Back to Journals » Clinical Epidemiology » Volume 13
Long-Term Risk of Skin Cancer and Lymphoma in Users of Topical Tacrolimus and Pimecrolimus: Final Results from the Extension of the Cohort Study Protopic Joint European Longitudinal Lymphoma and Skin Cancer Evaluation (JOELLE)
Authors Arana A, Pottegård A , Kuiper JG , Booth H, Reutfors J , Calingaert B , Lund LC, Crellin E , Schmitt-Egenolf M , Kaye JA , Gembert K, Rothman KJ, Kieler H, Dedman D , Houben E , Gutiérrez L , Hallas J , Perez-Gutthann S
Received 7 September 2021
Accepted for publication 6 December 2021
Published 29 December 2021 Volume 2021:13 Pages 1141—1153
DOI https://doi.org/10.2147/CLEP.S331287
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Irene Petersen
Alejandro Arana,1 Anton Pottegård,2 Josephina G Kuiper,3 Helen Booth,4 Johan Reutfors,5 Brian Calingaert,6 Lars Christian Lund,2 Elizabeth Crellin,4 Marcus Schmitt-Egenolf,5,7 James A Kaye,8 Karin Gembert,5 Kenneth J Rothman,8 Helle Kieler,5 Daniel Dedman,4 Eline Houben,3 Lia Gutiérrez,1 Jesper Hallas,2 Susana Perez-Gutthann1
1Department of Epidemiology, RTI Health Solutions, Barcelona, 08028, Spain; 2Clinical Pharmacology, Pharmacy and Environmental Medicine, Institute of Public Health, University of Southern Denmark, Odense C, 5000, Denmark; 3The PHARMO Institute, Utrecht, 3528 AE, the Netherlands; 4Clinical Practice Research Datalink (CPRD), The Medicines and Healthcare Products Regulatory Agency, London, E14 4PU, UK; 5Centre for Pharmacoepidemiology, Karolinska Institutet, Solna, 171 76, Stockholm, Sweden; 6Department of Epidemiology, RTI Health Solutions, Research Triangle Park, NC, 27709-2194, USA; 7Department of Public Health and Clinical Medicine, Umeå University, Umeå, 901 87, Sweden; 8Department of Epidemiology, RTI Health Solutions, Waltham, MA, 02451-1623, USA
Correspondence: Alejandro Arana
Department of Epidemiology, RTI Health Solutions, Av. Diagonal 605, 9-1, Barcelona, 08028, Spain
Tel +34 93 362 2805
Fax +34 93 414 2610
Email [email protected]
Purpose: Evidence is insufficient to infer whether topical calcineurin inhibitors (TCIs; tacrolimus and pimecrolimus) cause malignancy. The study objective was to estimate the long-term risk of skin cancer and lymphoma associated with topical TCI use in adults and children, separately.
Patients and Methods: A cohort study in Denmark, Sweden, UK, and the Netherlands was conducted. Adjusted incidence rate ratios (IRRs) and 95% confidence intervals (CIs) were calculated for nonmelanoma skin cancer (NMSC), melanoma, cutaneous T-cell lymphoma (CTCL), non-Hodgkin lymphoma (NHL) excluding CTCL, and Hodgkin lymphoma (HL) in new users of TCIs versus users of moderate/high-potency topical corticosteroids.
Results: The study included 126,908/61,841 adults and 32,605/27,961 children initiating treatment with tacrolimus/pimecrolimus, respectively. Follow-up was ≥ 10 years for 19% of adults and 32% of children. Incidence rate ratios and (95% confidence intervals) for tacrolimus versus corticosteroid users in adults were < 1 for melanoma, non-Hodgkin lymphoma, and Hodgkin lymphoma; and 1.80 (1.25– 2.58) for cutaneous T-cell lymphoma. For pimecrolimus, IRRs in adults were < 1 for non-Hodgkin lymphoma, cutaneous T-cell lymphoma, and Hodgkin’s lymphoma; and 1.21 (1.03– 1.41) for melanoma; and 1.28 (1.20– 1.35) for nonmelanoma skin cancer. In children, results were inconclusive due to few events. In adults, incidence rate ratios ≥ 5 years after first topical calcineurin inhibitor exposure were not higher than in overall analyses.
