Back to Journals » Clinical Ophthalmology » Volume 15
Long-term Surgical Outcomes of Phacoemulsification with Endoscopic Cyclophotocoagulation vs Phacoemulsification with Trabeculectomy and Mitomycin in Cataract and Glaucoma Patients
Authors A Bakr M, K Al-Mutairi N
Received 24 May 2021
Accepted for publication 20 July 2021
Published 24 August 2021 Volume 2021:15 Pages 3573—3580
DOI https://doi.org/10.2147/OPTH.S320092
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Medhat A Bakr,1 Naif K Al-Mutairi2
1Immam Abdulrahman Bin Faisal University, King Fahd University Hospital, Ophthalmology Department (Glaucoma Section), Al Khobar, Eastern Province, Kingdom of Saudi Arabia; 2Jeddah Eye Hospital, Jeddah, Kingdom of Saudi Arabia
Correspondence: Medhat A Bakr
King Fahd University Hospital, Immam Abdulrahman Bin Faisal University, Alaqrabia, Al Khobar, Kingdom of Saudi Arabia
Tel +966559753252
Email [email protected]
Purpose: To evaluate the long-term surgical outcomes of endoscopic cyclophotocoagulation (ECP) after four years follow-up in cataract and glaucoma patients that needed combined phacoemulsification and ECP (phaco-ECP) in comparison to combined phacoemulsification with trabeculectomy (phaco-trabeculectomy) with mitomycin C (MMC).
Patients and Methods: Retrospective case–control study of 34 patients (34 eyes) with glaucoma who underwent phaco-ECP compared with phaco-trabeculectomy in tertiary eye specialist hospital in Saudi Arabia from 2010 to 2012. Participants were enrolled in two groups; ECP and trabeculectomy with MMC when combined with phacoemulsification. Success is defined as complete success when the IOP ≤ 21 mmHg without medication, qualified success when the IOP ≤ 21 mmHg with aid of topical medication.
Results: Mean IOP decreased from 25.76 SD ± 8.227 to 15.24 SD ± 7.049 at last visit in phaco-trabeculectomy group and from 21.47 SD ± 4.215 to 12.88 SD ± 3.480 in phaco-ECP group. Mean medication use reduced from 2.89 SD ± 0.3 preoperatively to 1.50 SD ± 1.1 postoperatively (P< 0.001) in phaco-trabeculectomy group. It reduced in phaco-ECP group from 2.24 SD ± 0.8 preoperatively to 2.00 SD ± 0.9 postoperatively, 35.3% of phaco-trabeculectomy group developed vision-threatening complications while 0% in phaco-ECP group (P< 0.001), 29.4% in phaco-trabeculectomy group required second surgical intervention compared to 17.6% in phaco-ECP group. In phaco-trabeculectomy group, 29.4% reached complete success, meanwhile in phaco-ECP group, 64.7% reached qualified success (P=0.026).
Conclusion: ECP illustrates significant reduction of IOP and less postoperative complications if associated with phacoemulsification. Furthermore, it is safe and effective as a primary procedure alternative to combined cataract and trabeculectomy surgery for glaucoma patients having cataract and requiring surgical intervention.
Keywords: cataract, extraction, phacoemulsification, trabeculectomy, glaucoma; ECP Endoscopic cyclophotocoagulation
Introduction
Visual impairment due to cataract and glaucoma is a major health-care issue, where glaucoma is a leading cause of irreversible blindness.1,2 Studies predicted that the total global prevalence of primary open-angle glaucoma (POAG) was 3.54% among adults 40–80 years old and the number of people with glaucoma worldwide may increase to 111.8 million in 2040, disproportionally affecting people residing in Asia and Africa.1 According to the World Health Organization’s (WHO) 2010 global data on visual impairment, globally the number of visually impaired people of all ages was estimated to be 285 million, of which 39 million are legally blind. The data of WHO demonstrates that the major causes of visual impairment are uncorrected refractive errors (43%) and cataract (33%).3
The peripheral iridectomy described by German physician von Graefe in 1856 was the first surgical attempt to enhance aqueous egress through normal physiologic channels, but it certainly was not the last.4 Ironically, the Cairns trabeculectomy (1968) was initially conceived as a method of restoring physiologic outflow by removing the juxtacanalicular trabecular meshwork, but it ultimately became a sclerokeratectomy procedure that reduced intraocular pressure (IOP) by permitting suprascleral fluid to escape and forming a bleb.5
Endoscopic cyclophotocoagulation (ECP) is an endoscope-assisted technique that utilizes laser energy to destroy ciliary body epithelium and reduces the production of aqueous humor, thereby, lowering the IOP.6 Uram, in 1995, applied ECP combined with phacoemulsification in 10 patients with refractory open angle glaucoma and cataract.7 The results were impressive, showing a significant decrease of mean IOP.7 It minimized the disadvantages of conventional procedures and maximized the advantages of ablating the ciliary body epithelium to reduce the IOP.3,7 This new therapeutic modality ablated the ciliary epithelium by direct visualization of the ciliary processes with diode laser photocoagulation in precise titration of laser delivery to the ciliary processes,8 that can effectively manage the intractable glaucoma.9 It is a versatile micro-invasive glaucoma surgery (MIGS) procedure that uniquely lowers IOP through the reduction of aqueous humor production.
