Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Long-term outcomes and predictors of survival after cardiopulmonary resuscitation for in-hospital cardiac arrest in a tertiary care hospital in Thailand
Authors Limpawattana P , Aungsakul W, Suraditnan C, Panitchote A, Patjanasoontorn B , Phunmanee A , Pittayawattanachai N
Received 19 November 2017
Accepted for publication 24 January 2018
Published 20 March 2018 Volume 2018:14 Pages 583—589
DOI https://doi.org/10.2147/TCRM.S157483
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Garry Walsh
Panita Limpawattana,1 Wannaporn Aungsakul,2 Chomchanok Suraditnan,2 Anupol Panitchote,3 Boonsong Patjanasoontorn,3 Anakapong Phunmanee,3 Nittaya Pittayawattanachai4
1Division of Geriatric Medicine, Department of Internal Medicine, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand; 2Department of Internal Medicine, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand; 3Division of Critical Care, Department of Internal Medicine, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand; 4CPR Unit, Srinagarind Hospital, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand
Background: There are limited data available regarding long-term survival and its predictors in cases of in-hospital cardiac arrest (IHCA) in which patients receive cardiopulmonary resuscitation.
Purpose: The objectives of this study were to determine the 1-year survival rates and predictors of survival after IHCA.
Patients and methods: Data were retrospectively collected on all adult patients who were administered cardiopulmonary resuscitation from January 1, 2013 to December 31, 2014 in Srinagarind Hospital (Thailand). Clinical outcomes of interest and survival at discharge and 1 year after hospitalization were reviewed. Descriptive statistics and survival analysis were used to analyze the outcomes.
Results: Of the 202 patients that were included, 48 (23.76%) were still alive at hospital discharge and 17 (about 8%) were still alive at 1 year post cardiac arrests. The 1-year survival rate for the cardiac arrest survivors post hospital discharge was 72.9%. Prearrest serum HCO3<20 meq/L, asystole, urine <800 cc/d, postarrest coma, and absence of pupillary reflex were predictors of death.
Conclusion: Only 7.9% of patients with IHCA were alive 1 year following cardiac arrest. Prearrest serum HCO3<20 meq/L, asystole, urine <800 cc/d, postarrest coma, and absence of pupillary reflex were the independent factors that predicted long-term mortality.
Keywords: developing country, IHCA, outcomes, predictors, survival
Introduction
In-hospital cardiac arrest (IHCA) is defined as cessation of cardiac activity, confirmed by the absence of signs of circulation, in a hospitalized patient who had a pulse at the time of admission.1 The estimated incidence of this condition in previous reports is about 1.6 per 1,000 admissions in the UK and 17.5 per 1,000 admissions in People’s Republic of China.2,3 Cardiopulmonary resuscitation (CPR) has been used as an attempt to intervene in this process.4 The outcome of CPR, however, remains poor, even if it is performed in a hospital where there are trained staff and equipment available. Previous reports have revealed the return of spontaneous circulation (ROSC) and survival rates to discharge of IHCA to be 15%–60% and 6.6%–37%, respectively.2–11 These vary due to diversity in terms of age, comorbidities, and study populations.2,3,12 No single factor predicted any of those short-term outcomes. They were actually associated with multiple factors – including age, gender, race, ethnicity, preexisting conditions, event interval and duration to perform CPR, type of arrhythmia, hospital location, early defibrillation, and postresuscitation care.2,3,11–13 There are several morbidity scores that are used such as the prearrest morbidity scores, the prognosis after resuscitation score, and the modified prearrest morbidity scores index.12,14,15 However, these scores have demonstrated poor predictive performance, with sensitivities ranging from 20% to 30%.12,14,15 The consequences of CPR among survivors with prolonged hypoxemia are related to functional and cognitive decline, resulting in burdens on caregivers and reduced quality of life.13 Thus, it is crucial that health-care teams and families consider the rational and moral aspects of the decision to perform CPR in patients with cardiac arrest.11–13,16
Even though patients with cardiac arrest usually survive to discharge, they have poorer long-term survival rates.4,17 Long-term outcome following IHCA has been studied as a better prognostic predictor than short-term outcome.18 Unfortunately, there has been limited research regarding this outcome and its predictors. Existing reports showed absolute survival rates at 1 year to be only 5%–12%.4,17 The factors associated with long-term survival were age, cardiac rhythm, and comorbidities.4 Older adults who identified as black, women, and with extensive neurologic deficits were readmitted at 1 year after hospital discharge at a greater rate than other older adults.18 Data about the epidemiology and prognostic factors for short- and long-term survival in Thailand are limited. Therefore, the primary objective of this study was to assess survival rates for IHCA survival at 1 year after cardiac arrest. The secondary objectives were to determine predictors associated with death at 1 year following cardiac arrest in long-term survival among patients with IHCA.