Conclusion: Overall, we found little evidence associating use of topical calcineurin inhibitors with skin cancer and lymphoma; confounding by indication, surveillance bias, and reverse causation may have influenced these results. Even if causal, the public health impact of these excess risks would be low and confined to the first years of exposure.
Keywords: tacrolimus, pimecrolimus, cutaneous T-cell lymphoma, malignant melanoma, non-melanoma skin cancer, database study
Introduction
According to approved labeling, topical tacrolimus is indicated for the treatment of moderate to severe atopic dermatitis (AD), and topical pimecrolimus, for the treatment of mild to moderate AD. It is known that they are used off-label, too, but the extent of its use has not been investigated.1 Safety data from systemic use of immunosuppressants in patients with organ transplants, from animal studies, and from case reports raised initial concerns about a potential increase in the risk of lymphoma and skin cancer associated with the use of topical calcineurin inhibitors (TCIs), especially in children. The epidemiologic literature presents insufficient evidence to infer whether TCIs cause malignancy.2–5 Differentiating the effects of the medication itself from the risks associated with AD or severe AD is inherently difficult.6,7 Furthermore, reverse causation is a concern because patients in early stages of certain skin malignancies, particularly cutaneous T-cell lymphoma (CTCL), may present clinical manifestations resembling AD and therefore may be treated with the study medications.
Given the long potential latency for cancer development, postmarketing studies with long follow-up are necessary to determine whether there is an association between TCIs and cancer. The European Medicines Agency requested a European study with sufficient follow-up to evaluate long-term risk of cancer. The objective of the JOELLE extension study was to estimate the long-term risks of melanoma, nonmelanoma skin cancer (NMSC), CTCL, non-Hodgkin lymphoma (NHL) (excluding CTCL), and Hodgkin lymphoma (HL) in adults and children.
Patients and Methods
This cohort study included data from the Clinical Practice Research Datalink (United Kingdom) (UK-CPRD) (2002–2017), the PHARMO Database Network (the Netherlands) (NL-PHARMO) (2002–2017), the Danish health databases (Denmark) (2002–2016), and the Swedish health databases (Sweden) (2006–2015).
Within each data source, eligible patients were required to have ≥12 months of continuous database enrollment before the first recorded prescription (new users) within the study period (except for children 0–12 months of age, who were eligible for inclusion with no required period of prior continuous enrollment). Patients with documented history of skin cancer or lymphoma before cohort entry were excluded. New users of topical tacrolimus and new users of topical pimecrolimus were classified into four groups according to age (children <18 years and adults ≥18 years) and TCI exposure (tacrolimus or pimecrolimus). A comparative cohort of users of moderate- to high-potency corticosteroids was matched to each of the four TCI-exposed cohorts. The corticosteroid comparison cohorts included (i) patients with AD diagnosis with a prescription for topical corticosteroids of moderate to high potency (hereafter, “topical corticosteroids”) after the eligibility date and (ii) patients without AD diagnosis with a prescription for topical corticosteroids during the study enrollment period and at least one other prescription within the prior 12 months. The indication for the individual prescriptions was not recorded. A cohort of individuals not treated with any of the study medications (“untreated cohort”), with or without recorded AD diagnosis, was also identified for contextualization.
To control confounding, when selecting the corticosteroid cohort to match to each TCI cohort, we calculated exposure propensity scores (PSs) representing the probability of initiating TCI treatment rather than receiving topical corticosteroids, given a set of baseline covariates. After creating the PSs, trimming was performed to remove non-overlapping and extreme values within the PS distributions. All individuals (both TCI and corticosteroid) above the upper 99th percentile of the corticosteroid PS score distribution were trimmed, as were all individuals below the lowest 1st percentile of the TCI PS score distribution. After trimming, all remaining TCI users were retained as the TCI cohort and PS twentiles within this TCI cohort were identified. Then up to four times as many users of topical corticosteroids, depending on availability, were randomly selected, from all users of topical corticosteroids within each twentile-based stratum, to form the matched corticosteroid cohort.
For contextualization, each user of corticosteroids from the comparator cohort for tacrolimus was matched to four nonusers of any study medication on age, sex, geographic region, and calendar year of start date (untreated cohort).
Follow-up continued from the start date to the earliest of death, database disenrollment, end of the study, or occurrence of one of the study outcomes.
