Conclusion: Research on FLT3LG provided insight into its critical function. Hence, the low expression of FLT3LG may be a valuable biomarker in CESC patients linked with immune infiltration.
Keywords: FLT3LG, cervical cancer, prognosis, tumor-infiltrating, immune cells, immunotherapy
Introduction
Cervical cancer (CC) is the most common malignant tumor of the lower female genital tract. It has become a significant challenge to female health, despite initiatives to prevent cervical cancer with screening and vaccination.1 Nearly 604,127 new cases and 341,831 deaths were reported yearly.2 China has 10,9741 new cases and 59,060 deaths annually, an increasing trend.2 Recently, many articles have shown that effective surgery, technical radiotherapy, and the addition of bevacizumab to standard chemotherapy can significantly improve survival in cervical cancer patients.3,4 Unfortunately, the prognosis for patients with advanced or recurrent cervical cancer remains poor, and the treatment options remain limited.5 Hence, exploring effective prognostic and therapeutic targets for cervical cancer is urgent.
Immunotherapy is an emerging treatment option that might be a novel option to improve the prognosis of these patients. It has recently achieved great preclinical and clinical success through immune checkpoint inhibitors (ICIs).6–8 Nowadays, ICIs represent the most promising cancer treatment. However, only a fraction of patients received an immune response due to primary or acquired resistance. It is reported that nearly 85% of cancer patients have innate or acquired resistance to ICIs, which significantly limits their clinical application.9 Such resistance mechanisms may be due to dendritic cell (DCs) dysfunction, recruitment reduction, and T cell decreased or infiltration reduction.10 These resistance mechanisms can be corrected by therapeutic agents triggering cancer immune response or promoting DC activation.11–13 Targeted programmed cell death-1(PD-1), programmed cell death-Ligand 1 (PD-L1), and cytotoxic T lymphocyte-associated antigen-4 (CTLA-4) have a significant positive effect on cervical cancer. The Food and Drug Administration (FDA) has approved pembrolizumab for those patients with metastatic or recurrent cervical cancer for patients with metastatic or recurrent cervical cancer whose disease has progressed during or after chemotherapy.14,15 However, treatment options remain limited. Thus, it is essential to discover a novel target and available predictive biomarker to stratify patients who may benefit from immunotherapy in cervical cancer.
The FMS-related tyrosine kinase 3 (FLT3) ligand (FLT3LG), a growth factor, is mainly derived from lymphocytes in the tumor microenvironment (TME).16,17 It binds to FLT3 on DCs to enhance their differentiation and expansion.18 Therefore, it may assist DCs in tumor antigen presentation and antitumor immune response. In addition, mature DC express FLT3 and proliferate massively under the trigger of FLT3LG.19,20 Recently, Kalanxhi et al indicated that the serum FLT3LG level in patients after OXA neoadjuvant therapy was higher than the baseline level in locally advanced rectal cell cancer (RCC).21
Furthermore, Abrahamsson et al demonstrated circulating FLT3LG at baseline linked with RCC liver metastases.22 Their study showed that elevated circulating FLT3LG levels after neoadjuvant therapy were strongly associated with better prognosis, possibly due to a reduced risk of metastasis. It further illustrates that the FLT3LG levels in serum can be used as a predictive target after neoadjuvant therapy. In addition, elevated serum FLT3LG has been described clinically as a biomarker of recovery from chemotherapy-induced myelosuppression.22,23 Also, FLT3LG has been used to generate DCs from myeloid progenit or cells in vitro,24 but limited understanding of its immunomodulatory effect.
Given little research focused on FLT3LG, limited evidence has illustrated the expression level, function, and clinical value of FLT3LG in cervical cancer. This article aimed to evaluate the predictive and therapeutic value of FLT3LG in cervical cancer based on databases. This article developed a comprehensive analysis to provide further insight into the biological pathways, functional enrichment, and clinical significance involved in the cervical cancer-related FLT3LG regulatory network. This study opens a new perspective into the active role of FLT3LG in cervical cancer and highlights the underlying mechanistic basis by which FLT3LG affects immune cell-tumor interactions.
Materials and Methods
RNA-Sequencing Data and Bioinformatics Analysis
Normalized RNA-seq and clinicopathological data were acquired from TCGA-CESC datasets, including 306 cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC) sample tumor tissues and 13 normal tissues.25 And further analysis used the ClusteProfiler ggplot2 package in R (3.3.3).
TIMER Database Analysis
The Tumor Immune Estimation Resource (TIMER2.0) (https://timer.cistrome.org/) is a database used for the analysis of tumor-infiltrating immune cells and various gene expression levels in different types of cancer.26 We assessed the expression of FLT3LG in various tumors and the relationship with tumor-infiltrating lymphocytes (TILs) by gene modules. In addition, the association between FLT3LG level with markers of TILs has been investigated through correlation modules. And the significance of the estimation and correlation was analyzed by the correlation module.