Methods
Study setting and patient population
This is a retrospective study of patients who were aged 18 years and older and had IHCA and in whom CPR was attempted at Srinagarind Hospital from January 1, 2013 to December 31, 2014. Patients were excluded if they had subsequent episodes of cardiac arrest during the same hospital admission or if their medical records were unavailable.
Data collection
Demographic and clinical variables prearrest, intra-arrest, and postarrest were obtained from the CPR unit’s cardiac arrest records and civil registration records.
They included age, sex, type of ward, length of stay, reason for admission, comorbid diseases, prearrest cardiac rhythm, homebound status, use of mechanical ventilation, whether the arrest was witnessed, pre- and postarrest mental status, latest blood chemistry (blood urea nitrogen/creatinine, electrolytes) before cardiac arrest, duration of CPR, total dosage of epinephrine, presence of pupillary reflex postarrest, ROSC, and survival at discharge, 7 days after discharge, 30 days, 6 months, and 1 year after cardiac arrest. Survival at discharge might not reflect the true survival status due to the fact that patients in this population were likely to return home if their chances of survival were low. We, thus, collected data regarding survival at 7 days postdischarge.
Definition
Sepsis was defined based on the Society of Critical Care Medicine/the European Society of Intensive Care Medicine task force as life-threatening organ dysfunction caused by a dysregulated host response to infection.19
Pneumonia was defined as an infection of pulmonary parenchyma by various pathogens, not a single disease. The following clinical categories were identified: community-acquired, nosocomial, and aspiration pneumonia.20
Statistical analysis
Demographic data and clinical variables were analyzed using descriptive statistics and were presented as percentage, mean, and SD. If the distribution of these data did not conform to normal distribution, medians and interquartile ranges were used instead. A Kaplan–Meier plot was used to estimate the survival of the study population. Predictors of survival at 1 year after cardiac arrest were analyzed using univariate analysis. Crude hazard ratio and 95% CI were used to show the level of association. Factors were then entered into a multiple Cox regression model. An initial multivariable model and then purposeful selection with backward elimination were used to analyze the outcomes. Assessment of survival model adequacy was divided into five steps. The first step was verification of statistical significance of covariates. Then, Cox proportional hazard model-specific assumptions were examined. Poorly fit and influential subjects were identified in the next step. Finally, an overall goodness-of-fit test was performed to determine of the final models. A p-value <0.05 according to a partial likelihood ratio test was considered to indicate statistically significant differences. Strength of association was reported as adjusted hazard ratios and their 95% CI. All data analysis was carried out using STATA version 10.0 (StataCorp, College Station, TX, USA).
Ethical approval was provided by the Khon Kaen University Faculty of Medicine ethics committee as instituted by the Helsinki Declaration. The reference number was HE581210. Since the study design was a retrospective chart review, patient consent to review their medical records was not required. Anonymous patients’ information was used for patients’ privacy protection.