Exposure
Based on records of prescriptions (UK-CPRD) or dispensing (NL-PHARMO, Denmark, and Sweden), exposure to tacrolimus and pimecrolimus was defined as single use (any topical tacrolimus or topical pimecrolimus, but not both) for each of these medications.
Cumulative dose was the total quantity of active substance that a patient received during follow-up (grams) calculated from the strength of the formulation and the package size.
Outcomes
In Denmark and Sweden, outcomes were identified in national cancer registries. For NL-PHARMO, the pathology registry was used, and in the UK-CPRD, outcomes were identified via information from general practices, hospital admissions, and the cancer registry. In NL-PHARMO and UK-CPRD, case validation was performed for all pediatric cases, all CTCL cases, and a random sample of other adult cases. Validation was done in NL-PHARMO by an independent pathologist reviewing pathology excerpts and UK-CPRD by clinical review of electronic medical records.
Covariates
Covariates included immunosuppressive disease and use of immunosuppressive agents; chronic disease; severe skin diseases; AD diagnosis, if available; and measures of healthcare resource utilization. Age, sex, year of start date, and type of prescriber were forced into the PS models. Variables associated with the outcome were also included in the models regardless of whether they were associated with the exposure.8
Because information on AD severity was limited or missing in all the data sources, we evaluated the effect of type of prescriber of the first prescription as a proxy for severity of the cutaneous condition. The underlying assumption was that patients with more severe AD would have been seen and treated first by a dermatologist and patients with less severe AD would have been seen and treated first by a GP. The variable was available in Denmark, NL-PHARMO, and Sweden, but not in UK-CPRD.
Statistical Analysis
We evaluated the overall effect as well as the effect of cumulative dose of topical tacrolimus and topical pimecrolimus compared with use of topical corticosteroids. In each data source, cancer events and person-years were stratified between decile boundaries of PSs.9 We then used Mantel-Haenszel methods10 to estimate overall adjusted incidence rate ratios (IRRs) and incidence rate differences, stratifying on study database, deciles of PSs, and sex; and, in NL-PHARMO, Denmark, and Sweden, by type of prescriber (dermatologist, non-dermatologist) of the first prescription. For the main analysis, time at risk started after a lag time of 6 months. Additional analyses with 0-month, 12-month, 24-month, and 48-month lag times were conducted to explore reverse causation and surveillance bias. No hypothesis testing was performed, but 95% confidence intervals (CIs) were calculated around IRRs and incidence rate differences to allow interpretation of the strength of observed effects. No imputation was performed for missing values given the observational nature of the data analyzed in this study. If no prescription for a particular medication existed in the patient’s record, it was assumed the patient was not taking that medication, and if a medical event was not observed in the patient’s medical record, it was assumed they did not have that event.
To further assess whether treatment with the study medications was initiated for signs and symptoms that were compatible with early manifestations of CTCL, we obtained additional information from questionnaires sent to general practitioners in UK-CPRD and reviewed the medical records in Sweden for CTCL cases.11 We analyzed the occurrence of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) separately to test the role of immunosuppression in the results.
The study was based on medical records. The individual Institutional Review Boards or the Data Protection and Research committees waived the requirement of informed consent due to appropriate handling of patient data and maintenance of patient data confidentiality. We obtained ethical and scientific reviews from the RTI International institutional review board, the Regional Ethical Review Board of Stockholm, the CPRD Independent Scientific Advisory Committee, and the UK National Cancer Intelligence Network. Ethical approval was not required in PHARMO and Denmark. In PHARMO, the study fulfilled the requirements of the PHARMO Compliance Commission, and permission for the use of data from the Dutch National Pathology Registry was obtained. In Denmark, the study was approved by the Danish Data Protection Agency via Statistics Denmark. The study has received the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP) Study Seal. The protocol for the JOELLE study extension phase, protocol version 5.0, dated Jun 30, 2017, is posted in the EU PAS Register, EUPAS21769 #21769.
