Back to Journals » Clinical Ophthalmology » Volume 11
Long-term results of combination therapy using anti-VEGF agents and dexamethasone intravitreal implant for retinal vein occlusion: an investigational case series
Authors Singer MA, Jansen ME, Tyler L, Woods P, Ansari F, Jain U, Singer J, Bell D, Krambeer C
Received 9 August 2016
Accepted for publication 8 November 2016
Published 19 December 2016 Volume 2017:11 Pages 31—38
DOI https://doi.org/10.2147/OPTH.S119373
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Michael A Singer,1 Michael E Jansen,2 Lyndon Tyler,2 Paul Woods,1 Faisal Ansari,2 Udit Jain,2 Joshua Singer,1 Darren Bell,1 Chelsey Krambeer1
1Medical Center Ophthalmology Associates, 2University of Texas Health and Science Center at San Antonio, San Antonio, TX, USA
Background: One limitation of anti-VEGF therapy is the need for monthly retreatment to maintain efficacy. The purpose of this study was to determine the duration of effect in eyes with macular edema (ME) secondary to branch or central retinal vein occlusion (BRVO or CRVO) treated with anti-VEGF therapy plus sustained-release dexamethasone (DEX implant; Ozurdex).
Materials and methods: This open-label, interventional case series included 62 eyes with ME due to RVO, central foveal thickness (CFT) >300 µm, and best-corrected visual acuity (BCVA) of 20/40 or worse. Each treatment cycle included an anti-VEGF injection followed 2 weeks later with DEX implant. Patients were eligible for retreatment if CFT increased to >290 µm or increased by >50 µm from the lowest measurement, or if BCVA decreased by six or more Snellen letters. Efficacy and safety were evaluated 2 and 4–6 weeks after the beginning of each treatment cycle and every 4 weeks thereafter until retreatment criteria were met. The primary outcome measure was time to retreatment. Secondary outcome measures included BCVA, CFT, and safety parameters.
Results: The mean reinjection interval for all patients was 135.5±36.4 days. There was no statistically significant difference in mean intertreatment interval for up to six cycles of treatment or between eyes with BRVO or CRVO (P≥0.058). Mean peak change in BCVA was 13.8 letters, and 47.6% of eyes gained three or more lines of BCVA. The mean peak decrease in CFT across all treatment cycles was 200.9 µm for eyes with BRVO and 219.2 µm for eyes with CRVO. The percentage of patients with CFT ≤300 µm at any time during a given treatment cycle ranged from 78% to 94% among eyes with BRVO and from 85% to 100% among eyes with CRVO. Intraocular pressure increased in 19 of 62 eyes, and 26 of 44 phakic eyes underwent cataract surgery.
Conclusion: In eyes with ME due to RVO, treatment with an anti-VEGF agent plus DEX implant provided a predictable duration of effect, as well as significant improvements in BCVA and CFT.
Keywords: dexamethasone, intravitreal, macular edema, retinal vein occlusion
Background
Macular edema (ME) is the leading cause of vision loss in both branch and central retinal vein occlusion (BRVO and CRVO).1 Since 2010, several intravitreal medical therapies have been approved for the treatment of ME associated with RVO.2,3 These include the VEGF antagonists ranibizumab (Lucentis®; Genentech Inc, San Francisco, CA, USA) and aflibercept (Eylea®; Regeneron Pharmaceuticals Inc, Tarrytown, NY, USA), and the steroid dexamethasone in a sustained-release intravitreal implant (DEX implant; Ozurdex®; Allergan Inc, Irvine, CA, USA).2,3 Prior to the availability of approved intravitreal therapies, intravitreal injections of the anti-VEGF agent bevacizumab (Avastin®; Genentech) and the steroid triamcinolone acetonide were used off-label to treat ME due to BRVO or CRVO,4–6 and both are still used by some physicians when approved therapies are not available.
All of these treatments have been shown to produce significant improvements in central foveal thickness (CFT) and best-corrected visual acuity (BCVA) in randomized clinical trials of patients with ME due to RVO, but none is effective in all patients, and all have limitations.4–11 One of the most important limitations of anti-VEGF therapy is the need for monthly retreatment to maintain efficacy.7,8,10,11 This places a substantial burden on patients and puts them at risk of decreased efficacy if they miss a monthly dose. Consequently, there is an important need for treatment paradigms that can reduce ME and provide meaningful improvements in vision with a longer intertreatment interval. The visual and anatomical benefits of DEX implant in ME due to RVO can last for 4–6 months, but like the anti-VEGF agents, DEX implant is not effective in all patients.9 Although the exact mechanisms of action of the anti-VEGF and steroid therapies for ME in RVO are unknown, their fundamentally different molecular effects (VEGF inhibition vs anti-inflammatory effect) suggest that they might have synergistic effects when used in combination to treat ME associated with RVO.
