Back to Journals » Journal of Pain Research » Volume 15
Long-Term Follow-Up of Patients with Neck Pain Associated with Ossification of the Posterior Longitudinal Ligament Treated with Integrative Complementary and Alternative Medicine: A Retrospective Analysis and Questionnaire Survey
Authors Namgoong J, Lee YH, Ju AR, Chai J, Choi D, Choi HJ, Seo JY , Park KS, Lee YJ , Lee J, Ha IH
Received 29 December 2021
Accepted for publication 11 May 2022
Published 24 May 2022 Volume 2022:15 Pages 1527—1541
DOI https://doi.org/10.2147/JPR.S356280
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Houman Danesh
Jin Namgoong,1 Yun-Ha Lee,1 Ah Ra Ju,1 Jiwon Chai,1 DongJoo Choi,1 Hyo Jung Choi,1 Ji-Yeon Seo,1 Kyoung Sun Park,2 Yoon Jae Lee,1,3 Jinho Lee,2 In-Hyuk Ha1,3
1Bucheon Jaseng Hospital of Korean Medicine, 414 KR in Sangdong, Bucheon-si, Gyeonggi-do, Republic of Korea; 2Jaseng Hospital of Korean Medicine, Seoul, Republic of Korea; 3Jaseng Spine and Joint Research Institute, Jaseng Medical Foundation, Seoul, Republic of Korea
Correspondence: In-Hyuk Ha, Jaseng Spine and Joint Research Institute, Jaseng Medical Foundation, 3F JS Tower, 538 Gangnam-daero, Gangnam-gu, Seoul, 06110, Republic of Korea, Tel +82 2 2222 2740, Fax +82 2 3218 2244, Email [email protected]
Purpose: Integrative Korean medicine treatment (KMT) is a conservative treatment approach for the ossification of the posterior longitudinal ligament (OPLL) in Korea; nonetheless, relevant studies focusing on KMT for OPLL are lacking. A multicenter retrospective analysis of patient medical records and a questionnaire survey were conducted to investigate the effectiveness of integrative KMT in patients with OPLL treated for neck pain.
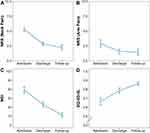
Patients and Methods: A total of 78 inpatients radiologically diagnosed with OPLL and treated for neck pain at four Korean medicine hospitals from April 1, 2016, to December 31, 2019, were enrolled. The primary index was an improvement in the numeric rating scale (NRS) score for neck pain, whereas the secondary outcome indices were improvements in the NRS score for arm pain, neck disability index (NDI) score, and EuroQol 5-dimension 5-level (EQ-5D-5L) score.
Results: At discharge, the NRS score for neck pain, NRS score for arm pain, and NDI score decreased by 2.47 (95% confidence interval [CI], − 2.81 to − 2.14), 1.32 (95% CI, − 1.73 to − 0.91), and 16.02 (95% CI, − 18.89 to − 13.15), respectively, as compared with the scores at admission (p < 0.001). The EQ-5D-5L score increased by 0.12 (95% CI, 0.09 to 0.16) as compared with the score at admission (p < 0.001). This trend was also evident during follow-up. With respect to Patient Global Impression of Change evaluation, 33 (61.1%) patients claimed to have very much improved, whereas 17 (31.5%) patients reported to have much improved.
Conclusion: Inpatients with OPLL who received integrative KMT showed improvements in neck pain, arm pain, the NDI, and quality of life, which were retained throughout the follow-up period.
Keywords: integrative medicine, Korean medicine, OPLL, neck pain
Introduction
Ossification of the posterior longitudinal ligament (OPLL) is a form of hyperostosis that can induce serious neurological disabilities1 and most commonly affects the cervical spine.2,3 OPLL symptoms include neck pain, arm pain, sensory abnormalities, muscle weakness, and bladder disturbance, with most symptoms manifesting gradually.4 The causes of OPLL remain unclear but are likely multifactorial, as OPLL is known to be associated with age, family history, environment, lifestyle, hormonal levels, and history of hypertension, diabetes mellitus, thyroid diseases, and osteoporosis.3–5 It is more prevalent among Asians than among Europeans and Americans, and its incidence ranges from 1.9% to 4.3% in Japan, where the condition was first described.1 OPLL can be categorized into continuous, segmental, mixed, and local types.4 A Korean study involving 3240 adults reported an incidence of approximately 4.6% for OPLL and confirmed that it was more common among men and adults aged ≥70 years.
OPLL treatments include conservative and surgical approaches. Surgical treatment is performed for cases of severe myelopathy caused by OPLL.6 The decision to perform surgery and the choice of surgical technique are determined depending on the symptom severity, patient’s status, surgeon’s experience, spinal curvature, presence of the K-line, and the size, level, and type of OPLL.3,7–9 On the other hand, conservative treatments for OPLL include fixation of the affected area using braces, traction, bed rest, and physiotherapy.10
Integrative Korean medicine treatment (KMT) is also performed in Korea as a form of conservative treatment for OPLL. However, relevant studies on the effectiveness of integrative KMT for OPLL are scarce. Relevant studies in literature mainly consist of case reports.11–19 The KMT described in these case reports included acupuncture, herbal medicine, moxibustion, Chuna therapy, and pharmacopuncture. Nonetheless, clinical studies, such as observational studies and randomized clinical trials, are lacking.