Results
The study included 126,908 adults and 32,605 children initiating treatment with topical tacrolimus. These patients were compared with 452,996 adults and 117,592 children treated with topical corticosteroids. Similarly, 61,841 adults and 27,961 children initiating treatment with topical pimecrolimus were compared with 244,572 adults and 111,024 children treated with topical corticosteroids. The untreated cohort comprised 1,291,042 adults and 361,584 children. Table 2 shows the distribution of patients by study cohort and population. The distributions by age and sex were similar in all study cohorts. The baseline prevalence of comorbidities and use of medications were similar overall between the topical tacrolimus and topical pimecrolimus cohorts but were different across data sources.
 |  |  |
Table 1 STROBE Statement for Cohort Studies with the RECORD Statement Extension—Checklist of Items That Should Be Included in Reports of Observational Studies Using Routinely Collected Health Data |
 |
Table 2 Distribution of Users by Study Cohort and Population |
Overall follow-up was ≥10 years for 19% of adults and for 32% of children. For users of topical tacrolimus, the median follow-up was 5.7 years in children and 5.0 years in adults. For users of topical pimecrolimus, the median follow-up was 8.9 years in children and 6.5 years in adults.
The median number of prescriptions was 1 for both tacrolimus and pimecrolimus. The median dose of active substance was 0.03 grams for tacrolimus (equivalent to a single 30-gram tube of 0.1% tacrolimus) and 0.3 grams for pimecrolimus (equivalent to a single 30-gram tube of 1% pimecrolimus). Other population characteristics are available in eTable 1 and eTables 4–9 of the Supplementary Materials.
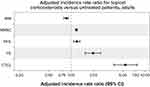
Use of Topical Tacrolimus versus Topical Corticosteroids
In adults, users of topical tacrolimus had an IRR for NMSC of 1.04 (95% CI, 1.00–1.09). The IRR point estimates for melanoma, NHL (excluding CTCL), and HL were <1 (Table 3, Figure 1). The IRR for CTCL with use of topical tacrolimus was 1.80 (95% CI, 1.25–2.58), corresponding to an excess risk of 3 cases per 100,000 person-years (95% CI, 1–6). IRRs for CTCL were 0.81 (95% CI, 0.45–1.47) for a cumulative dose of ≤ 0.05 grams, 2.11 (95% CI, 1.13–3.95) for a cumulative dose from 0.05 to 0.10 grams, and 5.25 (95% CI, 3.21–8.56) for a cumulative dose > 0.10 grams.
 |
Table 3 Pooled Adjusted Incidence Rate Ratios in Users of Topical Tacrolimus and Topical Pimecrolimus Compared with Users of Topical Corticosteroids—Adults |
For adult users of topical tacrolimus in whom the time since first exposure to treatment was ≥5 years, the IRR for CTCL was 0.25 (95% CI, 0.03–1.87) (Table 4). In the sensitivity analysis to address reverse causation conducted in UK-CPRD and Sweden, there was little change in the estimated effect on CTCL associated with topical tacrolimus when cases with manifestations of a previous skin condition in the same location as the subsequently diagnosed cutaneous lymphoma were omitted (see eTable 2 and eTable 3 in the Supplementary Materials).
In children (Figure 1), the IRR comparing use of topical pimecrolimus with topical corticosteroids was 0.69 (95% CI, 0.20–2.31) for melanoma and 0.63 (95% CI, 0.13–3.13) for NMSC. The IRR comparing use of topical tacrolimus with topical corticosteroids was 2.19 (95% CI, 0.81–5.97) for NHL (excluding CTCL), 2.37 (95% CI, 0.99–5.68) for HL, and 7.77 (95% CI, 0.50–121.45) for CTCL. The IRR for each type of lymphoma was based on few events. For NHL, the IRR was elevated for low cumulative doses, but not for medium or high cumulative doses. For HL, the IRR was elevated for low and high doses, but not for medium doses.
Use of Topical Pimecrolimus versus Topical Corticosteroids
In adults (Table 3, Figure 1), the IRR for melanoma for use of topical pimecrolimus was 1.21 (95% CI, 1.03–1.41), which corresponds to an excess risk of 10 cases per 100,000 person-years (95% CI, 1–18). The adjusted IRR for NMSC with topical pimecrolimus was 1.28 (95% CI, 1.20–1.35), an excess risk of 91 cases per 100,000 person-years (95% CI, 68–114). In adults, the IRR point estimates for NHL (excluding CTCL), HL, and CTCL for users of topical pimecrolimus compared with users of topical corticosteroids were all <1.