While transscleral ciliary body ablation is a long-established treatment for refractory glaucoma, ECP accomplishes this task in a more controlled and predictable fashion to achieve significant IOP reduction while maintaining a high safety profile.10 ECP also offers the benefits of shorter operative times, rapid vision recovery, lower risk profiles, and ability to combine easily with cataract surgery by sparing the conjunctiva for more invasive surgical options in the future.11 The instrument combines a light source endo-laser, and video endoscope in a 20-gauge single optic fiber probe. In addition, a laser is applied to the ciliary process in direct visualization until the ciliary process is shrunk and blanched or even exploded, which is not targeted. The reports of the efficacy of this procedure are encouraging and are associated with less postoperative complications when compared to the traditional transscleral methods.12 In this context this study examines the long-term surgical outcome of ECP to explore its advantages over the traditional procedures.
Materials and Methods
A retrospective case–control study was conducted at Dhahran eye specialist hospital, Dhahran city, Kingdom of Saudi Arabia between 2010 and 2012, in accordance with Declaration of Helsinki and after approval from the committee of research and ethics in Imam Abdurrahman Bin Faisal University in Saudi Arabia and Dhahran Eye Specialist Hospital. For retrospective evaluation of medical records, permission to use dataset records and patient information was obtained from dataset owner (Dhahran Eye Specialist Hospital) assuring data confidentiality and presented to IRB prior to study approval.
The study included total of 34 patients (34 eyes) with glaucoma who underwent (i) phaco-endoscopic photocoagulation (ECP) with phacoemulsification and (ii) trabeculectomy combined with phacoemulsification from 2010 to 2012, and operated by a single surgeon (MB) in a tertiary eye specialist hospital. The sample size was calculated using “RaoSoft” calculator. Medical files of all patients were reviewed. Inclusion criteria included the following: adult patients aged between 18 and 75 years diagnosed with primary or secondary open-angle glaucoma, chronic primary closed-angle glaucoma, not reaching target IOP (<21 mmHg) despite maximum tolerable medical and laser treatment, those who underwent ECP combined with phacoemulsification and those who underwent trabeculectomy with MMC combined with phacoemulsification, without previous glaucoma surgery, and compliant patients regarding follow-up (regularly following in OPD for duration of four years postoperatively). Exclusion criteria included the following: patients diagnosed with congenital, uveitic, neovascular, and/or traumatic glaucoma, and those with complicated cataract surgery or other ocular surgery like pars plana vitrectomy and previous glaucoma surgery. Patients were classified into two groups: first group was trabeculectomy combined phacoemulsification (phaco-trabeculectomy) and second one was ECP combined with phacoemulsification (phaco-ECP).
Trabeculectomy Surgical Technique
Limbal based peritomy approach with superficial scleral flap was performed and MMC (0.4%) was applied for two minutes. After washing MMC, trabeculectomy was carried out followed by surgical iridectomy and scleral flap was sutured with 10/0 nylon sutures.
ECP Surgical Technique
After phacoemulsification, two opposite paracentesis were made and ECP laser probe was introduced through it with presence of viscoelastic solution. Under direct visualization laser was applied to the ciliary body process and cut at the end of treatment when tissue color changed to white and the shrink process was repeated at 270°.