Gene Expression Profiling Interaction Analysis
The Gene Expression Profiling Interactive Analysis (GEPIA)27 (http://gepia.cancer-pku.cn/index.html) is a valuable online database that got the data from TCGA and The Genotype-Tissue Expression (GTEx) databases. We used it to evaluate the correlation between FLT3LG levels and significant markers in CESC and healthy samples by the correlation Analysis.
Prognostic Model Establishment and Prediction
We established a nomogram to predict the overall survival (OS) in cervical cancer patients using the RMS R package (version 6.2–0) and survival package (version 3.2–10).28 It mainly consists of two parts, significant clinical features and calibration maps. The calibration curve was assessed graphically by comparing the nomogram predicted probabilities to the observed ratios, with the 45° line representing the best-predicted value.
The Concordance Index (C-index) was used to evaluate the discriminative power of the model. Additionally, receiver operating characteristic (ROC) and C-index were carried out to analyze the predictive accuracy.
TISIDB
TISIDB included various heterogeneous data sources to analyze the relationship between tumors and the immune system (http://cis.hku.hk/TISIDB/index.php). The database can assist researchers in further understanding how tumors and immune cells interact, predict the efficacy of immunotherapy, and identify new immunotherapy targets. It will be a valuable resource for cancer immunology research and therapy. In the present study, we analyzed the relationship between FLT3LG and 28 TILs, 24 immunoinhibitors, 40 immunostimulators, 41 chemokines, and 18 receptors in CESC by the TISIDB database.29
Patients and Clinical Samples
We included 489 participants with cervical specimens from December 2017 to September 2021 in the Fujian Provincial Maternity and Children’s Health Hospital, an affiliated hospital of Fujian Medical University. The population was selected from the Fujian Cervical Lesion Screening Cohort (FCC). The Hospital Ethics Committee of Fujian Provincial Maternity and Children’s Hospital, an affiliated hospital of Fujian Medical University, approved the study (2022KYLLR03050), and all individuals participating in this study signed written informed consent.
Quantitative Real-Time Polymerase Chain Reaction (RT-qPCR)
Specimen collection, sample management, liquid-based cytology, HPV genotyping test, and histology were described in the previous study.30,31 RT-qPCR was carried out according to the protocol. FLT3LG PCR was used with primer pairs 5′-GCT GGG TCC AAG ATG CAA GG-3′ and 5′-GGT CTG GAC GAA GCG AAG AC- 3′. GAPDH was used as an experimental control for sample quality and adequacy during the PCR process. GAPDH PCR was applied with primer pairs 5′-GGT GTG AAC CAT GAG AAG TAT GA-3′ and 5′-GAG TCC TTC CAC GAT ACC AAA G-3′. Relative levels of FLT3LG mRNA were calculated by the 2−ΔΔCT method.
Statistical Analysis
All data analysis and visualizations were performed using R (3.6.3).28 The FLT3LG expression was analyzed in unpaired samples using Wilcoxon rank-sum test, while paired samples were analyzed using Wilcoxon signed-rank test. Cox regression analysis and Kaplan-Meier analysis were performed to assess the prognostic factors. Using multivariate Cox analysis, we compared the impact of FLT3LG expression on survival and other clinical characteristics. We used the median FLT3LG expression as the cut-off point. Furthermore, we conducted ROC analysis using the pROC package to determine whether transcriptional expression of FLT3LG can accurately distinguish cervical cancer from healthy tissues. Different risks were estimated using odds ratios (ORs) and 95% confidence intervals (CIs). An area under the curve (AUC) of 0.5 to 1.0 indicates 50–100% discriminability. In all statistical analyses, P-values below 0.05 indicated statistical significance.
Results
FLT3LG Decreased in Cervical Cancer
RNA-seq data were downloaded from UCSC XENA (https://xenabrowser.net/datapages/) and analyzed uniformly through the toiling process. Based on an analysis of FLT3LG expression in TCGA and GTEX normal samples and corresponding tumor samples in TCGA, FLT3LG expression was significantly low among 16 cancer types, including CESC Figure 1A and B. In comparison, 13 cancer types expressed FLT3LG highly in Figure 1A. Furthermore, the expression of FLT3LG decreased in poor prognosis (Figure 1C–E).