In 2009, a prospective, interventional case series was initiated to evaluate the benefits of combination therapy with an anti-VEGF agent and DEX implant in eyes with ME due to BRVO or CRVO. Each treatment cycle consisted of an anti-VEGF injection followed 2 weeks later by insertion of a DEX implant; each cycle was repeated whenever there was a significant increase in CFT or decrease in BCVA. The results for the first 34 eyes treated for up to 6 months with bevacizumab and DEX implant have been described, and showed that this combination could produce significant improvements in BCVA and CFT with a mean retreatment interval of 126 days.12 This study is ongoing, and the purpose of the present report is to describe the results for 62 eyes treated with anti-VEGF and DEX-implant combination therapy for up to six treatment cycles and 33 months of follow-up.
Materials and methods
This open-label interventional case series was Health Insurance Portability and Accountability Act-compliant and adhered to the tenets of the Declaration of Helsinki. Institutional review board approval was obtained from the Specialty Surgery Center of San Antonio prior to study start, and written informed consent was obtained from each participant before study enrollment.
Patients at least 18 years of age with ME secondary to RVO were enrolled in the study from September 2009 through June 2014. The key eligibility criteria for enrollment were CFT >300 μm on spectral domain optical coherence tomography and BCVA of 20/40 or worse. Patients were excluded if they had rubeosis, advanced glaucoma (defined as cup-to-disk ratio >0.8), or a history of pars plana vitrectomy. Prior treatment with anti-VEGF therapy was allowed if the last treatment was >6 weeks before study enrollment. For the current analysis, only patients who had received at least three cycles of treatment or had follow-up greater than 14 months’ duration were included.
Each treatment cycle consisted of intravitreal anti-VEGF therapy (bevacizumab, ranibizumab, or aflibercept) followed 2 weeks later by insertion of a DEX implant. The type of anti-VEGF agent given was based on availability and individual insurance-plan formulary guidelines. Patients were eligible for retreatment if CFT increased to >290 μm or increased by >50 μm from the lowest measurement, or if BCVA decreased by six or more Snellen letters. Efficacy and safety were evaluated 2 and 4–6 weeks after the beginning of each treatment cycle and every 4 weeks thereafter until retreatment criteria were met. For the current analysis, only data collected through June 30, 2014 were included.
The primary outcome measure was time to retreatment. Secondary outcome measures were mean change from baseline BCVA; percentage of patients with three or more lines’ improvement from baseline BCVA; mean change from baseline CFT, as measured by spectral domain optical coherence tomography; percentage of patients with CFT <300 μm during each treatment cycle; percentage of patients with IOP ≥23, 25, 30, or 35 mmHg; and percentage of patients requiring cataract surgery during the study period. If more than one assessment of BCVA or CFT was made during a treatment cycle, the BCVA or CFT demonstrating the greatest improvement from baseline (peak effect) was used in the analysis. The peak effect typically occurred by the 8-week period.
All data analyses were based on observed values, with no imputation of missing values and no last observations carried forward. BCVA was converted to a Snellen-letter score using the logarithm of the minimum angle of resolution formula. Except for hand motion and finger count, which are given explicitly, letter measurements were calculated as the interpolated values between BCVA milestones.13 Cycle length was evaluated using analysis of variance. Changes from baseline in BCVA and CFT were evaluated with two-tailed t-tests, with an α-level of 0.05 used for statistical significance.
Results
Patients and treatment
A total of 62 eyes (40 with BRVO and 22 with CRVO) from 58 patients were included in this analysis (Table 1). Mean age was 72 years, 43 of 62 (68.3%) were female, and 32 of 62 (52.5%) were Caucasian. Prior to study entry, 26 of 62 (41.9%) eyes had previously been treated with at least one dose of bevacizumab, three of 62 (4.8%) had been treated with ranibizumab, and one of 62 (1.6%) had been treated with both bevacizumab and ranibizumab; 32 of 62 (51.6%) received their first dose of anti-VEGF therapy as part of the study.