In children, the IRR point estimates for each study outcome for topical pimecrolimus compared with topical corticosteroids were based on few events and all were <1 (Figure 1).
Users of Topical Corticosteroids versus Untreated Population
In adults, the IRRs for all outcomes except melanoma were elevated in the cohort of users of topical corticosteroids compared with the untreated population (Figure 2), especially for CTCL (IRR, 5.42; 95% CI, 3.77–7.79). In children, the number of cases was too small for estimating the IRR for the individual outcomes.
Discussion
Adult users of topical tacrolimus had IRRs <1 for melanoma, NHL (excluding CTCL), and HL, which indicates that no increased risk of these outcomes was found in topical tacrolimus users compared with topical corticosteroid users. For topical pimecrolimus users, the IRRs for any type of lymphoma were likewise <1. In our study, the results were not homogeneous, and topical tacrolimus and pimecrolimus were not found to produce effects on the same outcomes in contrast with findings from a systematic review that suggested an association between TCI use and risk of lymphoma and no other cancers.4
For topical tacrolimus users, the IRR for CTCL was elevated, and the incidence of CTCL increased with increasing cumulative dose. This finding may reflect a causal effect or be the result of confounding by indication. AD is associated with increased risk of malignancies, and the strength of the association is related to the severity of the AD.6,7 According to the European Medicines Agency–approved labeling, TCIs are indicated only for AD, while topical corticosteroids are also indicated for the treatment of other skin diseases, so a higher proportion of patients without AD are likely included in the topical corticosteroid than in the TCI cohorts. In databases capturing diagnosis from hospital data only, AD diagnoses are often missing, which could hamper the control of confounding and result in overestimation of the risks associated with use of TCIs. Type of prescriber of the first prescription was used as a proxy measure for severity of the underlying cutaneous condition, except in UK-CPRD, where this information was not available. Still, residual confounding is possible and would result in an overestimation of the effect of the study medications, especially for topical tacrolimus, which is indicated for more severe forms of AD.
The IRRs for all outcomes except melanoma were elevated in the analysis of topical corticosteroid users compared with nonusers of any study medication, indicating that either the topical corticosteroids or their indication confers an increased risk of the outcomes studied.
Reverse causation is a concern because patients in early stages of certain skin malignancies, particularly CTCL, may present clinical manifestations resembling AD and therefore may be treated with the study medications. Our efforts to address this produced conflicting results. Although the cumulative dose-response analysis shows the highest risk with the highest cumulative dose, in one sensitivity analysis, the elevated relative risk of CTCL associated with topical tacrolimus was confined to the first years after starting the medication, a pattern that seems more consistent with reverse causation than with a causal effect of topical tacrolimus. However, the other sensitivity analysis for reverse causation indicated little change in the estimated effect of topical tacrolimus on the risk of CTCL when cases with manifestations of a previous skin condition in the same location as the subsequently diagnosed cutaneous lymphoma were omitted.11
In adults, IRRs for melanoma and NMSC in users of topical pimecrolimus were elevated. This may reflect surveillance bias, although that does not explain the greater IRR with greater cumulative doses. In a sensitivity analysis, among NMSC, the overall BCC-to-SCC ratio was >3 in the pimecrolimus and the corticosteroids cohorts. Because SCCs predominate over BCCs in clinical settings where strong immunosuppression is associated with an increased risk of NMSC, these results suggest that systemic immunosuppression is unlikely to be an important cause of the observed associations between exposure to the study drugs and the risk of NMSC in this study.12–16
Results from this study are consistent with those from other published studies7,17–19 summarized in a 2011 briefing document to the US Food and Drug Administration:
causality is difficult to determine in light of the potential study biases. (eg, misclassification of lymphoma, protopathic bias, and confounding by indication)20
Moreover, this study shows that any excess risk would be low and confined to a few years after first exposure.