Verification of FLT3LG Down-Expression in Our Cohort
To further determine the different expression levels of FLT3LG in cervical lesions, we collected 489 cervical specimens and clinical information. There were 121(24.74%) were normal, 96(19.63%) were defined as CIN1, 193(39.47%) as CIN2/3, and 79 (16.16%) as CC. According to Table 1, the participants had the following clinicopathologic characteristics. A significant relationship was found between cervical lesions and age, cytology, HPV genotype, and FLT3LG expression. We found that age, abnormal cytology, and HPV infections contributed to the development of CIN2+. Moreover, With the development of cervical lesions, the expression of FLT3LG decreased significantly, especially compared with CIN2+ (Figure 1F). It indicated that FLT3LG might serve as a predictor of CIN2+ lesions (p<0.01). It was similar to the results of TCGA analyses which showed that low levels of FLT3LG could predict worse pathologic stages in patients with CESC.
 |
Table 1 Clinical Characteristics of the Participants of the Study |
Decreased FLT3LG Predicts a Poor Prognosis in CESC
Based on TCGA-CESC data sets, a Kaplan-Meier survival analysis was conducted to investigate FLT3LG’s role in CESC survival. As shown in Figure 2A–C, low FLT3LG expression was significantly related to poor overall survival (OS) (HR = 0.46, 95% CI = 0.29–0.74, p = 0.001, Figure 2A). Similarly, we found a significant correlation between low FLT3LG expression and poor disease-specific survival (DSS)(HR = 0.45, 95% CI = 0.26–0.88, p = 0.004, Figure 2B) and progression-free interval (PFI) (HR = 0.55, 95% CI = 0.34–0.90, p = 0.016, Figure 2C). The univariate analysis demonstrated that the clinical stage, T stage, N stage, and M stage, as well as FLT3LG expression levels, affected CESC prognosis (all p < 0.05). According to multivariate Cox regression, the FLT3LG expression level was an independent risk factor in CESC patients (Table 2).
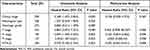 |
Table 2 Univariate and Multivariate Cox’s Regression Analysis of Factors Associated with OS in Cervical Cancer with TCGA Database |
We evaluated the impact of FLT3LG expression on the prognosis of low-stage CESC patients using subgroup analysis. According to Figure 2D–I, low FLT3LG expression is associated with poorer prognosis in stages T1 + T2, stages N0 + N1, M0, radiation therapy, different histological type (squamous cell carcinoma) and low clinical stage with OS (HR = 0.45, 95% CI = 0.23–0.88, p = 0.02, Figure 2D), (HR = 0.45, 95% CI = 0.22–0.90, p = 0.023, Figure 2E), (HR = 0.32, 95% CI = 0.11–0.90, p = 0.03, Figure 2F), (HR = 0.41, 95% CI = 0.23–0.72, p = 0.002, Figure 2G), (HR = 0.52, 95% CI = 0.31–0.87, p = 0.013, Figure 2H) and (HR = 0.31, 95% CI = 0.17–0.58, p < 0.001, Figure 2I), respectively.
FLT3LG Expression Can Serve as a Potential Diagnostic Biomarker for the Detection of CIN 2+
The reliability of FLT3LG mRNA expression level to distinguish cervical cancer from normal tissues was evaluated using ROC analysis. And the AUC was 0.820 (95% CI: 0.709–0.930, Figure 2J) in the TCGA-CESC dataset. Our cohort’s AUC was 0.811 (95% CI: 0.773–0.848, Figure 2K), and the optimal cut-off of FLT3LG mRNA was 0.405.
We calculated the independent factors that contributed to the diagnosis of the high-grade cervical lesion by multiple logistic regressions (Table 3). It is indicated that the FLT3LG had the highest OR (OR=10.519; 95% CI =7.371–27.071), as well as the following: TCT (OR=9.988; 95%=4.515–20.058), HPV-genotype (OR=8.256; 95% CI=4.150–18.436) and age (OR=2.637; 95%=1.336–5.207).
 |
Table 3 Independent Predictors for Detection of CIN2+ Lesions |
Prognostic Model of FLT3LG in CESC
The Cox regression analysis results created a nomogram using the RMS R package (Figure 3A). Based on a statistical significance level of 0.1, T stage and FLT3LG expression were chosen as independent prognostic factors in the prediction model. Multivariate Cox analysis was used to assign points to these variables. According to the FLT3LG-related Cox model, OS was predicted at 0.725 (0.689–0.761). A straight line was drawn to determine the variables’ points, and the sum of those points was scaled from 0 to 100. The total point topics probability of CESC patients was calculated from the points of each variable. To determine survival at 1, 3, and 5 years, a straight line was drawn from the total point axis to the outcome axis. According to the model, the probability of 1-year survival is < 20%, and 3- and 5-year < 10%. Based on the nomogram calibration curve, all patients’ observations were consistent with the prediction results (Figure 3B).