During the study, eyes were treated with the most appropriate anti-VEGF therapy available at the time of each treatment (based on availability of medication and individual insurance-plan formulary guidelines). Most eyes (68%; 42 of 62) were treated with bevacizumab initially. Of these, 16 of 42 were switched from bevacizumab to ranibizumab when it became available. A total of 19 eyes (31%; 19 of 62) were treated with ranibizumab initially. Of these, five were switched to aflibercept when it became available. Only one eye was treated exclusively with aflibercept.
Patients were included in this analysis if they had received at least three cycles of treatment or had a follow-up duration of greater than 14 months since their last treatment. Of the 62 eyes included, 30 continue to receive treatment at regular follow-up visits, and 32 have exited the study. Of the 32 who discontinued, four moved out of the area, one died (unrelated to study medication), and 27 had a change in insurance. The number of eyes available for analysis varied with the number of treatment cycles, due to patient dropout and differences in the time of study entry into this ongoing trial.
Time to retreatment
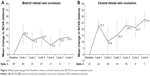
The mean (±standard deviation) intertreatment interval was 138.2±37.5 (range 42–183) days for eyes with BRVO and 131.2±34.4 (range 21–183) days for eyes with CRVO (P=0.64). Across all eyes, the mean intertreatment interval was 135.5±36.4 (range 21–183) days. There was no statistically significant difference in mean intertreatment interval for up to six cycles of treatment or between eyes with BRVO or CRVO (Figure 1; P≥0.058). Among eyes with BRVO, the mean time to retreatment for individual cycles varied from 124 days (95% confidence interval [CI] 25 days) to 143 days (95% CI 14 days). Among eyes with CRVO, the mean time to retreatment for individual cycles varied from 117 days (95% CI 24 days) to 140 days (95% CI 16 days). The intertreatment interval for individual patients tended to vary over the same range as the mean for the study population, with the occasional interval of 6 months or more.
  | Figure 1 Mean time to retreatment for each treatment cycle. Error bars represent 95% confidence intervals. |
Visual acuity
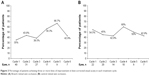
Mean BCVA at baseline was 54 letters among eyes with BRVO and 42 letters among eyes with CRVO. Mean peak improvement in BCVA across all treatment cycles was 12.5 (range 7.4–16.3) letters for eyes with BRVO and 20.1 (range 10.4–27.9) letters for eyes with CRVO. In general, mean peak BCVA remained fairly constant between treatment cycles (Figure 2). There was no statistically significant difference in mean change from baseline BCVA between the different treatment cycles for either BRVO or CRVO. The percentage of eyes that gained three or more lines of BCVA at any time during a given treatment cycle ranged from 35% to 67% among eyes with BRVO and from 43% to 60% among eyes with CRVO (Figure 3).
Central foveal thickness
Mean CFT at baseline was 470 μm among eyes with BRVO and 516 μm among eyes with CRVO. The mean peak decrease in CFT across all treatment cycles was 200.9 μm for eyes with BRVO and 219.2 μm for eyes with CRVO. In general, the mean peak change in CFT was relatively constant between cycles (Figure 4). The percentage of patients with CFT ≤300 μm at any time during a given treatment cycle ranged from 78% to 94% among eyes with BRVO and from 85% to 100% among eyes with CRVO (Figure 5).
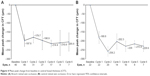  | Figure 4 Mean peak change from baseline in central foveal thickness (CFT). |
  | Figure 5 Percentage of patients with central foveal thickness ≤300 μm at any time in each treatment cycle. |
Safety
Seventy-one percent of eyes (44 of 62) were phakic at baseline. Of these, 62% (26 of 44) underwent cataract surgery during the course of the study. Across all eyes, 30.6% (19 of 62) experienced IOP ≥25 mmHg at some point during the study, and 4.8% (three of 62) experienced IOP ≥35 mmHg. The maximum IOP for any patient at any point during the study was 42 mmHg. No patients underwent incisional surgery, and only one patient received selective laser trabeculoplasty. Among eyes that developed increased IOP, the increase occurred within the first or second injection cycle in 75% of cases and within the first three cycles in 92% of cases.