Considering this background, we conducted a retrospective observational study on inpatients who received treatment for neck pain caused by OPLL. Our aim was to investigate the effectiveness and safety of integrative KMT for OPLL.
Materials and Methods
Study Design
Jaseng is a Korean medicine hospital, which specializes in spinal disorders, that is accredited and designated by the Korean Ministry of Health and Welfare. The study data were collected from four branches, in Gangnam, Bucheon, Daejeon, and Haewoondae.
The present study was a retrospective observational study. Among all patients hospitalized for neck pain from April 1, 2016, to December 31, 2019, only those diagnosed with OPLL based on imaging, such as X-ray, magnetic resonance imaging (MRI), and computed tomography (CT), were enrolled in this study. The radiological findings were interpreted by a radiologist.
Review of Medical Records
Data on age, sex, date of onset, length of hospital stay, diagnosis, height, body weight, body mass index (BMI), obesity, smoking status, alcohol use and types, and frequency and duration of treatment administered during the hospital stay were collected from electronic medical records (EMRs). The numeric rating scale (NRS) scores for neck and arm pain, neck disability index (NDI) score, and EuroQol 5-dimension 5-level (EQ-5D-5L) score at admission and discharge were recorded. Patient EMRs during the hospital stay (eg, admission record, discharge record, progress record, and adverse event [AE] record) were retrospectively analyzed to determine the site and type of OPLL, K-line, presence and site of a herniated intervertebral disc (HIVD), underlying disease at admission, and AEs. Furthermore, results of the manual muscle test and sensory test at admission and discharge were reviewed. Arm muscle impairment and levels of elbow flexion, elbow extension, wrist flexion, and wrist extension were evaluated using the manual muscle test. The degree of sensory abnormality was classified as sluggish, normal, and hyperactive using the sensory test. For the assessment of the range of motion (ROM) of neck, flexion, extension, lateral bending, and rotation were evaluated.
Phone Survey
During follow-up, the NRS, NDI, and EQ-5D-5L scores were re-assessed. In addition to the outcomes described above, the following data were surveyed: timing of surgery; postoperative progress; whether patients were referred for cervical surgery or had undergone surgery; whether they were diagnosed with concomitant disease; whether they used analgesics; whether they received treatment for neck pain in the past 3 months, as well as the type and duration of treatment; and whether they were referred for surgery before or after discharge. Furthermore, the Patient Global Impression of Change (PGIC) and satisfaction with KMT were assessed immediately after discharge.
Patients
The inclusion criteria were as follows: 1) diagnosis of OPLL based on radiological findings (eg, radiography, MRI, and CT findings) as recorded in EMRs; and 2) hospitalization with neck pain as the chief complaint.
The exclusion criteria were as follows: 1) length of hospital stay ≤3 days; 2) hospitalized for neck pain due to whiplash injury (automobile accident); 3) other chronic diseases that could hinder the interpretation of therapeutic effects or outcomes (eg, cardiovascular disease, renal disease, diabetic neuropathy, dementia, and epilepsy); 4) pain caused by soft tissue diseases and not a spinal disorder (eg, tumor, fibromyalgia, rheumatoid arthritis, and gout); 5) <3 months since undergoing cervical surgery; 6) cervical fracture identified on imaging; 7) patients unsuitable for study participation as deemed by the researcher; and 8) patients who declined to participate in the study.
Treatment
Inpatients received integrative KMT, including herbal medicine, acupuncture, pharmacopuncture, Chuna therapy, moxibustion, cupping, herbal hot pack, and traction treatments. Patients were permitted to receive any other treatments at the discretion of the Korean medicine doctor (KMD) or when needed. All treatments performed during the hospital stay were recorded in the EMRs.
Outcome Measures
All tests and surveys were performed at admission, discharge, and follow-up by trained KMDs to ensure consistency in measurements.
Primary Outcome
NRS Score for Neck Pain
The NRS is an instrument used for objectively quantifying subjective pain on a scale from 0 (no pain at all) to 10 (worst pain imaginable).20,21 In this study, the NRS score for neck pain was used as the primary outcome.
Secondary Outcomes
NRS Score for Arm Pain
When OPLL progresses and compresses some cervical nerves, pain, tingling, and sensory abnormalities can be felt at the dermatomes in the arm. Radiating pain in the arm was measured using the NRS.
NDI Score
The NDI is an instrument used for assessing neck and cervical functional impairment and consists of 10 items, with each item rated on a scale from 0 to 5. The total possible score is 50, with a higher score being indicative of more severe impairment in activities of daily living.22,23
EQ-5D-5L Score
The EQ-5D-5L is a health questionnaire used to measure health status and quality of life. The tool comprises five domains: mobility, self-care, usual activities, pain and discomfort, anxiety, and depression. Each item is rated on a scale from 1 (no problem) to 5 (unresolvable problem), and a score of 1 is given for a perfectly healthy state with no problems in any of the domains.24,25
PGIC Score
The PGIC is a self-report instrument used by patients to rate their perceived improvement (1: very much improved; 2: much improved; 3: minimally improved; 4: no change; 5: minimally worse; 6: much worse; and 7: very much worse). Although the PGIC was developed to assess psychological factors, it is now widely used in medicine to determine the level of pain relief achieved.26
AEs
Any AE was reported to healthcare providers during the hospital stay. In accordance with the three grades given by Spilker et al.,27 AEs were recorded every 7 AM by interviewing the patient. Moreover, the on-call doctor recorded any additional AEs for all inpatients. The relationship between treatment and AEs was classified according to the World Health Organization-Uppsala Monitoring Centre system into certain, probable/likely, possible, unlikely, conditional/unclassified, and not assessable/unclassifiable.28
Ethical Statement
This study was approved by the author’s Institutional Review Board (JASENG 2020-05-009) and was registered at ClinicalTrials.gov (NCT04446221). The requirement for a signed written consent form was waived due to the nature of the study, which is a telephone survey. Instead, all patients provided verbal informed consent. When patients refused to provide consent or withdrew their consent, their personal information was immediately removed and discarded from the study.