Association Between Immune Infiltration and FLT3LG Expression in CESC
Immune infiltration is a crucial factor related to tumor progression. In CESCs, FLT3LG expression was associated with immune cell infiltration levels using TIMER platforms. We analyzed the relationship between FLT3LG and 28 TILs. Figure 4A shows a strong correlation between FLT3LG expression level and TIL abundance. FLT3LG expression was strongly linked to CD8+ T cell (rho = 0.567), CD4+ T cell (rho = 0.396), T-cell regulatory (rho = 0.296), B cell (rho = 0.512), neutrophil (rho = 0.166), monocyte (rho = 0.728), and M1(rho = 0.499), myeloid dendritic cell (rho = 0.539), Mast cell activated (rho = 0.239), cancer-associated fibroblast (rho = 0.133), Hematopoietic stem cell (rho = 0.142), T cell follicular helper(rho = 0.464), T cell gamma delta (rho = 0.428). However, the FLT3LG expression level was negatively correlated with MDSC(rho = −0.441) (Figure 4B). All the p-values were below 0.001. These results demonstrated that FLT3LG plays an essential role in the immune infiltration of CESC.
GEPIA databases were used to analyze the relationship between FLT3LG and different biomarkers of TILs in CESC. We found that FLT3LG was significantly associated with most marker sets of Monocytes, TAMs, M1 macrophages, M2 macrophages, neutrophils, and T-cell exhaustion in CESC. Specifically, this study suggested that the makers of TAMs, T-cell exhaustion, and monocyte are all positively correlated with FLT3LG in CESC (p < 0.01; Figure 5 and Table 4). Therefore, FLT3LG may affect T-cell exhaustion and macrophage polarization in CESC.
 |
Table 4 Correlation Analysis Between FLT3LG and Related Genes and Markers of Monocyte, Macrophages, and T-Cell Exhaustion in Gene Expression Profiling Interaction Analysis (GEPIA) |
GEPIA databases were used to analyze the relationship between FLT3LG and 24 immunoinhibitors, 40 immunostimulators in CESC. The expression of FLT3LG is associated with immunomodulators in cervical cancer. Immunomodulators are important components that affect the function of the immune system. This research revealed that FLT3LG was significantly connected with immunoinhibitors (p < 2.2e−16), such as CD95 (rho = 0.564), CD244 (rho = 0.531), BTLA (rho = 0.525), CSF1R (rho = 0.484), KIR2DL3 (rho = 0.437), CTLA4 (rho = 0.573), HAVCR2 (rho = 0.716), IDO1 (rho = 0.538), TIGIT (rho = 0.576), PDCD1 (rho = 0.562), PDCD1LG2 (rho = 0.433), TIGIT (rho = 0.576) and LAG3 (rho = 0.625) (Figure 6A). The FLT3LG level was also strongly related with immunostimulators (p < 2.2e−16), including CD40LG (rho = 0.448), CD40 (rho = 0.533), C10orf54 (rho = 0.517), CD27 (rho = 0.61), CD48 (rho = 0.841), CD80 (rho = 0.455), CD86 (rho = 0.53), ICOS (rho = 0.567), LTA (rho = 0.637), KLRK1 (rho = 0.571), TNFRSF13B (rho = 0.489), TMIGD2 (rho = 0.507), TNFRSF14 (rho = 0.587), TNFRSF4 (rho = 0.483), and TNFSF13B (rho = 0.524), (Figure 6B). Hence, FLT3LG is intimately involved in modulating immune interactions and may facilitate tumor immune escape.
The Expression of FLT3LG is Associated with Chemokines in Cervical Cancer
Chemokines play a key role in regulating immune cell infiltration. We analyzed the relationship between FLT3LG and 41 chemokines and 18 receptors in CESC. According to this study, FLT3LG expression is associated with chemokine expression (p < 2.2e−16). FLT3LG expression was significantly linked with CCL5 (rho = 0.653), CCL4 (rho = 0.49.), CCL19 (rho = 0.476), CXCL9(rho = 0.459), CX3CL1 (rho = 0.448), XCL2 (rho = 0.513), CXCL13 (rho = 0.468), CXCL11 (rho = 0.454), and CXCL10 (rho = 0.554), (Figure 7A). In addition, we found significant correlations between FLT3LG expression and chemokine receptors (p < 2.2e−16), including CCR2 (rho = 0.424), CCR5 (rho = 0.565), CXCR5 (rho = 0.472), CXCR3 (rho = 0.586), and CXCR6 (rho = 0.597) (Figure 7B). Furthermore, based on these results, FLT3LG might act as an immunoregulatory factor in cervical cancer.