The patients’ demographic data included age and sex. Whereas, preoperative data included preoperative diagnosis, visual acuity, IOP taken at the visit when decision for intervention was taken, laterality, the number of preoperative medications needed and whether the patient had any laser peripheral iridectomy or selective laser trabeculoplasty. Postoperative data included IOP on the first postoperative month, then at the second, fourth, and sixth months, and later on at first, second, third, and fourth postoperative years. Success after trabeculectomy surgery was judged based on the World Glaucoma Association's guidelines on design and reporting of glaucoma surgical trials.13 Results were divided into three categories. Complete success was considered in cases where the IOP was equal or less than 21 mmHg, without antiglaucoma drops. Qualified success was considered if IOP was ≤21 mmHg on antiglaucoma drops. Failure was considered if the IOP was >21 mmHg on at least two visits despite maximum medical therapy or if further glaucoma surgery was required. The data regarding medication were collected as preoperative medications which is the number of medications patient used at the time when the decision for surgery need was taken. The last medication referred to the number of medications patient was using in last visit (four years postoperatively).
Serious postoperative complications (eg, endophthalmitis, choroidal effusion, blebitis, etc) were documented during the period of the study as a safety parameter for each surgery.
Statistical Analysis
All categorical data were represented by frequency with percentage. Continuous data were presented by mean with standard deviation. Independent t test was used to test the significant difference between the two groups, related to continuous variables. Chi-squared and Fisher'sexact tests were used for categorical variables. The analysis was performed using SPSS 21.0 version. A P-value of <0.05 was considered significant.
Results
A total of 34 consecutive eyes of 34 patients (21 males and 13 females) were distributed to the two surgical groups. Of these eyes, 17 were with trabeculectomy combined with phacoemulsification and mitomycin and 17 were with ECP combined with phacoemulsification. The mean age of subjects’ who underwent trabeculectomy was 58.35 (SD ±15.3) years and those having ECP had a mean age of 62.88 (SD ±10.4) years. The two groups were dominated by male subjects with a percentage of 58.8%, and 64.7% for trabeculectomy, and ECP respectively. The difference among them was not statistically significant based on age, gender, and site of surgery (Table 1).
 |
Table 1 Demographic Details of Enrolled Patients |
Mean IOP during the four-year study period was monitored for the two surgical groups (Table 2,Table 3). In the ECP group (n=17), mean preoperative IOP decreased from preoperative baseline (21.47 mmHg ±4.215 SD; at one year 15.47 mmHg ±5.363 SD; at two years 14.35 mmHg ±4.808 SD; at three years 12.41 mmHg ±3.001 SD; at four years 12.08 mmHG ±3.480 SD). Similarly in the trabeculectomy group (n=17), mean preoperative IOP decreased from baseline (25.76 mmHg ±8.227 SD; at one year 10.53 mmHg ±5.724 SD; at two years 12.76 mmHg ±4.855 SD; at three years 11.53 mmHg ±5.088 SD; at four years 15.24 mmHg ±7.049 SD). The mean IOP of the preoperative cases among two groups demonstrates statistical significance difference at the preoperative baseline (P=0.003).
 |
Table 2 Intraocular Pressure (IOP) Among Both Groups Across the Study Period |
Among the two surgical groups the mean IOP dropped dramatically after surgery and the lowest among them was observed in the trabeculectomy group in the first month after surgery with a mean of 9.06 mmHg (SD ±4.100), which was 25.76 mmHg (SD ±8.227) before surgery with 64.9% reduction. This was compared with ECP with mean 13.06 (SD ±3.864) in the first month after surgery and was observed statistically significant (P=0.006) at the first month. Mean IOP of the trabeculectomy group keeps maintaining the lowest position from the first month after surgery to the third year of follow-up and the mean value rose to 15.24 (SD ±7.049) in the fourth year. But the mean IOP of the ECP group was slightly higher in the beginning to the sixth month of surgery, then started dropping gradually and was observed to be the lowest among the groups in the fourth year of follow-up with a mean of 12.08 (SD ±3.480) compared to the trabeculectomy group 15.24 (SD ±7.049), respectively. However, there was no statistically significant difference among the groups during the second year, until the fourth year. The rate of IOP reduction at the end of study period (four years) was 40.83% and 30.26% for trabeculectomy and ECP groups, respectively (Figure 1).