Statistical Analysis
Baseline characteristics and baseline outcomes of the enrolled patients were presented as means and standard deviations (SDs) for continuous variables and as frequencies and percentages for categorical variables. The details of treatment during the hospital stay were described as the number and percentage of patients for each type of treatment, and the frequency of treatment was presented as mean ± SD and median (first quartile to third quartile).
The outcomes at each time point were presented as mean ± SD, and the amount of change from the baseline value was presented as mean with 95% confidence interval (CI). The amount of change over time was assessed using a mixed linear model. The time of measurement was considered a categorical variable and was included in the model as a fixed effect along with the baseline value of each outcome. The subject was included as a random effect. The results are presented with 95% CI.
The minimal clinically important difference (MCID) was set as 1.5 for the NRS score for neck and arm pain,29 3.5 for the NDI score,30 and 0.074 for the EQ-5D-5L score.31 The number (N) and percentage of patients achieving the MCID were presented. The achievement of MCID was determined using a multivariate logistic regression model that included age, sex, onset, obesity, smoking, alcohol use, type of OPLL, onset mode, disc herniation, NRS scores for neck and arm pain, as well as the NDI and EQ-5D-5L scores at admission. The results were presented as odds ratios (ORs) with 95% CI. The goodness of fit was presented as the area under the receiver operating characteristic curve (AUC).
For patients who completed the long-term follow-up, the results obtained at follow-up were presented as mean ± SD and median (first quartile to third quartile) for continuous variables and as frequencies and percentages for categorical variables.
For sensitivity analysis, multiple imputation with 20 imputed sets was performed. A mixed linear model and logistic regression were used. Statistical significance was set at a p-value of <0.05. Statistical analyses were performed using RStudio version 1.1.463 (2009–2018, RStudio Inc., Boston, MA, USA).
Results
Study Flow
Among 5605 patients admitted to one out of the four Korean medicine hospitals for neck pain from April 1, 2016, to December 31, 2019, 170 were diagnosed with cervical OPLL based on cervical spine X-ray, MRI, or CT findings. Among these, 92 patients were excluded as per the inclusion and exclusion criteria, resulting in a total of 78 patients included in the analysis. A follow-up using a telephone was performed by a KMD from July to August 2020. Overall, 24 patients, who did not answer the telephone or refused to participate in the follow-up survey were excluded; therefore, only the data of 54 patients were analyzed (Figure 1).
Baseline Characteristics
The mean age of the 78 participating patients was 54.3 ± 9.0 years, while 32 (41.0%) participants were ≥50 years of age. There were more male (n = 41, 52.6%) than female patients, and the most common duration of hospital stay ranged from 2 weeks to <1 month (n = 34, 43.6%). Based on BMI, 37 (47.4%) patients were obese (≥25 kg/m2). The most common type of OPLL was segmental (n = 53, 67.9%).32 Four (5.1%) patients did not have a K-line. Fifty-eight patients presented with a HIVD (74.4%), which was defined as an abnormal protrusion.33 Six (7.7%) patients did not undergo MRI for financial reasons or because of the physician’s decision. The underlying diseases speculated to be associated with the onset of OPLL5 included hypertension (n = 22, 28.2%), diabetes mellitus (n = 17, 21.8%), osteoporosis (n = 1, 1.3%), thyroidism (n = 1, 1.3%), and ischemic stroke (n = 2, 2.6%) (Table 1).
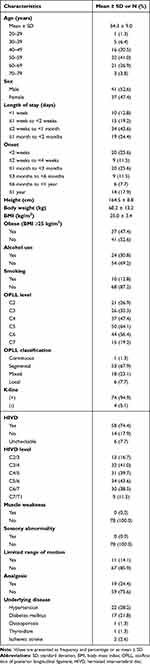 |
Table 1 Baseline Characteristics of the Study Population (n = 78) |
Changes in Outcome Measures
The NRS score for neck pain was 5.28 upon admission (95% CI, 4.97 to 5.60), which decreased by 2.47 upon discharge (95% CI, −2.81 to −2.14). Moreover, it was 3.11 upon follow-up (95% CI, −3.48 to −2.73). The NRS score for arm pain and NDI score decreased by 1.87 (95% CI, −2.32 to −1.42) and 27.91 (95% CI, −31.09 to −24.74) upon follow-up, respectively. On the other hand, the EQ-5D-5L score increased by 0.20 (95% CI, 0.16 to 0.23) upon follow-up (Table 2, Figure 2). The results were consistent in the sensitivity analysis using multiple imputation (Supplementary Table 1).
 |
Table 2 Change in Values After Treatment (n = 78) |
Among 11 patients who presented with limited ROM upon admission, six had fully recovered ROM upon discharge. Three out of five patients still presented with a 10–15° ROM limitation compared with the normal angle upon discharge. They had limitations in right rotation, extension, and extension and both rotations. One patient presented with limited ROM upon discharge but showed ROM recovery upon follow-up. The other patient had 20° limitation in flexion and extension and 30° limitation in side bending upon admission, and no improvements were observed upon discharge. However, it was difficult to perform an accurate ROM test because the patient was psychologically anxious about moving the neck following screw fixation at C3–6 due to OPLL in 2016.