Results
Characteristics of the study population and survival time
There were 278 cardiac arrest patients who received CPR during the study period which included both in- and out-hospital cardiac arrest. A total of 202 patients who received cardiopulmonary resuscitation met the inclusion criteria. Table 1 shows the demographics and survival times of the cardiac arrest patients. The median age of the patients was 59 years, and the number of women was slightly higher than that of men. The majority of the patients were in the general ward, followed by the intensive care unit. Infection was the top reason for admission. About 40% of patients had a history of hypertension and about 30% had diabetes. Pulseless electrical activity was the most frequent cause of arrest, followed by asystole and ventricular tachycardia/ventricular fibrillation (VT/VF). The median duration of CPR was 15 minutes. Approximately 60% of patients had ROSC following CPR, about 24% survived to discharge from the hospital and 8% survived to 1 year. The 1-year survival rate of the arrest survivors post hospital discharge was 72.9% (35 out of 48 cases). Figure 1 demonstrates the Kaplan–Meier curve of survivors at 7 days after cardiac arrest.
  | Figure 1 Kaplan–Meier curve of survivors at 7 days after cardiac arrest. |
Predictors of death at 1 year after cardiac arrest
Univariate analysis found that patients with comorbid hematologic malignancy and dementia, urine <800 cc/d, initial coma, hyponatremia, and serum HCO3<20 meq/L had increased risk of death, whereas factors such as VF/VT and other cardiac rhythms apart from asystole and pulseless electrical activity at presentation as opposed to asystole were associated with decreased mortality. In terms of intra- and postarrest factors, higher epinephrine dosage, coma at 72 hours postarrest, and absence of pupillary reflex increased risk of death, whereas infection appeared to be a protective factor (Table 2).
Final models were developed using multivariate analysis. Interaction effect and assessment of model adequacy to test proportional hazard assumption were performed. Influential and poorly fit subjects were identified. An overall goodness-of-fit test was then performed. Model A was the best-fit model that was used for prearrest prediction. The model included three factors: serum HCO3<20 meq/L, asystole, and urine <800 cc/d. Model B, which included both pre- and postarrest factors, was the best-fit model that was used for predicting mortality at 1 year after cardiac arrest. It included coma at 72 hours postarrest and absence of pupillary reflex, along with the three factors listed above (Table 3).
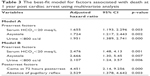  | Table 3 The best-fit model for factors associated with death at 1 year post cardiac arrest using multivariate analysis |
Discussion
The survival rates after resuscitation and discharge from the hospital in this study were comparable to the previous reports, among which ROSC varied from 15% to 60% and survival at discharge varied from 6.6% to 37%.1,2,4–11 However, in this report, these figures were rather low, which was probably due to the use of CPR in patients who had poor prognoses, such as those with metastatic cancer or other terminal illnesses. As shown above, around one-third of the patients had malignancy or sepsis. In addition, survival at discharge in this study might not reflect the true survival rates, most patients with low chances of survival opted to return home, as mentioned above. Survival at 7 days after discharge from the hospital was more likely to reflect the actual short-term outcome. Nevertheless, the figures (about 18%) were similar to those from previous reports.1,2,7–11 The period after discharge in which patients were the most vulnerable in this study was the first 7 days. According to previous reports, most patients die within 30–90 days after discharge.17,18 Differences in patient characteristics could influence the period in which patients are most susceptible. In this study, a greater proportion of patients were admitted due to noncardiac causes and nonshockable cardiac rhythm than in previous reports.17,18 These two factors have been reported as independent predictors of death at hospital discharge in several studies.12,21,22
This study is the first report from Asia to examine the long-term outcomes of IHCA patients after CPR. Only 8% of patients survived. The results of long-term follow-ups after IHCA may more accurately represent the prognosis of the patients than status at discharge.17,18 Of the patients who survived, the survival rate at 1 year post cardiac arrest was 72.9%, which was higher than the rates found in the majority of previous studies (58.5%–68%).4,17,18 One study, however, reported a survival rate of 86%.6 A possible explanation for this is that the studies with lower survival rates were conducted in older patients, as several studies have found age to be a predictor of death.9,12,21 The study that had highest survival rate included both younger and older adults.6 This may have meant the population was positively skewed toward having better a survival rate.
