Back to Journals » Journal of Pain Research » Volume 15
Long-Term Follow-Up of Inpatients with Cervical Myelopathy Who Received Integrative Korean Medicine Treatment: A Retrospective Analysis and Questionnaire Survey Study
Authors Cho HW , Park JH, Yoo DH , Hwang DW, Kim SD, Kim ES, Park KS, Lee YJ , Lee J, Yang CS , Han CH , Ha IH
Received 9 November 2021
Accepted for publication 18 January 2022
Published 28 March 2022 Volume 2022:15 Pages 801—812
DOI https://doi.org/10.2147/JPR.S347410
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Houman Danesh
Hyun Woo Cho,1 Ju Hun Park,1 Dong Hwi Yoo,1 Dong Wook Hwang,1 Sang Don Kim,1 Eun-San Kim,2 Kyoung Sun Park,3 Yoon Jae Lee,2 Jinho Lee,3 Changsop Yang,4 Chang Hyun Han,4,5 In-Hyuk Ha2
1Haeundae Jaseng Hospital of Korean Medicine, Busan, 48102, Republic of Korea; 2Jaseng Spine and Joint Research Institute, Jaseng Medical Foundation, Seoul, 06110, Republic of Korea; 3Jaseng Hospital of Korean Medicine, Seoul, 06110, Republic of Korea; 4KM Science Research Division, Korea Institute of Oriental Medicine, Daejeon, 34054, Republic of Korea; 5Korean Convergence Medical Science, Korea Institute of Oriental Medicine School, University of Science & Technology, Daejeon, 34054, Republic of Korea
Correspondence: Chang Hyun Han, Clinical Medicine Division, Korea Institute of Oriental Medicine, 1672 Yuseong-daero, Yuseong-gu, Daejeon, 34054, Republic of Korea, Tel +82 42-868-9498, Email [email protected] In-Hyuk Ha, Jaseng Spine and Joint Research Institute, Jaseng Medical Foundation, 3F 538 Gangnam-daero, Gangnam-gu, Seoul, 06110, Republic of Korea, Tel +82 2-2222-2740, Email [email protected]
Purpose: Cervical myelopathy (CM) is generally considered an indication for surgery in Western medicine. Case reports have indicated that Korean medicine (KM) treatments are effective in improving CM-associated symptoms. We investigated the effectiveness of non-surgical KM treatment of CM patients through a retrospective chart review and follow-up survey.
Patients and Methods: We retrospectively analyzed the medical records and surveyed follow-up data of CM patients with neurological symptoms admitted to KM hospitals between January 2011 and January 2018. The admission and discharge assessments included the numeric rating scale (NRS) for neck and arm pain, neck disability index (NDI), and 5-level EuroQol 5-dimension (EQ-5D-5L). A follow-up survey was conducted about whether surgery was subsequently performed or recommended, symptom recurrence, discomfort in daily living, current treatment, as well as NRS, NDI, EQ-5D-5L, and patient global impression of change (PGIC) scores.
Results: The NRS for neck pain decreased from 4.88 ± 2.03 (95% CI: 4.23‒5.52) at admission to 3.23 ± 1.64 (95% CI: 2.70‒3.75) at discharge and 2.24 ± 1.84 (95% CI: 1.43‒3.05) at follow-up. The NRS for radiating arm pain decreased from 5.42 ± 1.55 (95% CI: 4.93‒5.92) to 3.77 ± 1.54 (95% CI: 3.28‒4.27) at discharge and 2.43 ± 1.60 (95% CI: 1.72‒3.13) at follow-up. The NDI decreased significantly from 36.24 ± 18.79 (95% CI: 30.24‒42.24) at admission to 30.89 ± 15.54 (95% CI: 25.93‒35.86) at discharge and 13.35 ± 11.95 (95% CI: 8.08‒18.63) at follow-up. The EQ-5D score improved significantly from 0.70 ± 0.21 (95% CI: 0.63‒0.77) to 0.78 ± 0.17 (95% CI: 0.73‒0.84) at discharge and 0.84 ± 0.08 (95% CI: 0.80‒0.88) at follow-up. At the follow-up, four patients experienced persistent pain and were undergoing treatment (19.1%), while 20 patients (95.8%) reported symptom improvement.