 |
Figure 1 Mean IOP among the two groups over four years. |
The average number of medications needed by the two different types of surgical procedures were analyzed (Table 3) and significant difference between medication use both pre and post operatively in trabeculectomy group was observed (P <0.001), demonstrated the lowest average number of medications required postoperatively 1.90 (SD ± 1.1) than preoperative 2.89 (SD ± 0.3), while the number of postoperative medications for ECP group did not show any statistically significant difference compared to the number of medications used preoperatively (P =0.361). The number of preoperative and postoperative medication usage among the groups showed statistically significant difference (P =0.007) preoperatively and (P = 0.018) postoperatively (Table 4).
 |
Table 3 Average Frequency of Medications Required Pre- and Postoperatively |
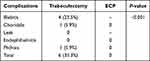 |
Table 4 Observed Sight-threatening Complications |
With regard to the need for further surgical interventions, the ECP group showed a lower number of further surgical operations ie, only three cases (two Ahmed glaucoma valve implantation and one trabeculectomy with MMC) (17.6%) required further intervention. Meanwhile, in the trabeculectomy group five cases needed further surgery to achieve reasonable IOP (three had redo trabeculectomy with MMC, one had Ahmed glaucoma valve implantation, and one had bleb revision) (29.4%). However, the difference was insignificant (P=0.418) (Table 5).
 |
Table 5 Further Surgical Interventions |
For the success rate, the trabeculectomy group showed higher complete success rate ie, five eyes (29.4%) with significant reduction in IOP and medication usage compared to the ECP group that had no case labeled as complete success. However, ECP group showed a higher rate of qualified success ie, 11 eyes (64.7%) compared to trabeculectomy group which had five eyes (29.4%) only (Table 6). Failure was higher among trabeculectomy group ie, seven eyes (41.2%) compared to the ECP group which had six eyes (35.3%). Total success rate was 58.8% in trabeculectomy group and 64.7% in the ECP group but it was statistically insignificant (P=0.724) (Figure 2).
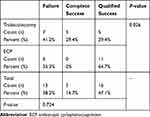 |
Table 6 Success and Failure Rate Between Two Groups |
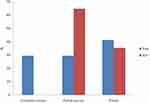 |
Figure 2 Displaying the success and failure between both groups. |
The overall difference in the IOP reduction between the two groups was found statistically significant until the time point of postoperative one year, also statistically significant association was observed in reduced medication usage both pre- and postoperatively. In terms of sight-threatening complications significant difference was observed between two groups (P<0.001). However, no difference was observed in both groups in terms of surgical interventions.
Discussion
The study focused on surgical outcomes of ECP and it demonstrated the advantages of the procedure in the management of cases with cataract and glaucoma by comparing combined ECP with phacoemulsification and trabeculectomy with phacoemulsification in regard to IOP reduction, topical medications needed, complications, and success or failure rate at the four-year follow-up period.
Concerning IOP, irrespective of the different procedures, it was observed that the IOP dropped significantly in the first month until one year of follow-up for both procedures. ECP provided a steady mean value without much fluctuation of IOP. Subsequently, the drop in mean IOP of the ECP group was observed and maintained until the end of the study period. Yip et al10 also observed an overall success rate based on IOP reduction of 20%. This was compatible with the prospective study of Francis et al14 who found statistically significant reduction of IOP in combined phaco-ECP group after two years of follow-up.
The study subjects were of different ages in both groups. As age advances the condition of cataract and glaucoma intensifies and in our study population, the ECP group had the highest mean age compared to the trabeculectomy group. This may be the reason why the IOP was on the higher side when compared to the trabeculectomy group until the sixth month of follow-up.
A study by Lindfield et al15 showed statistically significant reduction in the mean IOP at 18 and 24 months with difference reaching up to 7.1 from baseline. The Kahook et al16 study on 40 eyes with six months follow-up documented reduction in IOP that was statistically significant for combined phacoemulsification with ECP applied to 180° and 360° and the reduction was more among the 360° approach. The 24-month cohort study by Yip et al10 on 29 eyes showed a statistically significant IOP reduction at 18 months, however, this significant reduction was not observed at 24 months. Lima et al17 documented result from 368 eyes with follow-up exceeding two years showed statistically significant reduction. They reported that 46% reduction of IOP from baseline was achieved at all time points of mean follow-up during 35.2 months and their explanation of that significant amount of reduction is related to the degree of pigmentation. Siegel et al18 studied 261 eyes that underwent combined phaco-ECP and 52 eyes that underwent phacoemulsification alone in period of 36 months also showed a reduction in IOP among the phaco-ECP group.