This study showed that both prearrest and postarrest factors were the important predictors after multivariate analysis. The majority of previous studies focused on factors associated with short-term survival, and there were few that included long-term factors.8,12,21,22 The varying results of previous reports make it clear that the predictors of IHCA are not universal.4,9,18 Some studies have shown advanced age and longer duration of CPR to be associated with mortality.4,9 The results of this study, however, support the findings that prearrest cardiac rhythm, comorbid conditions, and significant neurologic disability are related to survival.4,9 Consistent with several reports, patients with VF/VT had better prognoses than those with asystole,2,3,22 as asystole is typically a terminal arrest, meaning that chances of recovering are low. VF/VT reflects early arrest and can be treated promptly with defibrillation.2,22 Low serum HCO3 indicates acidosis, which could be the result of a variety of serious illnesses, such as lactic acidosis from sepsis and renal failure, which are factors know to be associated with mortality.4,9,12,23 Renal failure is also a frequent cause of mortality in hospitalized patients, which explains the association decreased urine volume with mortality found in this study.17 This study did not find an association between age and long-term outcomes. This may be explained by the differences in study population mentioned previously. The median age of patients in this study was 59 years (compared to that of 70 years in a previous study).9 Furthermore, differences in study setting could be as issue as that prior study included only intensive care unit patients, in whom disease is likely to be more severe. In addition, patients with comorbid hematologic malignancy and dementia showed significant association with death at 1 year. However, they failed to show the association when using multivariate analyses.
According to our results, Model A is useful in predicting patient prognosis before they receive CPR in order to avoid futile resuscitation, and Model B is helpful in determining prognosis prior to hospital discharge as they use common factors in clinical practice. Simple risk models to predict long-term mortality with good discrimination should be then developed. Information regarding prognosis should be shared with allied health care members, family members, and the patient him/herself (if possible) as a part of the decision-making process on the basis of patient center to abstain from prolonged inevitable death.12 Further study regarding the validation each model’s usefulness is advised.
There were some limitations in this study. First, it is a single-setting analysis of long-term survival following IHCA. Therefore, it might not be generalizable to different settings. Second, actual functional status, such as neurological outcomes, activities of daily living, and quality of life post cardiac arrest, was not measured in this study. Third, due to the nature of retrospective study, data from charts or CPR records, such as known predictors of mortality (like activities of daily living), might be lost or incomplete. Lastly, the majority of the patients died in the first 7 days post cardiac arrest. Factors associated with long-term survival might not represent the actual fact while investigating periarrest factors in patients who survived to hospital discharge might be a better approach.
Conclusion
IHCA has poor long-term outcomes. Only about 7.9% of patients survived for 1 year after cardiac arrest. Survival at discharge might not be a good endpoint to determine the effectiveness of CPR. Prearrest factors (serum HCO3<20 meq/L, asystole and urine <800 cc/d) and postarrest factors (coma at 72 hours postarrest and absence of pupillary reflex) were independent outcome predictors for long-term mortality. Further studies to develop practical predictive models and validate the performance of these models are recommended for using as part of the decision-making process with regard to CPR, which should take into account individual outcomes and patient preference.
Acknowledgments
We would like to acknowledge Dylan Southard (Research Affairs, Faculty of Medicine, Khon Kaen University, Thailand) for editing the manuscript. This manuscript was funded by the Sleep Apnea Research Group (Khon Kaen University, Thailand) and the Thailand Research Fund (number IRG 5780016).
Disclosure
The authors report no conflicts of interest in this work.