The pediatric population in the JOELLE study was larger than all previous study populations in this area; however, few events occurred among children treated with TCIs. The IRR for each type of lymphoma was elevated for topical tacrolimus at low cumulative doses. Associations that are strongest among those with a low cumulative dose typically are the result of reverse causation or surveillance bias rather than a causal effect because low cumulative dose is correlated with short duration of use and an outcome may already have been present, although clinically undetected, when exposure began. It is also notable that no lymphomas occurred in a recently presented cohort study of 7954 children treated with topical tacrolimus in 2005–2012 (mean follow-up, 6.4 years; 15% were followed for ≥10 years).21
This study is the largest to date to evaluate the association of TCIs with skin cancer and lymphomas and includes the longest duration of follow-up of patients in population-based data sources. When analyzing the risk of malignancies associated with long-term follow-up, the data were not consistent with an increased risk of skin cancer or lymphoma as the duration of follow-up increased. However, despite being the largest study of these agents with the longest follow-up, the rarity of the outcomes in children limits the conclusions.
Conclusion
We found little evidence of an association between the use of either topical tacrolimus or topical pimecrolimus and the occurrence of skin cancer and lymphoma. The elevated IRR for CTCL among adult users of topical tacrolimus and the elevated IRRs for melanoma and NMSC among adult users of topical pimecrolimus could represent causal effects or might result from the underlying disease. The IRRs for skin cancer or lymphoma in adults in the fifth and subsequent years since first exposure to the study medications were not increased as might be expected if these were causal effects. Even if causal, the public health impact of these excess risks would be low. Also, the prognosis of these outcomes might be improved through early diagnosis by doctors being alert to the potential development or unmasking of a cutaneous malignancy in patients with a dermatological condition treated with topical immunomodulators.
Abbreviations
AD, atopic dermatitis; BCC, basal cell carcinoma; CI, confidence interval; CTCL, cutaneous T-cell lymphoma; EMA, European Medicines Agency; HL, Hodgkin lymphoma; IRR, incidence rate ratio; JOELLE study, Protopic Joint European Longitudinal Lymphoma and Skin Cancer Evaluation; NHL, non-Hodgkin lymphoma; NL-PHARMO, PHARMO Database Network in the Netherlands; NMSC, nonmelanoma skin cancer; PS, propensity score; RTI, RTI International, of which RTI Health Solutions is a business unit; SCC, squamous cell carcinoma; TCI, topical calcineurin inhibitor; UK, United Kingdom; UK-CPRD, Clinical Practice Research Datalink in the UK; US, United States.
STROBE Statement
This manuscript complies with the STROBE Statement for the reporting of epidemiological studies (https://www.strobe-statement.org/index.php?id=strobe-home). The STROBE checklist is on Table 1.
Data Sharing Statement
Data in the study were aggregated. Individual patient-level data from each database were analyzed and remain in the home institutions because of data protection rules.
Ethics Approval and Informed Consent
The RTI study team received approval for exemption from review by the RTI International institutional review board on November 22, 2017.
Ethics approval is not required for anonymized database research in the Netherlands. However, this study fulfilled the requirements, as checked by the PHARMO Compliance Commission on October 7, 2011, to use data from the PHARMO Database Network (NL-PHARMO) for this specific study. Permission for the use of data from the Dutch National Pathology Registry (PALGA) was received on April 23, 2013. Approval for access to the Netherlands Cancer Registry staging data for melanoma cases was received on August 9, 2018.
The study extension was approved by the Danish Data Protection Agency via Statistics Denmark on March 13, 2018. According to Danish law, studies based solely on register data do not require approval from an ethics review board.
The Centre for Pharmacoepidemiology at Karolinska Institutet received ethics approval for the JOELLE study extension phase and for the medical record review of cutaneous lymphoma cases on July 12, 2017, and approval to use data from the Swedish registers from the National Board of Health and Welfare on November 24, 2017.
Approval of the Clinical Practice Research Datalink (CPRD) Independent Scientific Advisory Committee was received on March 26, 2018 (protocol number, 13_121RAR).
Acknowledgments
The contract between RTI Health Solutions and LEO Pharma to conduct this study provides independent publication rights to the research team. The sponsor provided input on the study design but had no role in data collection or analysis. In line with the Guidance on Good Pharmacovigilance Practices (GVP): Module VIII, of the European Medicines Agency, the sponsor reviewed the manuscript and provided comments, but the authors made final decisions regarding its content and submission. All authors had full access to all of the data (including statistical reports and tables) and take responsibility for the integrity and accuracy of the data analysis and results.
The investigators would like to thank Henny Bang Jakobsen, Malene Nielsen, Thomas Delvin, and Mette Stagaard Janas, for the continuous support and coordination within LEO Pharma.