The use of medications was also observed, and statistically significant reduction in medication usage was observed between two groups both preoperatively (P<0.007) and postoperatively (P=0.018). While the ECP group does not show significant reduction in number of medications preoperatively and postoperatively that is comparable to, Lindfield et al15 and Morales et al19 who observed no statistically significant changes in number of medications required and they concluded that the ECP could reduce the medication needed but patients may not control the IOP with procedure alone. Contrarily, Lima et al17 and Siegel et al18 found a statistically significant reduction in number of medications.
Another interesting observation regarding sight-threatening complications that not even a single postoperative sight-threatening complication was found during the four-year study period. Lima et al17 and Siegel et al18 also reported that the surgical complications were low and all were mild non-vision-threatening complications eg, anterior chamber reaction and mild corneal edema. This was also mentioned by Rathi and Radcliffe20 in their literature review, they concluded that phaco-ECP has a minimal side effect profile, and risks are limited to those usual with post-phacoemulsification procedures.
The complete success as well as the failure rate was higher among the trabeculectomy group, while in ECP group none of the subjects meet criteria for complete success but higher percent met qualified success. This was compatible with Morales et al19 study, who reported absolute success was achieved only in 11.9% participants, while the qualified success was achieved in 72.3% participants in their study. Siegel et al18 reported that phaco-ECP group had higher rate of either qualified success or complete success compared to group that underwent phacoemulsification alone at the 18 month follow-up period.
Regarding the phaco-trabeculectomy group, a 40% reduction of IOP from baseline was found after four years of follow-up. While Jung et al8 reported only 20% of reduction. Shingleton et al21 also reported reduction of IOP and number of medications for group of phaco-trabeculectomy after seven years of follow-up period in pseudo-exfoliation patients. The reduction in mean postoperative IOP was greater in eyes with a higher mean preoperative IOP. Still 13.8% of eyes required subsequent laser trabeculoplasty, glaucoma surgery, or both.
A high rate of sight-threatening complication was found in the phaco-trabeculectomy group, like blebitis, phthisis bulbi, and choridalis which might have occurred due to reduction in IOP and fistula nature of trabeculectomy. This was compatible with Funnell's22 finding as he reported delayed bleb leaks were seen in seven eyes (18.4%) of the phaco-trabeculectomy group.
Conclusion
ECP illustrates significant reduction of IOP and fewer postoperative complications if associated with phacoemulsification with statistically significant reduction in medication usage. Moreover, it is safe and effective as a primary procedure alternative to combined cataract and trabeculectomy surgery for glaucoma patients suffering from cataract and requiring surgical intervention.
Abbreviations
ECP, endoscopic cyclophotocoagulation; MMC, mitomycin C; POAG, primary open-angle glaucoma; WHO World Health Organization; IOP, intraocular pressure; MIGS, micro-invasive glaucoma surgery.
Acknowledgments
The author is very thankful to all the associated personnel in any reference that contributed in/for the purpose of this research.
Disclosure
The authors reports no conflict of interest in this work.
References
1. Tham Y, Li X, Wong T, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
2. Yang Y, Zhong J, Dun Z, et al. Comparison of efficacy between endoscopic cyclophotocoagulation and alternative surgeries in refractory glaucoma. Medicine. 2015;94(39):e1651. doi:10.1097/md.0000000000001651
3. Seibold L, SooHoo J, Kahook M. Endoscopic cyclophotocoagulation. Middle East Afr J Ophthalmol. 2015;22(1):18. doi:10.4103/0974-9233.148344
4. Wollensak G, Muchamedjarow F, Iomdina E. Early German-Russian cooperation in ophthalmology. Russ Ophthalmol J. 110103.