References
Tirkkonen J, Hellevuo H, Olkkola KT, Hoppu S. Aetiology of in-hospital cardiac arrest on general wards. Resuscitation. 2016;107:19–24. | ||
Nolan JP, Soar J, Smith GB, et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation. 2014;85(8):987–992. | ||
Shao F, Li CS, Liang LR, et al. Incidence and outcome of adult in-hospital cardiac arrest in Beijing, China. Resuscitation. 2016;102:51–56. | ||
Bloom HL, Shukrullah I, Cuellar JR, Lloyd MS, Dudley SC Jr, Zafari AM. Long-term survival after successful in hospital cardiac arrest resuscitation. Am Heart J. 2007;153(5):831–836. | ||
Song W, Chen S, Liu YS, Mo DF, Lan BQ, Gao YS. A prospective investigation into the epidemiology of in-hospital cardiopulmonary resuscitation using the international Utstein reporting style. Hong Kong J Emerg Med. 2011;18(6):391–396. | ||
Fredriksson M, Aune S, Thoren AB, Herlitz J. In-hospital cardiac arrest – an Utstein style report of seven years experience from the Sahlgrenska University Hospital. Resuscitation. 2006;68:351–358. | ||
Lidhoo P. Evaluating the effectiveness of CPR for in-hospital cardiac arrest. Am J Hosp Palliat Care. 2013;30(3):279–282. | ||
Krittayaphong R, Saengsung P, Chawaruechai T, Yindeengam A, Udompunturak S. Factors predicting outcome of cardiopulmonary resuscitation in a developing country: the Siriraj cardiopulmonary resuscitation registry. J Med Assoc Thai. 2009;92(5):618–623. | ||
Kutsogiannis DJ, Bagshaw SM, Laing B, Brindley PG. Predictors of survival after cardiac or respiratory arrest in critical care units. CMAJ. 2011;183(14):1589–1595. | ||
Chan JC, Wong TW, Graham CA. Factors associated with survival after in-hospital cardiac arrest in Hong Kong. Am J Emerg Med. 2013;31(5):883–885. | ||
Limpawattana P, Siriussawakul A, Chandavimol M, et al. National data of CPR procedures performed on hospitalized Thai older population patient. Int J Gerontol. 2015;9(2):67–70. | ||
Ebell MH, Afonso AM. Pre-arrest predictors of failure to survive after in-hospital cardiopulmonary resuscitation: a meta-analysis. Fam Pract. 2011;28(5):505–515. | ||
Chang WH, Huang CH, Chien DK, Su YJ, Lin PC, Tsai CH. Factors analysis of cardiopulmonary resuscitation outcomes in the elderly in Taiwan. Int J Gerontol. 2009;3:16–25. | ||
Bowker L, Stewart K. Predicting unsuccessful cardiopulmonary resuscitation (CPR): a comparison of three morbidity scores. Resuscitation. 1999;40(2):89–95. | ||
Cohn EB, Lefevre F, Yarnold PR, Arron MJ, Martin GJ. Predicting survival from in-hospital CPR: meta-analysis and validation of a prediction model. J Gen Intern Med. 1993;8(7):347–353. | ||
Mohr M, Kettler D. Ethical aspects of resuscitation. Br J Anaesth. 1997;79(2):253–259. | ||
Feingold P, Mina MJ, Burke RM, et al. Long-term survival following in-hospital cardiac arrest: a matched cohort study. Resuscitation. 2016;99:72–78. | ||
Chan PS, Nallamothu BK, Krumholz HM, et al. Long-term outcomes in elderly survivors of in-hospital cardiac arrest. N Engl J Med. 2013;368(11):1019–1026. | ||
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–810. | ||
Levison ME. Pneumonia, including necrotizing pulmonary infections (lung abscess). In: Braunwald E, Fauci AS, Hauser SL, Longo DL, Kasper DL, Jameson JL, editors. Harrison’s Principles of Internal Medicine. 15th ed. New York, NY: McGraw-Hill; 2001:1475–1484. | ||
Taffet GE, Teasdale TA, Luchi RJ. In-hospital cardiopulmonary resuscitation. JAMA. 1988;260(14):2069–2072. | ||
Brindley PG, Markland DM, Mayers I, Kutsogiannis DJ. Predictors of survival following in-hospital adult cardiopulmonary resuscitation. CMAJ. 2002;167(4):343–348. | ||
Suraseranivongse S, Chawaruechai T, Saengsung P, Komoltri C. Outcome of cardiopulmonary resuscitation in a 2300-bed hospital in a developing country. Resuscitation. 2006;71(2):188–193. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