Achievement of the MCID
Table 3 shows the prediction of achievement of the MCID for each outcome measure. Fifty-eight (74.4%) patients achieved the MCID for the NRS score upon discharge, whereas 42 (77.8%) patients achieved it upon follow-up. The number of patients who achieved the MCID for the NDI score was 57 (73.1%) upon discharge and 51 (94.4%) upon follow-up. Moreover, the number of patients who achieved the MCID for the EQ-5D-5L score was 43 (55.1%) upon discharge and 38 (70.4%) upon follow-up.
 |
Table 3 Prediction of the Achievement of the MCID for Each Indicator |
With respect to predictors of the achievement of the MCID, the OR for achieving the MCID for the NRS score upon discharge was 5.18 (95% CI, 1.12 to 24.1) in patients with a chronic condition. Patients with a high NRS score upon admission had higher MCID achievement. The OR for achieving the MCID was 4.08 (95% CI, 1.88 to 8.84) upon discharge and 2.37 (95% CI, 1.18 to 4.77) upon follow-up. Furthermore, the OR for achieving the MCID for the NDI score upon discharge was 1.08 (95% CI, 1.03 to 1.14). As for the EQ-5D-5L score, the OR for achieving the MCID was 0.86 (95% CI, 0.8 to 0.93) upon discharge and 0.84 (95% CI, 0.73 to 0.95) upon follow-up. Age, obesity, and chronic state were significantly associated with the achievement of the MCID but were not significant in the sensitivity analysis using multiple imputation (Supplementary Table 2).
Treatment
Inpatient treatments included acupuncture, herbal medicine, cupping, moxibustion, pharmacopuncture, traction, Chuna therapy, herbal hot pack, manual therapy, and western pharmacological treatment. Herbal therapy regimens consisted of taking pills (2 g) or prepared oral liquid medicine (120 mL) twice or three times per day after meals from the day of admission to the day of discharge. Acupuncture therapy was performed by inserting disposable standardized stainless-steel needles (40 × 0.25 mm, Dong-bang Acupuncture, Seongnam, Korea) into the acupuncture points related to the pain sites. It was performed twice a day in the morning and afternoon, with 15 min of needle retention and electrostimulation. Pharmacopuncture was performed using standardized disposable syringes (1 mL, 26G × 1.5-mL syringe; Shinchang Medical Co., Gumi, Korea). Shinbaro pharmacopuncture solution (2 mL; Jaseng Herbal Medicine Dispensary, Namyangju, Korea), Bee Venom pharmacopuncture solution (2 mL; Jaseng Herbal Medicine Dispensary, Namyangju, Korea), Hominis Placenta pharmacopuncture solution (2 mL; Jaseng Herbal Medicine Dispensary, Namyangju, Korea), or Hwangryunhaedok-tang pharmacopuncture solution (2 mL; Jaseng Herbal Medicine Dispensary, Namyangju, Korea) was subcutaneously injected once or twice a day before acupuncture treatment. Chuna therapy was provided by a KMD who had completed the formal Chuna training curriculum, and the method and frequency were also determined by the treating KMD.
Other treatments included moxibustion, cupping, herbal hot pack, and traction. Moxibustion and cupping therapies were performed as necessary by the treating KMD on the corresponding meridians and pain sites at the time of acupuncture. Herbal hot pack therapy was performed by placing a heating pad steamed with geoseup-hwalhyeoljitong-tang on the affected area (posterior cervical, cervico-thoracic junction) in the supine position. Traction therapy, which alleviates radiating pain by widening the internal disc space, was performed on the affected segments after imaging tests.
Acupuncture and herbal medicine were prescribed to all patients, with a mean frequency of 38.9 ± 24.0 sessions and 22.3 ± 14.3 days, respectively. Pharmacopuncture, cupping, and Chuna manual therapy were provided to 77 (98.7%), 77 (98.7%), and 71 (91.0%) patients, with a mean frequency of 35.3 ± 24.6, 37.8 ± 23.9, and 17.7 ± 13.9 sessions, respectively (Supplementary Table 3).
AEs
In total, 16 cases of AEs were reported among 14 patients during their hospital stay. All AEs were gastrointestinal symptoms, with 11 cases of indigestion and five cases of diarrhea. Two of the 14 patients had both symptoms. All reported AEs were mild. Thirteen cases were resolved with herbal medicine, and one case spontaneously resolved without any further treatment.
Follow-Up Survey
The results of the follow-up survey are shown in Table 4. Ten patients stated that they had no underlying disease at the time of admission but subsequently developed diseases, including hypertension (n = 3), diabetes mellitus (n = 2), osteoporosis (n = 1), thyroidism (n = 1), and ischemic stroke (n = 3).
 |
Table 4 Results of the Follow-Up Survey (n = 54) |
According to 13 patients, they were referred for surgery by a different healthcare facility prior to admission. Ten of these patients were referred for surgery for cervical HIVD, while seven of these patients were referred for surgery for cervical OPLL. One of these patients underwent cervico-thoracic screw fixation, since he/she had both HIVD and OPLL. Three patients underwent surgery after discharge. Two of these patients underwent surgery for OPLL, while the other patient underwent cervical surgery. However, the details on the type of surgery were not available.