Conclusion: From a long-term perspective, integrative KM treatment may help to reduce pain and improve function, and improve quality of life of CM patients.
Keywords: cervical myelopathy, Korean medicine, acupuncture, musculoskeletal manipulations, pharmacopuncture, Shinbaro
Introduction
Cervical myelopathy (CM) is a commonly serious spinal cord dysfunction caused by compression of the nerves as a result of changes in the cervical area that occur due to enlarged yellow ligaments and osteophyte proliferation around the disc. The disease occurs secondary to a severely herniated intervertebral disc (HIVD) in the cervical spine, ossification of the posterior longitudinal ligament (OPLL), and cervical spondylosis. The most common early symptoms include cervical and upper extremity pain, weakness of the hand muscles, clumsiness, paresthesia, and ambulatory impairment caused by weakening of the lower extremity muscles. According to Clarke and Robinson1 and Epstein et al,2 CM can progress rapidly. However, in most cases, it progresses slowly with cyclical episodes of improvement and exacerbation of symptoms. In general, once the symptoms develop, CM rarely resolves spontaneously.
CM is diagnosed based on characteristic clinical symptoms, such as weakening of the upper extremities, myelopathic hand, deep tendon hyperreflexia, and radiologic tests, such as magnetic resonance imaging (MRI).3 Radiological tests are needed for the accurate diagnosis and prediction of prognosis in CM. Magnetic resonance imaging (MRI) is reported to be more useful than other tests for examining the pathology associated with CM and for assessing the related changes in the spinal cord.4 CM is treated either conservatively or surgically. Conservative treatment modalities include non-steroidal anti-inflammatory drugs, physiotherapy, and cervical braces. Nevertheless, evidence-based standards of care are lacking.5 Surgical treatment generally involves anterior cervical decompression or fusion at an early stage.6 However, a prospective study that compared the effects of surgical and conservative treatment in patients with CM reported that there were no significant differences in the objective parameters between the two treatment groups at the 2-year follow-up.7 Similarly, a randomized controlled trial (RCT) with a 10-year follow-up failed to identify any significant differences in patients who did not experience rapid symptom onset.8 In addition, other studies have found that some CM patients have mild symptoms.9 In recent years, several case reports showed that Korean medicine (KM) treatments, such as acupuncture, moxibustion, herbal therapy, and Chuna therapy are effective in improving the symptoms associated with CM.10–12 However, as mentioned in several literature reviews, the potential of KM treatment as a conservative treatment has only been examined in a few low-quality RCTs13–15 and many case reports.
Thus, this study aimed to investigate the effectiveness of integrative KM treatment, a nonsurgical treatment, in treating CM, by analyzing the electronic medical records (EMRs) of patients diagnosed with CM who underwent inpatient integrative KM treatment at a KM hospital. Data on the long-term therapeutic effects were collected by telephonic survey.
Patients and Methods
Patients
Patients who received inpatient care at five network KM hospitals between January 2011 and January 2018 were enrolled in the study. Patients whose chief complaints were neurological impairments, such as cervical and upper extremity pain, upper extremity weakening or paresthesia, or ambulatory impairment due to weakening of the lower extremities, with symptoms in line with MRI findings primarily as determined by a radiologist, and secondarily diagnosed as CM by a KM doctor, were considered.
Patients were included if a T2-weighted MRI scan of their C-spine showed spinal cord compression and injury (high-signal contrast), and if their chief complaints were deemed to be caused by CM, and if neurological symptoms were present.