Discussion
Recently, the expression and functions of FLT3LG in the TME have been reported.16,17 And It stimulates the differentiation and expansion of DCs by binding to FLT3.18 Furthermore, several studies demonstrated that the FLT3LG levels in serum could be used as a predictive target after neoadjuvant therapy in CRC.20,21 However, a few reports about FLT3LG are mainly about RCC. The effect of FLT3LG expression on cervical cancer prognosis has not been explored. This study investigated the role of FLT3LG in cervical cancer.
This study systematically analyzes the clinical value and expression lever of FLT3LG in CESC via comprehensive bioinformatics research. Our results demonstrated that poor prognosis was consistent with low-expression FLT3LG in CESC, which is compatible with our clinical specimens. Moreover, CESC with low FLT3LG expression exhibited poor clinicopathological characteristics. A multivariate, univariate, and ROC analysis of FLT3LG in cervical cancer patients also suggested that it was an extremely valuable predictive biomarker. Furthermore, our results also show that the expression of FLT3LG is closely related to the degree of infiltration of different immune cells, immunostimulators, immunoinhibitors, chemokines, and receptors in CESCs.
A major clinically relevant conclusion was that low expression of FLT3LG was related to poor survival. Decreased FLT3LG is the only independent prognostic factor for overall survival by multivariate Cox regression analysis. A nomogram prediction model was established to confirm the predictive effect of FLT3LG expression on prognosis. Hence, the low expression of FLT3LG may be a valuable biomarker in CESC patients. Additionally, FLT3LG was evaluated by ROC curve analysis for its potential to differentiate CESC patients from normal individuals, with an AUC of 0.82. Also, the AUC of FLT3LG was 0.811 based on our cohort, and the cut-off value of FLT3LG expression was 0.405.
Furthermore, after adjusting for standard clinical factors, FLT3LG appears to be an independent predictor of poor prognosis in CESC. According to a multivariate Cox regression analysis, low FLT3LG expression was an independent predictor of OS. To improve prognosis prediction, a nomogram prognosis map was constructed by combining FLT3LG with the T stage. According to the FLT3LG-related Cox model, OS was predicted at 0.725 (0.689–0.761). As shown in the calibration chart, the nomogram predictions associated with FLT3LG matched optimally with the observations of 1-, 3-, and 5-year OS probabilities. Using the Cox analysis and nomogram model, FLT3LG expression appears to be more predictive than other factors. Our model may provide a personalized score for each patient with CESC in this regard.
Additionally, the present study revealed that FLT3LG is significantly linked to the degree of immune infiltration in cervical cancer. There is evidence that infiltration of immune cells plays a vital role in cancer progression and development in the TME.32,33 In immune cell infiltration analysis, FLT3LG expression was positively associated with cytotoxic cells, T cells, Treg cells, active dendritic cells (aDCs), NK CD56dim B cells, Th1 cells, and CD8 T cells. There are two primary subsets of human NK cells, CD56 (bright) and CD56 (dim), which account for 10–15% of circulating lymphocytes. It has been considered that CD56 (bright) NK cells are immature NK cells. CD56 (bright) NK cells are highly productive and have low cytotoxicity.34–36 In particular, NK cells play a dual role in tumor formation. It is traditionally an immunosurveillance system and antitumor cell.37 Emerging studies have recently shown that CD56(bright) NK cells play a role in tumor development.38,39 In this study, NK CD56(dim) cells’ infiltration was strongly linked to FLT3LG expression.
Additionally, FLT3LG expression was strongly linked to immunostimulators, immunoinhibitors, chemokines, and receptors. Furthermore, this article also indicated the relationship between FLT3LG level and the marker of TIL in CESC. FLT3LG level was associated with M2 markers, including CD163 and MS4A4A. However, M1 markers, such as NOS2 and IRF5, had weakly correlation with FLT3LG level. Macrophages can further differentiate into M1 and M2 macrophages,40 and play a key role in proliferation,41 angiogenesis,42 invasion,43 metastasis,44 and immunity of tumor.45 Based on these findings, FLT3LG may be able to regulate TAM polarization.
Furthermore, FLT3LG expression was strongly associated with T-cell exhaustion markers (PD1, PD-L1, CTLA4, LAG3, TIM3, GZMB). ICIs are the primary immunotherapeutic strategy. It has been shown that PD-1/PDL-1 controls the function of TILs, making it one of the essential immune checkpoints. So far, anti-PD-1/PD-L1 has been widely used in various tumors, including cervical cancer.46,47 However, it is reported that nearly 85% of cancer patients have innate or acquired resistance to ICIs, which significantly limits their clinical application.9 Therefore, it is essential to improve the response of tumor cells to immune checkpoint inhibitors and cytokines. Merad et al48 demonstrate the limited response of anti-PD-L1 therapy in a murine melanoma model (B16). However, anti-PD-L1 treatment combined with FLT3LG infusions reduced tumor growth. As a result of these findings, it was suggested that targeting FLT3LG might enhance immunotherapy efficacy. In a word, FLT3LG played a valuable function in recruiting and modulating TILs in CESC. It deserves to continue investigating the molecular mechanism and role of FLT3LG in modulating the TME.