5. Razeghinejad MR, Spaeth GL. A history of the surgical management of glaucoma. Optom Vis Sci. 2011;88(1):e39–e47. doi:10.1097/opx.0b013e3181fe2226
6. Murthy G, Murthy P, Murthy K, et al. A study of the efficacy of endoscopic cyclophotocoagulation for the treatment of refractory glaucomas. Indian J Ophthalmol. 2009;57(2):127. doi:10.4103/0301-4738.45502
7. Uram M. Combined phacoemulsification, endoscopic ciliary process photocoagulation, and intraocular lens implantation in glaucoma management. Ophthalmic Surg. 1995;26:346–352. doi:10.3928/1542-8877-19950701-17
8. Jung JL, Isida-Llerandi CG, Lazcano-Gomez G, SooHoo JR, Kahook MY. Intraocular pressure control after trabeculectomy, phacotrabeculectomy and phacoemulsification in a Hispanic population. J Curr Glaucoma Pract. 2014;8(2):67–74. doi:10.5005/jp-journals-10008-1164
9. Gayton J, Van Der Karr M, Sanders V. Combined cataract and glaucoma surgery: trabeculectomy versus endoscopic laser cycloablation. J Cataract Refract Surg. 1999;25(9):1214–1219. doi:10.1016/s0886-3350(99)00141-8
10. Yip L, Yong S, Earnest A, et al. Endoscopic cyclophotocoagulation for the treatment of glaucoma: an Asian experience. Clin Exp Ophthalmol. 2009;37(7):692–697. doi:10.1111/j.1442-9071.2009.02120.x
11. Iordanous Y, Kent J, Hutnik C, et al. Projected cost comparison of trabectome, istent, and endoscopic cyclophotocoagulation versus glaucoma medication in the ontario health insurance plan. J Glaucoma. 2014;23(2):e112–e118. doi:10.1097/ijg.0b013e31829d9bc7
12. Kaplowitz K, Kuei A, Klenofsky B, et al. The use of endoscopic cyclophotocoagulation for moderate to advanced glaucoma. Acta Ophthalmol. 2015;93(5):395–401. doi:10.1111/aos.12529
13. Heuer DK, Barton K, Grehn F, et al. Consensus on definition of success. In: Shaarway T, Sherwood M, Grehn F, editors. Guidelines on Design and Reporting of Glaucoma Surgical Trials: World Glaucoma Association. Amsterdam, The Netherlands: Kluger Publications; 2009:15–24.
14. Francis B, Berke S, Dustin L, et al. Endoscopic cyclophotocoagulation combined with phacoemulsification versus phacoemulsification alone in medically controlled glaucoma. J Cataract Refract Surg. 2014;40(8):1313–1321. doi:10.1016/j.jcrs.2014.06.021
15. Lindfield D, Ritchie R, Griffiths M. ‘Phaco–ECP’: combined endoscopic cyclophotocoagulation and cataract surgery to augment medical control of glaucoma. BMJ Open. 2012;2(3):e000578. doi:10.1136/bmjopen-2011-000578
16. Kahook M, Lathrop K, Noecker R. One-site versus two-site endoscopic cyclophotocoagulation. J Glaucoma. 2007;16(6):527–530. doi:10.1097/ijg.0b013e3180575215
17. Lima F, Carvalho D, Ávila M. Facoemulsificação e ciclofotocoagulação endoscópica como tratamento primário para catarata e glaucoma coexistentes. Arq Bras Oftalmol. 2010;73(5):419–422. doi:10.1590/s0004-27492010000500006
18. Siegel MJ, Boling WS, Faridi OS, et al. Combined endoscopic cyclophotocoagulation and phacoemulsification versus phacoemulsification alone in the treatment of mild to moderate glaucoma. Clin Exp Ophthalmol. 2015;43(6):531–539. doi:10.1111/ceo.12510
19. Morales J, Al Qahtani M, Khandekar R, et al. Intraocular pressure following phacoemulsification and endoscopic cyclophotocoagulation for advanced glaucoma. J Glaucoma. 2015;24(6):e157–e162. doi:10.1097/ijg.0000000000000228
20. Rathi S, Radcliffe N. Combined endocyclophotocoagulation and phacoemulsification in the management of moderate glaucoma. Surv Ophthalmol. 2017;62(5):712–715. doi:10.1016/j.survophthal.2017.01.011
21. Shingleton B, Wooler K, Bourne C, et al. Combined cataract and trabeculectomy surgery in eyes with pseudoexfoliation glaucoma. J Cataract Refract Surg. 2011;37(11):1961–1970. doi:10.1016/j.jcrs.2011.05.036
22. Funnell C. Combined cataract and glaucoma surgery with mitomycin C: phacoemulsification-trabeculectomy compared to phacoemulsification-deep sclerectomy. Br J Ophthalmol. 2005;89(6):694–698. doi:10.1136/bjo.2004.055319
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