Discussion
The most important findings of the present study are that combination therapy with an anti-VEGF agent and DEX implant produced substantial visual and anatomical improvements in eyes with ME due to RVO, and that these improvements could be maintained for up to 2 years with retreatment every 4–5 months. The mean time to retreatment, mean increase in BCVA, and mean decrease in CFT all remained relatively constant over up to six treatment cycles, with no sign of decreasing efficacy with repeated treatments. Approximately 20% of patients were considered “cured” at the end of the study, and did not require another round of combination therapy for 6 months after the last injection. This was based on both retinal thickness and BCVA.
In the present study, patients were monitored monthly and retreated with combination therapy as soon as any deterioration in vision (six or more Snellen letters) or macular thickness (>50 μm) was detected. This allowed the retreatment interval to vary according to the needs of each patient and if there was any change in treatment efficacy. Nonetheless, the mean retreatment interval was similar in eyes with BRVO and those with CRVO, and remained relatively constant at 4–5 months (plus or minus approximately 1 month) throughout the study. This predictable 4- to 5-month intertreatment interval suggests that some patients may not need to be monitored every month in order to ensure that their visual and anatomic treatment goals are being maintained.
The mean intertreatment interval seen in the present study (134 days) was similar to that reported for the first 34 eyes treated with this combination-therapy protocol (126 days).12 This 4- to 5-month retreatment interval is considerably longer than the monthly retreatment intervals required to maintain efficacy with anti-VEGF monotherapy.7,8,10,11 It is not known, however, what intertreatment intervals are required to maintain efficacy with DEX-implant monotherapy, because it has not been prospectively evaluated in pro re nata treatment regimens. A large, multicenter, retrospective chart review that included eyes that had been treated with DEX implants either alone or in combination with other treatments for ME due to RVO found a mean retreatment interval of 5.6 months.14 Lack of information about the retreatment criteria used in this earlier study, however, make the results difficult to compare to the findings of the present study.
In the present study, mean improvements in BCVA among eyes with BRVO remained near 12–13 letters across most treatment cycles, and there was no apparent change in efficacy with the number of treatments (Figure 2A). Among eyes with CRVO (Figure 2B), however, the mean improvement in BCVA was 20 or more letters during most treatment cycles and appeared to increase with the number of treatments (not statistically significant). In earlier studies, eyes with CRVO tended to show less improvement with treatment than eyes with BRVO,2 so the importance of the present findings are unclear and no strong conclusions should be drawn until the results can be verified.
The percentage of eyes gaining at least three lines of BCVA in the present study (35%–67% in each cycle) appeared to be in the same general range as those seen in randomized controlled studies of ranibizumab (BRVO 60%, CRVO 48%–51%)7,8 or aflibercept (BRVO 53%, CRVO 49%–56%)10,11,15 used as monotherapy, and higher than that reported for DEX-implant monotherapy (approximately 30%).9,16 This suggests that the addition of DEX implant to anti-VEGF therapy may provide efficacy similar to anti-VEGF monotherapy, but with a predictable 4- to 5-month retreatment interval. This should be verified in a larger, randomized clinical trial with an anti-VEGF monotherapy control group.
The improvements in CFT in the present study were generally similar between treatment cycles and between eyes with BRVO or CRVO. The overwhelming majority of eyes (78%–100%) achieved a CFT ≤300 μm during each treatment cycle. The mean decrease in CFT (201–219 μm) was very similar to what was seen in a randomized controlled trial of DEX implant in eyes with ME due to RVO (208 μm).9,16 Larger mean decreases in CFT were seen in the randomized, controlled trials of ranibizumab in eyes with ME due to RVO (345–452 μm).7,8 It is not clear, however, if this was due to the more frequent use of anti-VEGF therapy in these earlier trials or to differences in the patient population compared with the present study.