As we know, tumor cells are essential in tumor immune escape and immunotherapy. However, the relationship between the immune system and CESC has not been fully elaborated. Hence, the relationship between FLT3LG expression and cytotoxic cells, T cells, Treg cells, active dendritic cells (aDCs), NK CD56dim cells, B cells, Th1 cells, and CD8 T cells need to reveal. Given our findings and the above research reports, whether FLT3LG and those immune cells are involved in the immune escape in CESC still deserves further exploration.
However, this study has the following limitations. Firstly, the sample of this study is small. Therefore, the sample size should be expanded in future studies to obtain better reliability and representative of the results and hypotheses. Secondly, in vivo and in vitro experiments should also explore the function of FLT3LG in CESC and the regulatory mechanisms of FLT3LG in the CESC microenvironment. We will further validate the projected results via experiments in future studies.
Conclusion
This study first demonstrated that FLT3LG expression decreased in CESC, also related to poor prognosis based on various online databases and our cohort. Moreover, ROC and univariate and multivariate cox regression analysis demonstrated that FLT3LG was a critical predictive biomarker for cervical cancer patients. In addition, our result suggested that the low levels of FLT3LG would be a valuable biomarker for poor prognosis. What is more, FLT3LG significantly associated with immune infiltration. Therefore, this present study provides novel insights into understanding the critical function of FLT3LG. Hence, the low expression of FLT3LG may be a valuable biomarker in CESC patients linked with immune infiltration.
Patient Consent for Publication
The Hospital Ethics Committee of Fujian Provincial Maternity and Children’s Hospital, an affiliated hospital of Fujian Medical University, approved the study (2022KYLLR03050) and complied with the Declaration of Helsinki. And all individuals participating in this study signed written informed consent.
Acknowledgment
The authors thank the gynecological laboratory of Fujian Provincial Maternity and Children’s Hospital, an affiliated hospital of Fujian Medical University, for helping with specimen collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was funded by grants from the National Natural Science Foundation of China (Nos. 81772783, 81971475).
Disclosure
All authors report no competing interests in this work.
References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi:10.3322/caac.21262
2. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
3. Fokdal L, Sturdza A, Mazeron R, et al. Image guided adaptive brachytherapy with combined intracavitary and interstitial technique improves the therapeutic ratio in locally advanced cervical cancer: analysis from the retro embrace study. Radiother Oncol. 2016;120:434–440. doi:10.1016/j.radonc.2016.03.020
4. Rosen VM, Guerra I, McCormack M, et al. Systematic review and network meta-analysis of bevacizumab plus first-line topotecan-paclitaxel or cisplatin-paclitaxel versus non-bevacizumab-containing therapies in persistent, recurrent, or metastatic cervical cancer. Int J Gynecol Cancer. 2017;27:1237–1246. doi:10.1097/IGC.0000000000001000
5. Fontham ETH, Wolf AMD, Church TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70:321–346. doi:10.3322/caac.21628
6. Ott PA, Dotti G, Yee C, Goff SL. An update on adoptive T-cell therapy and neoantigen vaccines. Am Soc Clin Oncol Educ B. 2019;39:e70–e78. doi:10.1200/EDBK_238001
7. Martinez M, Moon EK. CAR T cells for solid tumors: new strategies for finding, infiltrating, and surviving in the tumor microenvironment. Front Immunol. 2019;10:128. doi:10.3389/fimmu.2019.00128
8. Robert C. A decade of immune-checkpoint inhibitors in cancer therapy. Nat Commun. 2020;11:3801. doi:10.1038/s41467-020-17670-y
9. Xiao Q, Nobre A, Piñeiro P, et al. Genetic and epigenetic biomarkers of immune checkpoint blockade response. J Clin Med. 2020;9(1):286. doi:10.3390/jcm9010286