We excluded patients whose chief complaints were not symptoms of CM, or where there were no neurological impairments of the upper or lower extremities, those whose neurological impairments of the upper and lower extremities were not caused by spinal or tissue-related factors, or those whose medical records at hospital admission were not complete. We also excluded patients who did not provide consent to participate.
Treatment
Acupuncture treatment was administered using mainly proximal acupuncture points and Ah-shi points. Shinbaro pharmacopuncture was injected at 4‒5 acupoints proximal to the dysfunctional site, at the physician’s discretion. Each acupuncture point was injected with a total of 0.5‒1 cc using disposable injection needles.
Herbal medicine was provided as a water-based decoction (120 mL) and dried powder (2 g) (Ostericum koreanum, Eucommia ulmoides, Acanthopanax sessiliflorus, Achyranthes japonica, Psoralea corylifolia, Saposhnikovia divaricata, Cibotium barometz, Lycium chinense, Boschniakia rossica, Cuscuta chinensis, Glycine max, Atractylodes japonica).
Chuna manipulation was administered to pelvic, lumbar, thoracic, and cervical vertebrae at the physician’s discretion. Chuna is a Korean spinal manipulation that incorporates spinal manipulation techniques for joint mobilization that involve high-velocity, low-amplitude thrusts to joints slightly beyond the passive range of motion (ROM), and gentle force to joints within the passive ROM.
Chart Review
The EMRs of the eligible patients were reviewed to analyze patient characteristics (eg, sex, age, occupation), treatment modality (acupuncture, pharmacopuncture, herbal medicine, Chuna), length of hospital stay, admission and discharge assessments of the numeric rating scale (NRS), Vernon‒Mior Neck Disability Index (NDI), 5-level EuroQol 5-dimension (EQ-5D-5L), and physical examinations. In addition, the types and frequency of integrative KM treatments performed during the hospital stay were examined.
Follow-Up Survey
A follow-up survey was conducted telephonically. The survey inquired whether cervical surgery was performed after discharge, whether cervical surgery was recommended prior to hospitalization, symptom recurrence, discomfort in daily living, the current status of persistent pain (≥ 3 months) that hinders daily living, current treatment for neck or upper extremity pain, as well as the NRS for neck pain and radiating arm pain, NDI, EQ-5D-5L, and patient global impression of change (PGIC) scores.
Outcomes
We used the outcomes described below to analyze improvement in aspects such as pain, function, and quality of life related to CM. These outcomes had been used in many previous neck pain and CM-related studies, and their reliability and validity have been acknowledged.16,17
Neck Pain and Radiating Arm Pain
The NRS was used to measure the patients’ subjective neck and arm pain.18 The patients chose a number from 0 (no pain) to 10 (unbearable pain) to indicate their level of pain.
NDI
The NDI was developed to examine the degree of cervical impairment in daily living. It comprises 10 questions that are rated on a 6-point scale (from 0 to 5). The total possible score is 50.19 The NDI was computed by dividing the total score by the number of items completed.
EQ-5D-5L
The EQ-5D-5L was developed to measure health-related quality of life and is widely used in the field of healthcare. It consists of five items (mobility, self-care, usual activities, pain/discomfort, anxiety/depression), with each item rated on five levels (level 1: no problems; level 2: slight problems; level 3: moderate problems; level 4: severe problems; level 5: extreme problems). In this study, weights estimated for the Korean population were used to determine the health-related quality of life.20
PGIC
The PGIC is a tool used to assess the level of improvement in patients (1: very much improved; 2: much improved; 3: minimally improved; 4: no change; 5: minimally worse; 6: much worse; or 7: very much worse). This index was originally developed for psychological assessments, but it is currently used in other medical fields to assess improvement in pain.21
Ethics Statement
This study was approved by the Institutional Review Board of the Jaseng Hospital of Korean Medicine (JASENG 2018-11-003-012). This study was conducted in accordance with the Declaration of Helsinki. The study was carried out in compliance with all the applicable research ethics. In addition, informed consent was obtained from the patients before the follow-up survey.