The adverse events most commonly associated with DEX-implant therapy are increased IOP and increased risk of cataract in phakic eyes.9,16 The increases in IOP seen in the present study were generally moderate, and no patient required incisional surgery to control their IOP. Rates of IOP increases in this study were similar to those seen in a study evaluating the use of two or more DEX implants in combination therapy to treat RVO.17 Importantly, the incidence of increased IOP tended to decrease with repeated treatments. Over the 2-year period covered by the present study, 62% of phakic patients required cataract surgery. This is similar to the rate of cataract surgery seen in phakic eyes that had been treated at least three consecutive times with DEX implants for RVO.18
There have been very few previous reports of the use of combined anti-VEGF and DEX implant in eyes with ME due to RVO. Of the few that do exist, only two are prospective, and none used the same treatment paradigm or retreatment criteria used in the present study. That being said, the results of previous studies suggest that the addition of DEX implant to anti-VEGF therapy allows the number of anti-VEGF treatments to be reduced, while providing efficacy similar to that seen with anti-VEGF monotherapy. One prospective study found that the addition of a DEX implant 1 week following intravitreal bevacizumab reduced the need for additional bevacizumab injections from monthly to every 3 months (on average).19 In this earlier study, retreatment with DEX implant was given every 4–5 months if needed, but not always given in conjunction with bevacizumab. In a separate, prospective case series of eyes with ME due to RVO, DEX-implant monotherapy was compared to eyes that had received three intravitreal bevacizumab injections followed by a DEX implant.20 This study found that this particular combination therapy was more effective than DEX-implant monotherapy among eyes with BRVO, but not among eyes with CRVO.20
The most important limitation of the present study is the lack of an anti-VEGF monotherapy control group. Although the efficacy results in the present study appear similar to what has been reported for anti-VEGF monotherapy, no strong conclusions can be drawn without a randomized, masked, head-to-head clinical trial. Another limitation is the use of three different anti-VEGF agents during the course of the study. Aflibercept was only approved for the treatment of ME due to RVO in October 2014, so the overwhelming majority of eyes in this study (56 of 62; 90%) were treated with bevacizumab and/or ranibizumab. The present study was not powered to detect a significant difference in outcomes between eyes treated with the different anti-VEGF agents, but it is possible that such differences exist. It should be noted, however, that two randomized, controlled trials and one retrospective chart review failed to find any statistically significant difference in the efficacy of bevacizumab and ranibizumab in eyes with ME due to RVO.21–23 In the recently completed Protocol T study conducted by the Diabetic Retinopathy Clinical Research Network,24 aflibercept was found to be more effective than bevacizumab and ranibizumab in the treatment of center-involving Diabetic Macular Edema in eyes with worse BCVA or greater macular thickness at baseline, but there was no treatment difference among eyes with good vision and less retinal thickening at baseline. There have been no head-to-head comparisons of aflibercept with the other anti-VEGF therapies in the treatment of ME due to RVO.
In conclusion, the present study demonstrated that the use of anti-VEGF injections followed 2 weeks later by the insertion of a DEX implant produced meaningful improvements in vision and retinal thickness in eyes with ME due to RVO. These improvements could be maintained with retreatment every 4–5 months for up to 2 years. The time until the need for retreatment remained relatively constant for up to six treatment cycles. The safety findings were similar to what has been reported for DEX-implant monotherapy. Overall, these findings suggest that combination therapy with an anti-VEGF agent and DEX implant may provide a valuable and flexible treatment alternative for patients with ME associated with RVO.
Acknowledgments
Allergan Inc provided the funds for professional writing assistance (Lindsay Biomedical Communications Inc) and statistical analysis, but played no role in study design, data collection or analysis, or manuscript preparation or approval. A preliminary report of this study was presented at the 29th Meeting of the Club Jules Gonin, September 2–6, 2014, Zurich, Switzerland, and the 47th Retina Society Meeting, September 11–14, 2014, Philadelphia, PA.
Disclosure
The authors report no conflicts of interest in this work.