10. Liu D, Jenkins RW, Sullivan RJ. Mechanisms of resistance to immune checkpoint blockade. Am J Clin Dermatol. 2019;20:41–54. doi:10.1007/s40257-018-0389-y
11. Salmon H, Idoyaga J, Rahman A, et al. Expansion and activation of CD103 + dendritic cell progenitors at the tumor site enhances tumor responses to therapeutic PD-L1 and BRAF inhibition. Immunity. 2016;44(4):924–938. doi:10.1016/j.immuni.2016.03.012
12. Hammerich L, Marron TU, Upadhyay R, et al. Systemic clinical tumor regressions and potentiation of PD1 blockade with in situ vaccination. Nat Med. 2019;25(5):814–824. doi:10.1038/s41591-019-0410-x
13. Levesque S, Le Naour J, Pietrocola F, et al. A synergistic triad of chemotherapy, immune checkpoint inhibitors, and caloric restriction mimetics eradicates tumors in mice. Oncoimmunology. 2019;8(11):e1657375. doi:10.1080/2162402X.2019.1657375
14. Liu P, Zhao L, Pol J, et al. Crizotinibinduced immunogenic cell death in non-small cell lung cancer. Nat Commun. 2019;10(1):1486. doi:10.1038/s41467-019-09415-3
15. Alley EW, Lopez J, Santoro A, et al. Clinical safety and activity of pembrolizumab in patients with malignant pleural mesothelioma (KEYNOTE-028): preliminary results from a non-randomised, open-label, phase 1b trial. Lancet Oncol. 2017;18(5):623–630. doi:10.1016/S1470-2045(17)30169-9
16. Borcoman E, Le Tourneau C. Keynote-158 study, FDA granted accelerated approval of pembrolizumab for the treatment of patients with advanced PD-L1-positive cervical cancer. Ann Transl Med. 2020;8:1611. doi:10.21037/atm-20-2656
17. Lisovsky M, Braun SE, Ge Y, et al. Flt3-ligand production by human bone marrow stromal cells. Leukemia. 1996;10:1012–1018.
18. Barry KC, Hsu J, Broz ML, et al. A natural killer-dendritic cell axis defines checkpoint therapy-responsive tumor microenvironments. Nat Med. 2018;24:1178–1191. doi:10.1038/s41591-018-0085-8
19. Anandasabapathy N, Feder R, Mollah S, et al. Classical Flt3Ldependent dendritic cells control immunity to protein vaccine. J Exp Med. 2014;211:1875–1891. doi:10.1084/jem.20131397
20. Durai V, Bagadia P, Briseno CG, et al. Altered compensatory cytokine signaling underlies the discrepancy between Flt3(-/-) and Flt3l (-/-) mice. J Exp Med. 2018;215:1417–1435. doi:10.1084/jem.20171784
21. Kalanxhi E, Meltzer S, Schou JV, et al. Systemic immune response induced by oxaliplatin-based neoadjuvant therapy favors survival without metastatic progression in high-risk rectal cancer. Br J Cancer. 2018;118(10):1322–1328. doi:10.1038/s41416-018-0085-y
22. Abrahamsson H, Jensen BV, Berven LL, et al. Antitumor immunity invoked by hepatic arterial infusion of first-line oxaliplatin predicts durable colorectal cancer control after liver metastasis ablation: 8–12 years of follow-up. Int J Cancer. 2020;146:2019–2026. doi:10.1002/ijc.32847
23. Greystoke A, O’Connor JP, Linton K, et al. Assessment of circulating biomarkers for potential pharmacodynamic utility in patients with lymphoma. Br J Cancer. 2011;104(4):719–725. doi:10.1038/sj.bjc.6606082
24. Wonder-Filipowicz A, Lyman SD, Gratwohl A, Tichelli A, Speck B, Nissen C. Flt3 ligand level reflects hematopoietic progenitor cell function in aplastic anemia and chemotherapy-induced bone marrow aplasia. Blood. 1996;88(12):4493–4499. doi:10.1182/blood.V88.12.4493.bloodjournal88124493
25. Maraskovsky E, Brasel K, Teepe M, et al. Dramatic increase in the numbers of functionally mature dendritic cells in FLT3 ligand-treated mice: multiple dendritic cell subpopulations identified. J Exp Med. 1996;184:1953–1962. doi:10.1084/jem.184.5.1953
26. Vivian J, Rao AA, Nothaft FA, et al. Toil enables reproducible, open source, big biomedical data analyses. Nat Biotechnol. 2017;35:314–316. doi:10.1038/nbt.3772
27. Li T, Fu J, Zeng Z, et al. TIMER2.0 for analysis of tumor-infiltrating immune cells. Nucleic Acids Res. 2020;48:W509–W514. doi:10.1093/nar/gkaa407
28. Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z. GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017;45(W1):W98–W102. doi:10.1093/nar/gkx247