Twelve patients indicated that they had received cervical pain treatment in the past 3 months, with the duration of treatment ranging from 1 to 50 days. The treatment included acupuncture (n = 10), cupping (n = 8), herbal medicine (n = 7), pharmacopuncture (n = 7), physiotherapy (n = 5), manual therapy (n = 5), Chuna therapy (n = 4), and moxibustion (n = 4).
With respect to PGIC evaluation, 33 patients reported that their condition very much improved, whereas 17 patients reported that their condition improved much. On the other hand, 4 patients reported that there was only little improvement.
Discussion
This study was conducted on patients hospitalized in a Korean medical hospital for neck pain, who were later diagnosed with OPLL based on radiological findings. Most patients complained of moderate or more severe pain at the time of admission but exhibited significant changes in NRS, NDI, and EQ-5D-5L scores upon discharge. We confirmed that improvements in pain perception, functional state, and quality of life were retained in the long run, and we further examined patients’ satisfaction with KMT through a follow-up using a telephone.
The prevalence of OPLL varies among racial groups but is known to be higher among Asians. A study involving 3161 inpatients in the USA during a 4-year period confirmed differences in the prevalence across races, with 1.3% in Caucasian Americans, 4.8% in Asian Americans, 1.9% in Hispanic Americans, 2.1% in African Americans, and 3.2% in native Americans.34 Additionally, the prevalence of OPLL among outpatients was 1.5–2.4% in Japan, 1.0% in Korea, 1.5% in the Philippines, 2.1% in Taiwan, and 0.8% in Singapore. Based on health insurance data in a study on Japanese adults aged 30 years or older, the incidence rate ranged from 1.9% to 4.3%.1 The prevalence also varies according to the research method and study population. A study involving 20,057 outpatients in Korea reported a prevalence of 3.6%,35 whereas a study on 3240 individuals with no history of spinal disease reported an incidence of 4.6% for OPLL.36 In contrast, the prevalence was 0.19% in a study analyzing the national health insurance data from 2002 to 201337 and 0.60% in another study analyzing the radiography findings of 17,036 patients from a single university hospital.38 In this study, 170 out of 5605 outpatients and inpatients who underwent imaging tests for neck pain had OPLL, indicating a prevalence of 3.03%. The prevalence in our study is higher than that reported for the general population, presumably because our study was conducted on patients who visited a hospital for neck pain.
In the present study, 74.4% of the 78 participants had both OPLL and a cervical HIVD, as determined by MRI. The concurrent incidence of OPLL and HIVD varies depending on various factors. In previous studies that analyzed cases of surgery due to OPLL, 55.6% of 54 patients39 and 61% of 141 patients also had an HIVD.40 Among 142 patients, the rate was 18.3% in one study,41 which was probably lower because the HIVD was deemed to be present only when neurological symptoms were clearly caused by the HIVD. OPLL has been shown to contribute to the onset of an HIVD. Calcium accumulation in the posterior longitudinal ligament induces ossification and hyaline degeneration. This results in volume reduction of the ligament, thereby leading to abnormal mechanical stimulation in the surrounding disc.39 Furthermore, pathological changes in the posterior longitudinal ligament attached to the fibrous ring may increase disc protrusion or prolapse.41,42 Thus, OPLL can be considered to contribute to the onset of an HIVD. Moreover, a cervical HIVD is common among individuals with OPLL.39
In this study, there were different types of OPLL, including segmental (67.9%), continuous (1.3%), mixed (23.1%), and local (7.7%) types. A Korean study on 87 patients in a different hospital reported rates of 60% for the segmental type, 8% for the continuous type, 24% for the mixed type, and 8% for the local type among patients with neck pain only and radiating pain without cervical myelopathy.43 This shows a trend similar to that observed in this study. Conversely, the rates were 35% for the segmental type, 24% for the continuous type, 24% for the mixed type, and 15% for the local type among patients exhibiting symptoms of myelopathy. In cases of continuous OPLL spanning several segments, HIVD more commonly occurred between—as opposed to the top or bottom of—continuous ossifications.39 Moreover, patients who also presented with disc degeneration had a primarily segmental or local type of OPLL.40 Regarding the relationship between the type of OPLL and the incidence of an HIVD, an HIVD most frequently occurs with the segmental type. Although an HIVD does not induce this type of OPLL, patients with segmental-type OPLL have an elevated risk of an HIVD due to the increased fragility of the posterior longitudinal ligament and fibrous ring.39
Although OPLL symptoms gradually manifest,4 neck pain itself is often concomitant with other causes. In the present study, most patients were in the acute (35.9%; <1 month since onset) or subacute (37.2%; <6 months since onset) phase of neck pain, with a smaller proportion of patients in the chronic stage at 6 months or longer (11.7%) or 1 year or longer (18.2%) since onset. This study was conducted on inpatients; hence, it is likely that there were several patients who were hospitalized due to an acute onset of symptoms or recent exacerbation of symptoms. Although OPLL itself progresses chronically, trauma may facilitate the onset of OPLL symptoms.1 Moreover, many patients often present to a hospital after developing acute neck pain, which was presumed to contribute to the higher proportion of patients with acute or subacute onset. OPLL is a slowly progressing disease, and it is difficult to pinpoint the exact time of onset.