At RTI Health Solutions: Joan Fortuny, MD, PhD, and Xabier García de Albéniz, MD, MS, PhD, for clinical case review; Carla Franzoni, BS, for project management and administration; Joan Forns, PhD, David Martinez, BS, MSc, and Nuria Riera, PhD, for epidemiology support; and Paul Hobson, John Forbes, and Adele Monroe, DVM, MSPH, ELS, for editorial review.
At the UK-CPRD: the Independent Scientific Advisory Committee; the Interventional Research team for their work on the questionnaire study; and all contributing general practitioners.
At PHARMO: Willeke Blokx, MD, for clinical case review; Huub Straatman, data analyst, for programming and analysis; and all contributing health care providers for providing their data to the PHARMO Database Network and the Dutch National Pathology Registry (PALGA).
At the University of Southern Denmark: Morten Olesen and Martin T. Ernst for valuable help with data management.
At the Centre for Pharmacoepidemiology, Karolinska Institutet: Camilla Byström for medical record reviews.
The authors would like to thank the general practitioners contributing information to the Clinical Practice Research Datalink (CPRD) in the United Kingdom and the health care providers contributing information to the PHARMO Database Network and the Dutch National Pathology Registry (PALGA).
The research team chose the acronym JOELLE to honor Dr Joelle Erkens, pharmacoepidemiologist at Astellas and formerly at PHARMO Institute, who was lost to the research team in June 2011 upon her untimely death.
Funding
The study was funded by LEO Pharma.
Disclosure
Alejandro Arana, Lia Gutiérrez, Brian Calingaert, Kenneth J Rothman, James A Kaye, and Susana Perez-Gutthann are full-time employees of RTI International, an independent nonprofit research organization that does work for government agencies and pharmaceutical companies including LEO Pharma and Astellas Pharma. As employees of RTI International, Susana Perez-Gutthann, Kenneth J Rothman, and James A Kaye also participate in scientific advisory boards (for studies and medications) that are funded by pharmaceutical companies.
Josephina Kuiper and Eline Houben are employees of the PHARMO Institute for Drug Outcomes Research. This independent research institute performs financially supported studies for government and related health care authorities and several pharmaceutical companies.
Jesper Hallas, Anton Pottegård, and Lars Christian Lund are employees of the University of Southern Denmark, Clinical Pharmacology and Pharmacy. They have participated in studies funded by pharmaceutical companies including LEO Pharma and Menarini Pharmaceuticals; funds are paid to their employer.
Daniel Dedman, Elizabeth Crellin, and Helen Booth are employees of the Clinical Practice Research Datalink (CPRD), which provides contract research services for government and related health care authorities and pharmaceutical companies including LEO Pharma.
Helle Kieler, Karin Gembert, and Johan Reutfors are employees of the Centre for Pharmacoepidemiology of the Karolinska Institutet in Sweden, which receives grants from regulatory authorities, pharmaceutical companies including LEO Pharma and Astellas Pharma, and contract research organizations for performance of drug safety and drug utilization studies.
Professor Marcus Schmitt-Egenolf MD, PhD, is an employee of the Department of Public Health & Clinical Medicine, Umeå University, Sweden. The authors report no other conflicts of interest in this work.