References
Rehak M, Wiedemann P. Retinal vein thrombosis: pathogenesis and management. J Thromb Haemost. 2010;8(9):1886–1894. | ||
Pielen A, Feltgen N, Isserstedt C, Callizo J, Junker B, Schmucker C. Efficacy and safety of intravitreal therapy in macular edema due to branch and central retinal vein occlusion: a systematic review. PLoS One. 2013;8(10):e78538. | ||
Chatziralli I, Nicholson L, Sivaprasad S, Hykin P. Intravitreal steroid and anti-vascular endothelial growth agents for the management of retinal vein occlusion: evidence from randomized trials. Expert Opin Biol Ther. 2015;15(12):1685–1697. | ||
Lip PL, Malick H, Damer K, et al. One-year outcome of bevacizumab therapy for chronic macular edema in central and branch retinal vein occlusions in real-world clinical practice in the UK. Clin Ophthalmol. 2015;9:1779–1784. | ||
Ip MS, Scott IU, VanVeldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with observation to treat vision loss associated with macular edema secondary to central retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 5. Arch Ophthalmol. 2009;127(9):1101–1114. | ||
Scott IU, Ip MS, VanVeldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Arch Ophthalmol. 2009;127(9):1115–1128. | ||
Brown DM, Campochiaro PA, Bhisitkul RB, et al. Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology. 2011;118(8):1594–1602. | ||
Campochiaro PA, Brown DM, Awh CC, et al. Sustained benefits from ranibizumab for macular edema following central retinal vein occlusion: twelve-month outcomes of a phase III study. Ophthalmology. 2011;118(10):2041–2049. | ||
Haller JA, Bandello F, Belfort R Jr, et al. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion: twelve-month study results. Ophthalmology. 2011;118(12):2453–2460. | ||
Brown DM, Heier JS, Clark WL, et al. Intravitreal aflibercept injection for macular edema secondary to central retinal vein occlusion: 1-year results from the phase 3 COPERNICUS study. Am J Ophthalmol. 2013;155(3):429–437. | ||
Campochiaro PA, Clark WL, Boyer DS, et al. Intravitreal aflibercept for macular edema following branch retinal vein occlusion: the 24-week results of the VIBRANT study. Ophthalmology. 2015;122(3):538–544. | ||
Singer MA, Bell DJ, Woods P, et al. Effect of combination therapy with bevacizumab and dexamethasone intravitreal implant in patients with retinal vein occlusion. Retina. 2012;32(7):1289–1294. | ||
Colenbrander A. Measuring vision and vision loss. In: Duane T, editor. Duane’s Clinical Ophthalmology. Vol 5. Philadelphia: Lippincott Williams & Wilkins; 2001:1–39. | ||
Capone A Jr, Singer MA, Dodwell DG, et al. Efficacy and safety of two or more dexamethasone intravitreal implant injections for the treatment of macular edema related to retinal vein occlusion (SHASTA study). Retina. 2014;34(2):342–351. | ||
Heier JS, Clark WL, Boyer DS, et al. Intravitreal aflibercept injection for macular edema due to central retinal vein occlusion: two-year results from the COPERNICUS study. Ophthalmology. 2014;121(7):1414–1420. | ||
Haller JA, Bandello F, Belfort R Jr, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010;117(6):1134–1146. | ||
Singer MA, Capone A Jr, Dugel PU, et al. Two or more dexamethasone intravitreal implants as monotherapy or in combination therapy for macular edema in retinal vein occlusion: subgroup analysis of a retrospective chart review study. BMC Ophthalmol. 2015;15:33. | ||
Pina JP, Turki K, Labreuche J, Duhamel A, Tran TH. Efficacy and safety in retinal vein occlusion treated with at least three consecutive intravitreal dexamethasone implants. J Ophthalmol. 2016;2016:6016491. | ||
Maturi RK, Chen V, Raghinaru D, Bleau L, Stewart MW. A 6-month, subject-masked, randomized controlled study to assess efficacy of dexamethasone as an adjunct to bevacizumab compared with bevacizumab alone in the treatment of patients with macular edema due to central or branch retinal vein occlusion. Clin Ophthalmol. 2014;8:1057–1064. | ||
Mayer WJ, Remy M, Wolf A, et al. Comparison of intravitreal bevacizumab upload followed by a dexamethasone implant versus dexamethasone implant monotherapy for retinal vein occlusion with macular edema. Ophthalmologica. 2012;228(2):110–116. | ||
Narayanan R, Panchal B, Das T, Chhablani J, Jalali S, Ali MH. A randomised, double-masked, controlled study of the efficacy and safety of intravitreal bevacizumab versus ranibizumab in the treatment of macular oedema due to branch retinal vein occlusion: MARVEL report no 1. Br J Ophthalmol. 2015;99(7):954–959. | ||
Rajagopal R, Shah GK, Blinder KJ, et al. Bevacizumab versus ranibizumab in the treatment of macular edema due to retinal vein occlusion: 6-month results of the CRAVE study. Ophthalmic Surg Lasers Imaging Retina. 2015;46(8):844–850. | ||
Yuan A, Ahmad BU, Xu D, et al. Comparison of intravitreal ranibizumab and bevacizumab for the treatment of macular edema secondary to retinal vein occlusion. Int J Ophthalmol. 2014;7(1):86–91. | ||
Diabetic Retinopathy Clinical Research Network. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372(13):1193–1203. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.