The NRS scores for neck and arm pain, NDI score, and EQ-5D-5L score significantly decreased upon discharge than the scores upon admission (p < 0.001), and the MCID for the NRS, NDI, and EQ-5D-5L was set at 1.5,29 3.5,30 and 0.074,31 respectively. At the long-term follow-up, achievement of the MCID for the NRS, NDI, and EQ-5D-5L was 77.8%, 94.4%, and 70.4%, respectively. The odds for achieving the MCID for each outcome measure were higher among those with higher NRS scores for neck pain and NDI scores upon admission, whereas the odds for achieving the MCID were lower among those with higher EQ-5D-5L scores upon admission. This may be attributable to the fact that patients with more severe symptoms would perceive a greater improvement as their symptoms improved.
Patients received integrative KMT consisting of acupuncture, herbal medicine, pharmacopuncture, Chuna therapy, cupping, application of herbal hot packs, moxibustion, and traction therapies during their hospital stay. Acupuncture is a treatment that stimulates acupuncture points and meridians to activate the endogenous pain control mechanism,44 and it is known to induce pain relief by regulating opioid, serotonin, and norepinephrine levels and inhibiting the activation of endogenous pain receptors, inflammatory cytokines, and the central nervous system.45 Cheongpa-jeon accounts for the greatest percentage of herbal medicine prescriptions and contains GCSB-5, which is a mixture of six herbs (Cibotii Rhizoma, Ledebouriellae Radix, Eucommiae Cortex, Acanthopanacis Cortex, Achyranthis Radix, and Glycine Semen). GCSB-5 has been confirmed to facilitate nerve46 and cartilage regeneration47 and to have anti-inflammatory effects48 in vivo and in vitro. Pharmacopuncture is a KMT that integrates herbal medicine with acupuncture, in which herbal medicine preparations are injected into acupuncture points to intensify the stimulation of acupuncture points and extend the duration of action.49 The pharmacopuncture preparations used in this study included Shinbaro, bee venom, hominis placenta, and Hwangryunhaedok-tang. The widely used Shinbaro pharmacopuncture is prepared by extracting and purifying herbal mixtures, such as Cibotii Rhizoma, Eucommiae Cortex, Acanthopanacis Cortex, Achyranthis Radix, Glycine Semen, Scolopendra subspinipes mutilans, Ostericum koreanum (Max.) Kitagawa, Aralia contientalis, and Paeonia lactiflora and it contains GCSB-5.50 Chuna therapy is a manual Korean medicine practice in which KMDs administer effective stimulation to a patient’s body using their hands, a part of their body, or a tool.51 This therapy induces biomechanical changes in which trapped meniscoids or distorted fibrous rings are corrected and vertebral motion is intensified with small forced movements, thereby reducing mechanical stress.52 The health insurance coverage for Chuna therapy began in April 2019, and this therapy is performed by KMDs who have successfully completed a formal Chuna training curriculum.
In this study, we performed a retrospective review of medical records and a follow-up survey using a telephone communication. This study had some limitations. First, there was no control group owing to the nature of a retrospective analysis. Second, the effects of individual treatment modalities could not be determined, since we examined integrative KMT. Third, there might have been recall bias in the result concerning the satisfaction with KMT because the patients had to recall their impressions at the time of their treatment during the hospital stay.
Despite these limitations, this study is significant as the first follow-up study on patients who received integrative KMT for OPLL. Nonsurgical treatment for OPLL is an important challenge in terms of improving the quality of life, and non-invasive KMT seems to be a good treatment option. This study established a study population comprising patients across four Korean medicine hospitals in Korea over a period of 3 years and 9 months, and the survey participation rate was high at 69.23%. Furthermore, we confirmed that integrative KMT effectively reduced pain and improved the functional state as well as the quality of life. Moreover, these improvements were maintained until follow-up. Accordingly, large-scale well-designed studies on patients with OPLL are necessary.
Conclusion
Integrative KMT reduced neck pain, radiating arm pain, and cervical functional impairment and improved the quality of life of patients hospitalized for OPLL, with improvements persisting even after discharge.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Ethics Approval and Informed Consent
This study complies with the Declaration of Helsinki, and was approved by the author’s Institutional Review Board (JASENG 2020-05-009). Due to the nature of the study involving a telephone survey, the requirement for a signed written consent form was waived, and all patients provided verbal informed consent (JASENG 2020-05-009). When a patient refused to consent or withdrew their consent, their personal information was immediately removed and discarded from the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HF21C0099).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Matsunaga S, Sakou T. Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine. 2012;37(5):E309–E314. doi:10.1097/BRS.0b013e318241ad33
2. Epstein N. Diagnosis and surgical management of cervical ossification of the posterior longitudinal ligament. Spine J. 2002;2(6):436–449. doi:10.1016/S1529-9430(02)00394-7
3. Saetia K, Cho D, Lee S, Kim DH, Kim SD. Ossification of the posterior longitudinal ligament: a review. Neurosurg Focus. 2011;30(3):E1. doi:10.3171/2010.11.FOCUS10276
4. Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res. 1984;184:71–84.
5. Shin J, Choi JY, Kim YW, Chang JS, Yoon SY. Quantification of risk factors for cervical ossification of the posterior longitudinal ligament in Korean populations: a nationwide population-based case-control study. Spine. 2019;44(16):E957–E964. doi:10.1097/BRS.0000000000003027
6. Masaki Y, Yamazaki M, Okawa A, et al. An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament: anterior decompression with spinal fusion versus laminoplasty. Clin Spine Surg. 2007;20(1):7–13.