Statistical Analysis
In order to analyze the participants’ baseline characteristics and baseline outcomes, continuous variable data are presented as mean and standard deviation, while categorical variable data are presented as frequency and percentage. In relation to the details of treatment during the hospital stay, we computed the number and percentage of patients who received each treatment, and for patients who received different types of treatment, the number of treatment sessions is expressed as mean ± standard deviation (SD) and median (1st quartile–3rd quartile).
The outcomes at each time point are presented as mean ± SD, and changes from the baseline are presented as mean and 95% confidence interval (CI). Changes over time were tested using a linear mixed model. Time of measurement was considered a categorical variable and was included in the model as a fixed effect along with the baseline value of each outcome. The subjects were included as a random effect. The results are presented with a 95% CI.
For the long-term follow-up, continuous variable data are presented as mean ± SD and median (1st quartile–3rd quartile), and categorical variable data are presented as frequency and percentage.
Statistical significance was set at p < 0.05. Statistical analyses were performed using R Studio (Version 1.1.463-© 2009–2018 RStudio, Inc., Boston, MA, USA).
Results
Patient Flow
We screened 81 patients with suspected CM. Of these, patients whose imaging findings indicated CM, but who lacked neurological symptoms (n = 6), patients who were diagnosed with CM but who received inpatient care for a different chief complaint (n = 14), and patients whose admission and discharge data were not accurately recorded (n = 21) were excluded. Thus, 40 patients were included in the study. Of them, 19 patients who refused to participate in the telephonic survey and patients who could not be reached due to a change in phone number or address were excluded. Finally, the questionnaire data of 21 patients were used for the analysis. The overall flow chart is illustrated in Figure 1.
 |
Figure 1 Flow diagram of the patients included in the study. |
Baseline Characteristics
The mean age of the 40 patients was 51.8 ± 10.4 years, with 24 men (60%) and 16 women (40%). The mean onset time was 364.4 ± 748.2 days. CM onset had no specific cause in 31 patients (77.5%) and was caused by trauma in nine patients (22.5%). Ten patients (25%) took analgesics and another 10 patients (25%) received a steroid injection within a week prior to admission. The type of radiating pain was unilateral (n = 20, 50%) or bilateral (n = 20, 50%). There were 17 cases (42.5%) with ROM restrictions, 11 cases (27.5%) with muscle weakness, and 26 cases (65.0%) of paresthesia. The imaging tests revealed that the 40 (100%) patients had an HIVD in the cervical spine, three of whom had undergone surgery for the same. Seven patients (17.5%) had cervical stenosis, while one patient (2.5%) had OPLL (Table 1).
 |
Table 1 Baseline Characteristics of the Patients (n=40) |
Length of Hospital Stay and Details of Treatment
The mean length of the hospital stay was 21.9 ± 17.4 days. The type of treatment and proportion of each treatment were as follows: acupuncture (100%), pharmacopuncture (97.5%), herbal medicine (97.5%), Chuna (77.5%), herbal hot pack (42.5%), and traction (27.5%) (Table 2). There were no reports of treatment-related side effects.