References
1. Örtqvist A, Lundholm C, Wettermark B, Ludvigsson J, Ye W, Almqvist C. Validation of asthma and eczema in population-based Swedish drug and patient registers. Pharmacoepidemiol Drug Saf. 2013;22(8):850–860. doi:10.1002/pds.3465
2. Asgari MM, Tsai AL, Avalos L, Sokil M, Quesenberry CP
3. Castellsague J, Kuiper JG, Pottegard A, et al. A cohort study on the risk of lymphoma and skin cancer in users of topical tacrolimus, pimecrolimus, and corticosteroids (Joint European Longitudinal Lymphoma and Skin Cancer Evaluation - JOELLE study). Clin Epidemiol. 2018;10:299–310. doi:10.2147/CLEP.S146442
4. Lam M, Zhu JW, Tadrous M, Drucker AM. Association between topical calcineurin inhibitor use and risk of cancer, including lymphoma, keratinocyte carcinoma, and melanoma: a systematic review and meta-analysis. JAMA Dermatol. 2021;157(5):549–558. doi:10.1001/jamadermatol.2021.0345
5. Tennis P, Gelfand JM, Rothman KJ. Evaluation of cancer risk related to atopic dermatitis and use of topical calcineurin inhibitors. Br J Dermatol. 2011;165(3):465–473. doi:10.1111/j.1365-2133.2011.10363.x
6. Arana A, Wentworth CE, Fernandez-Vidaurre C, Schlienger RG, Conde E, Arellano FM. Incidence of cancer in the general population and in patients with or without atopic dermatitis in the U.K. Br J Dermatol. 2010;163(5):1036–1043. doi:10.1111/j.1365-2133.2010.09887.x
7. Arellano FM, Wentworth CE, Arana A, Fernandez C, Paul CF. Risk of lymphoma following exposure to calcineurin inhibitors and topical steroids in patients with atopic dermatitis. J Invest Dermatol. 2007;127(4):808–816. doi:10.1038/sj.jid.5700622
8. Brookhart Ma, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Sturmer T. Variable selection for propensity score models. Am J Epidemiol. 2006;163(12):1149–1156. doi:10.1093/aje/kwj149
9. Sturmer T, Wyss R, Glynn RJ, Brookhart MA. Propensity scores for confounder adjustment when assessing the effects of medical interventions using nonexperimental study designs. J Intern Med. 2014;275(6):570–580. doi:10.1111/joim.12197
10. Rothman KJ, Greenland S, Lash TL, eds. Modern Epidemiology.
11. Gutierrez L, Booth H, Dedman D, et al. Case validation of cutaneous lymphoma to minimize protopathic bias.
12. Berg D, Otley CC. Skin cancer in organ transplant recipients: epidemiology, pathogenesis, and management. J Am Acad Dermatol. 2002;47(1):1–17;quiz 18-20. doi:10.1067/mjd.2002.125579
13. Hartevelt MM, Bavinck JN, Kootte AM, Vermeer BJ, Vandenbroucke JP. Incidence of skin cancer after renal transplantation in The Netherlands. Transplantation. 1990;49(3):506–509. doi:10.1097/00007890-199003000-00006
14. Jensen P, Hansen S, Moller B, et al. Skin cancer in kidney and heart transplant recipients and different long-term immunosuppressive therapy regimens. J Am Acad Dermatol. 1999;40(2 Pt 1):177–186. doi:10.1016/S0190-9622(99)70185-4
15. Mittal A, Colegio OR. Skin cancers in organ transplant recipients. Am J Transplant. 2017;17(10):2509–2530. doi:10.1111/ajt.14382
16. Zwald FO, Brown M. Skin cancer in solid organ transplant recipients: advances in therapy and management: part I. Epidemiology of skin cancer in solid organ transplant recipients. J Am Acad Dermatol. 2011;65(2):253–261; quiz 262. doi:10.1016/j.jaad.2010.11.062
17. Hui RL, Lide W, Chan J, Schottinger J, Yoshinaga M, Millares M. Association between exposure to topical tacrolimus or pimecrolimus and cancers. Ann Pharmacother. 2009;43(12):1956–1963. doi:10.1345/aph.1M278
18. Schneeweiss S, Doherty M, Zhu S, et al. Topical treatments with pimecrolimus, tacrolimus and medium- to high-potency corticosteroids, and risk of lymphoma. Dermatology. 2009;219(1):7–21. doi:10.1159/000209289
19. Margolis DJ, Abuabara K, Hoffstad OJ, Wan J, Raimondo D, Bilker WB. Association between malignancy and topical use of pimecrolimus. JAMA Dermatol. 2015;151(6):594–599. doi:10.1001/jamadermatol.2014.4305
20. Manthripragada A. Addendum: update on calcineurin inhibitor pediatric literature review (FDA briefing document). Office of Surveillance and Epidemiology, FDA Center for Drug Evaluation and Research, Food and Drug Administration; May 10, 2011. Available from: https://wayback.archive-it.org/7993/20170114054651/http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/PediatricAdvisoryCommittee/UCM255140.pdf.
21. Paller AS, Folster-Holst R, Chen SC, et al. No evidence of increased cancer incidence in children using topical tacrolimus for atopic dermatitis. J Am Acad Dermatol. 2020;83(2):375–381. doi:10.1016/j.jaad.2020.03.075
22. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.