7. Chiba K, Ogawa Y, Ishii K, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy− average 14-year follow-up study. Spine. 2006;31(26):2998–3005. doi:10.1097/01.brs.0000250307.78987.6b
8. Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: part 1: clinical results and limitations of laminoplasty. Spine. 2007;32(6):647–653. doi:10.1097/01.brs.0000257560.91147.86
9. Fujiyoshi T, Yamazaki M, Kawabe J, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine. 2008;33(26):E990–E993. doi:10.1097/BRS.0b013e318188b300
10. Pham MH, Attenello FJ, Lucas J, He S, Stapleton CJ, Hsieh PC. Conservative management of ossification of the posterior longitudinal ligament: a review. Neurosurg Focus. 2011;30(3):E2. doi:10.3171/2011.1.FOCUS10273
11. Hong M-W, Kim J-K, Park M-J, et al. A case report on ossification of posterior longitudinal ligament treated by Korean medicine: focusing on chuna therapy. J Korea CHUNA Manual Med Spine Nerves. 2020;15(1):135–145. doi:10.30581/jkcmm.2020.15.1.135
12. Jo M, Kim D, Kim S, Kim E, Jin J. A case report of ossification of posterior longitudinal ligament with cervical herniated intervertebral disc patient treated with Korean medical treatment. J Spine Joint Korean Med. 2018;15(1):17–23.
13. Kim M-Y, Park S-C, Kang S-H, Song Y-S, Shin B-C. A case report on the ossification of the posterior longitudinal ligament treated by CHUNA manual therapy. J Korea CHUNA Manual Med Spine Nerves. 2002;3(1):153–166.
14. Kim S-K, Seo W-H, Choi S-G, Moon I-R, Park J-T. Clinical studies on Ossification of posterior longitudinal ligament (OPLL). J Acupuncture Res. 2002;19(6):264–279.
15. Kim J-U, Choi S-Y, Hwang W-J, Lee S-H, Yoo I-S. Clinical studies on Ossification of ligaments within spinal canal-3 cases of OPLL and 3 cases of OLF. J Acupuncture Res. 2004;21(6):127–149.
16. Lee J-B, Lee H-Y, Cho Y-H, Jeong S-Y. A case report on cervical spinal stenosis with ossification of posterior longitudinal ligament applied chuna treatment. J Korea CHUNA Manual Med Spine Nerves. 2009;4(1):85–94.
17. Park S-W, Kim S-S, Yang S-B, Lee G-M. The clinical effects of acupotomy for ossification of the posterior longitudinal ligament. J Acupuncture Res. 2011;28(4):127–135.
18. Park J, Lee J, Yang H, et al. A case report of ossification of posterior longitudinal ligament with intervertebral disc calcification. J Spine Joint Korean Med. 2011;8(1):19–26. doi:10.3904/kjim.1993.8.1.19
19. Lee SM, Yoon KH, Lim JS, et al. A case report of cervical myelopathy caused by ossification of posterior longitudinal ligament: focusing on warm needling therapy. J Acupuncture Res. 2014;31(3):75–82. doi:10.13045/acupunct.2014045
20. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), McGill pain questionnaire (mpq), short-form McGill pain questionnaire (sf-mpq), chronic pain grade scale (CPGs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res. 2011;63(S11):S240–S252.
21. Solodiuk JC, Scott-Sutherland J, Meyers M, et al. Validation of the Individualized Numeric Rating Scale (INRS): a pain assessment tool for nonverbal children with intellectual disability. Pain. 2010;150(2):231–236. doi:10.1016/j.pain.2010.03.016
22. de Leon SP, Lara-Muñoz C, Feinstein AR, Wells CK. A comparison of three rating scales for measuring subjective phenomena in clinical research: II. Use of experimentally controlled visual stimuli. Arch Med Res. 2004;35(2):157–162. doi:10.1016/j.arcmed.2003.07.009
23. Song K-J, Choi B-W, Choi B-R, Seo G-B. Cross-cultural adaptation and validation of the Korean version of the neck disability index. Spine. 2010;35(20):E1045–E1049. doi:10.1097/BRS.0b013e3181df78e9
24. Kim S-H, Ahn J, Ock M, et al. The EQ-5D-5L valuation study in Korea. Qual Life Res. 2016;25(7):1845–1852. doi:10.1007/s11136-015-1205-2
25. Seong SS, Choi CB, Sung YK, et al. Health-related quality of life using EQ-5D in Koreans. J Korean Rheum Assoc. 2004;11(3):254–262.
26. Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1):9–19. doi:10.1016/j.pain.2004.09.012
27. Spilker B. Guide to Clinical Trials. Philadelphia: Lippincott-Raven; 1996:565–587.
28. Son M-K, Lee Y-W, Jung H-Y, et al. Comparison of the Naranjo and WHO-Uppsala Monitoring Centre criteria for causality assessment of adverse drug reactions. Korean J Med. 2008;74(2):181–187.