29. Jianfang LIU, Lichtenberg T, Hoadley KA, et al. An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell. 2018;173(2):400–416. e11. doi:10.1016/j.cell.2018.02.052
30. Ru B, Wong CN, Tong Y, et al. TISIDB: an integrated repository portal for tumor-immune system interactions. Bioinformatics. 2019;35(20):4200–4202. doi:10.1093/bioinformatics/btz210
31. Chen L, Dong B, Zhang Q, et al. HR-HPV viral load quality detection provide more accurate prediction for residual lesions after treatment: a prospective cohort study in patients with high-grade squamous lesions or worse. Medical Oncology. 2020;37(5):1–9. doi:10.1007/s12032-020-01363-z
32. Chen L, Dong B, Gao H, et al. HPV-16 E2/E6 and POU5F1B as biomarkers to determine cervical high-grade squamous lesions and more. J Inflamm Res. 2020;13:813–821. doi:10.2147/JIR.S278911
33. Curigliano G. Gyneco-oncological genomics and emerging biomarkers for cancer treatment with immune-checkpoint inhibitors. Semin Cancer Biol. 2018;52(Pt 2):253–258. doi:10.1016/j.semcancer.2018.05.004
34. Klauschen F, Müller K-R, Binder A, et al. Scoring of tumor-infifiltrating lymphocytes: from visual estimation to machine learning. Semin Cancer Biol. 2018;52(Pt 2):151–157. doi:10.1016/j.semcancer.2018.07.001
35. Sanchez-Correa B, Campos C, Pera A, et al. Natural killer cell immunosenescence in acute myeloid leukemia patients: new targets for immunotherapeutic strategies? Cancer Immunol Immunother. 2016;65:453–463. doi:10.1007/s00262-015-1720-6
36. Montaldo E, Vacca P, Moretta L, Mingari MC. Development of human natural killer cells and other innate lymphoid cells. Semin Immunol. 2014;26:107–113. doi:10.1016/j.smim.2014.01.006
37. Michel T, Poli A, Cuapio A, et al. Human CD56bright NK cells: an update. J Immunol. 2016;196:2923–2931. doi:10.4049/jimmunol.1502570
38. Klein E, Vánky F, Vose BM. Natural killer and tumor recognizing lymphocyte activity in tumor patients. Haematologica. 1978;12:107–112.
39. Bruno A, Bassani B, D’Urso DG, et al. Angiogenin and the MMP9-TIMP2 axis are up-regulated in proangiogenic, decidual NK-like cells from patients with colorectal cancer. FASEB J. 2018;32:5365–5377. doi:10.1096/fj.201701103R
40. Poli A, Michel T, Thérésine M, Andrès E, Hentges F, Zimmer J. CD56bright natural killer (NK) cells: an important NK cell subset. Immunology. 2009;126:458–465. doi:10.1111/j.1365-2567.2008.03027.x
41. Jayasingam SD, Citartan M, Thang TH, Mat Zin AA, Ang KC, Ch’ng ES. Evaluating the polarization of tumor-associated macrophages into M1 and M2 phenotypes in human cancer tissue: technicalities and challenges in routine clinical practice. Front Oncol. 2019;9:1512. doi:10.3389/fonc.2019.01512
42. Su C, Jia S, Liu H. Immunolocalization of CD163+ tumorassociated macrophages and symmetric proliferation of Ki-67 as biomarkers to differentiate new different grades of laryngeal dysplasia. Am J Clin Pathol. 2017;149(1):8–16. doi:10.1093/ajcp/aqx107
43. Sammarco G, Gadaleta CD, Zuccalà V, et al. Tumor-associated macrophages and mast cells positive to tryptase are correlated with angiogenesis in surgically-treated gastric cancer patients. Int J Mol Sci. 2018;19:19.
44. Zhang D, Qiu X, Li J, Zheng S, Li L, Zhao H. TGF-β secreted by tumor-associated macrophages promotes proliferation and invasion of colorectal cancer via miR-34a-VEGF axis. Cell Cycle. 2018;17(24):2766–2778. doi:10.1080/15384101.2018.1556064
45. Song W, Mazzieri R, Yang T, Lobe GC. Translational significance for tumor metastasis of tumor-associated macrophages and epithelialmesenchymal transition. Front Immunol. 2017;8:1106. doi:10.3389/fimmu.2017.01106
46. Wynn TA, Chawla A, Pollard JW. Macrophage biology in development, homeostasis, and disease. Nature. 2013;496(7446):445–455. doi:10.1038/nature12034
47. Lorusso D. Role of immune checkpoint inhibitors in cervical cancer: from preclinical to clinical data. Cancers. 2021;13(9):2089.
48. Rotman J, Otter L, Bleeker M, et al. PD-L1 and PD-L2 expression in cervical cancer: regulation and biomarker potential. Front Immunol. 2020;11:11. doi:10.3389/fimmu.2020.00011
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