29. Kovacs FM, Abraira V, Royuela A, et al. Minimum detectable and minimal clinically important changes for pain in patients with nonspecific neck pain. BMC Musculoskelet Disord. 2008;9(1):43. doi:10.1186/1471-2474-9-43
30. Pool JJ, Ostelo RW, Hoving JL, Bouter LM, De Vet HC. Minimal clinically important change of the neck disability index and the numerical rating scale for patients with neck pain. Spine. 2007;32(26):3047–3051. doi:10.1097/BRS.0b013e31815cf75b
31. Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual life res. 2005;14(6):1523–1532. doi:10.1007/s11136-004-7713-0
32. Tetreault L, Nakashima H, Kato S, et al. A systematic review of classification systems for cervical ossification of the posterior longitudinal ligament. Global Spine J. 2019;9(1):85–103. doi:10.1177/2192568217720421
33. Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology: recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine. 2001;26(5):E93–E113. doi:10.1097/00007632-200103010-00006
34. Fujimori T, Le H, Hu SS, et al. Ossification of the posterior longitudinal ligament of the cervical spine in 3161 patients: a CT-based study. Spine. 2015;40(7):E394–E403. doi:10.1097/BRS.0000000000000791
35. Jin BH, Kim YS. Ossification of spinal ligaments. J Korean Neurosurg Soc. 1991;20(10–11):875–884.
36. Sohn S, Chung CK, Yun TJ, Sohn C-H. Epidemiological survey of ossification of the posterior longitudinal ligament in an adult Korean population: three-dimensional computed tomographic observation of 3240 cases. Calcif Tissue Int. 2014;94(6):613–620. doi:10.1007/s00223-014-9846-7
37. Shin J, Kim YW, Lee SG, Park E-C, Yoon SY. Cohort study of cervical ossification of posterior longitudinal ligament in a Korean populations: demographics of prevalence, surgical treatment, and disability. Clin Neurol Neurosurg. 2018;166:4–9. doi:10.1016/j.clineuro.2018.01.014
38. Kim T-J, Bae K-W, Uhm W-S, Kim T-H, Joo K-B, Jun J-B. Prevalence of ossification of the posterior longitudinal ligament of the cervical spine. Joint Bone Spine. 2008;75(4):471–474. doi:10.1016/j.jbspin.2007.07.019
39. Hanakita J, Suwa H, Namura S, Mizuno M, Ootsuka T, Asahi M. The significance of the cervical soft disc herniation in the ossification of the posterior longitudinal ligament. Spine. 1994;19(4):412–418. doi:10.1097/00007632-199402001-00006
40. Lee JK, Ham CH, Kwon W-K, et al. Classification for cervical ossification of the posterior longitudinal ligament based on the coexistence of segmental disc degeneration. J Korean Neurosurg Soc. 2021;64(1):69. doi:10.3340/jkns.2020.0080
41. Yang H-S, Chen D-Y, Lu X-H, et al. Choice of surgical approach for ossification of the posterior longitudinal ligament in combination with cervical disc hernia. Eur Spine J. 2010;19(3):494–501. doi:10.1007/s00586-009-1239-7
42. Tsuzuki N, Imai T, Hotta Y. Histopathological findings of the ossification of the posterior longitudinal ligament of the cervical spine and their significance (author’s transl). Nihon Seikeigeka Gakkai Zasshi. 1981;55(4):387–397.
43. Chang H, Song K, Kim H, Choi BW. Factors related to the development of myelopathy in patients with cervical ossification of the posterior longitudinal ligament. J Bone Joint Surg Br. 2012;94(7):946–949. doi:10.1302/0301-620X.94B7.29018
44. Coutaux A. Non-pharmacological treatments for pain relief: TENS and acupuncture. Joint Bone Spine. 2017;84(6):657–661. doi:10.1016/j.jbspin.2017.02.005
45. Lee I-S, Cheon S, Park J-Y. Central and peripheral mechanism of acupuncture analgesia on visceral pain: a systematic review. Evid Based Complement Alternat Med. 2019;2019:1–22. doi:10.1155/2019/1304152
46. Jun B-C, Kim E-S, Kim D-S, Kim T-H, J-Y K. Effectiveness of ShinBaro pharmacopuncture on lumbar spinal herniated intervertebral disc: a randomized controlled trial. J Korea CHUNA Manual Med Spine Nerves. 2011;6(2):109–119.
47. Kim J-K, Park S-W, Kang J-W, et al. Effect of GCSB-5, a herbal formulation, on monosodium iodoacetate-induced osteoarthritis in rats. Evid Based Complement Alternat Med. 2012;2012:1–11.
48. Chung H-J, Lee H-S, Shin J-S, et al. Modulation of acute and chronic inflammatory processes by a traditional medicine preparation GCSB-5 both in vitro and in vivo animal models. J Ethnopharmacol. 2010;130(3):450–459. doi:10.1016/j.jep.2010.05.020
49. Strudwick MW, Hinks RC, Choy SB. Point injection as an alternative acupuncture technique–an exploratory study of responses in healthy subjects. Acupuncture Med. 2007;25(4):166–174. doi:10.1136/aim.25.4.166
50. LeeIH KE, Kim MJ, Lee JW, Kim MR, Lee IH, Kim EJ. A study on standardization of shinbaro pharmacopuncture using herbal medicines identification test and HPLC-DAD. Acupuncture. 2015;32(2):1–9. doi:10.13045/acupunct.2015015
51. Park J-M, Shin S-W, Park J-H. A comparative study on the concepts of the Chuna. J Korean Med Classics. 2008;21(2):173–191.
52. Pickar JG. Neurophysiological effects of spinal manipulation. Spine J. 2002;2(5):357–371. doi:10.1016/S1529-9430(02)00400-X
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.