 |
Table 2 Length of Hospital Stay and Details of Treatment (n=40) |
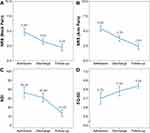
Changes in the Outcome After Treatment
The NRS for neck pain decreased from 4.88 ± 2.03 (95% CI: 4.23‒5.52) at admission to 3.23 ± 1.64 (95% CI: 2.70‒3.75) at discharge and 2.24 ± 1.84 (95% CI: 1.43‒3.05) at follow-up (p < 0.001), and the NRS for radiating arm pain decreased from 5.42 ± 1.55 (95% CI: 4.93‒5.92) at admission to 3.78 ± 1.54 (95% CI: 3.28‒4.27) at discharge and 2.43 ± 1.60 (95% CI: 1.72‒3.13) at follow-up (p < 0.001). The NDI decreased significantly from 36.24 ± 18.79 (95% CI: 30.24‒42.24) at admission to 30.89 ± 15.54 (95% CI: 25.93‒35.86) at discharge (p = 0.01) and 13.35 ± 11.95 (95% CI: 8.08‒18.63) at follow-up (p < 0.001). The EQ-5D score improved significantly from 0.70 ± 0.21 (95% CI: 0.63‒0.77) at admission to 0.78 ± 0.17 (95% CI: 0.73‒0.84) at discharge and 0.84 ± 0.08 (95% CI: 0.80‒0.88) at follow-up (p < 0.001) (Table 3, Figure 2).
Follow-Up Survey Results
The mean time between discharge and follow-up was 983.5 ± 423.4 days. Of the 21 patients included, 15 had been recommended to undergo surgery prior to being admitted to the KM hospital. Six (28.6%) patients underwent surgery after discharge from the KM hospital, while 15 (71.4%) did not. Four patients (19.1%) had a relapse of persistent pain that lasted more than 3 months, which was severe enough to hinder daily living, and these four patients (19.1%) were receiving treatment for pain at the time of writing. Two of these patients chose KM treatment, and the other two patients chose Western medical treatment (pharmacological and physical therapy). The PGIC results ascertained in the long-term follow-up were as follows: very much improved: n = 6, 28.6%; much improved: n = 8, 38.1%; minimally improved: n = 6, 28.6%; or no change: n = 1, 4.8% (Table 4).
 |
Table 3 Change in the Outcomes After Treatment (n=40) |
 |
Table 4 Follow-Up Survey Results of Cervical Myelopathy Patients (n=21) |
Discussion
The findings of this study highlight the potential of intensive inpatient KM care as a conservative treatment for mild-to-moderate CM, without leading to paralysis or rapid progression of neurological symptoms, to secure time to determine the need for surgery and to improve some symptoms. The results of this study objectively demonstrated that conservative treatment with KM is effective in improving symptoms associated with CM, thereby ensuring patient satisfaction over the long-term, and represents an advancement over the fragmentary information obtained by case series to date.
In general, CM is treated conservatively or surgically. Surgery is commonly performed in Western medicine to achieve symptomatic improvement through early decompression for severe CM.6 The typical surgeries performed are laminectomy and fusion, and laminoplasty. Both surgical techniques are beneficial for attaining rapid functional recovery and pain relief.22 Expansive laminoplasty is considered an excellent method that minimizes the risk of the common complications associated with laminectomy, such as cervical instability, osteocyte formation, and nerve injury. However, several studies have reported that expansive laminoplasty can also cause complications, such as kyphosis and cervical fracture.23
In relation to the treatment for CM, Ghogawala et al24 stated that conservative or surgical treatment should be chosen, depending on the severity of the symptoms. According to retrospective postoperative evaluations of CM, surgery should be considered for patients with moderate-to-severe CM with persistent spinal symptoms that hinder activities of daily living with a modified Japanese Orthopedic Association score of < 11, while surgery is not immediately necessary for patients with mild CM without such symptoms.25,26 In addition, Kadaňka et al8 reported that conservative treatment produces superior therapeutic effects for mild cases of CM, as compared to surgery.
Conservative treatments include neck immobilization, pharmacological treatments, lifestyle modifications, and physical modalities.27 In KM, herbal medicine, acupuncture, acupotomy, retraction, and Chuna therapies are used as conservative treatment for CM, and the most commonly used treatment modality is herbal therapy.28 Similar results were observed in our study, with the most frequently performed treatments being herbal therapy, acupuncture, pharmacopuncture, and Chuna therapy.
The treatment methods provided to patients with CM at this hospital vary. Among them, acupuncture, pharmacopuncture, herbal medicine, and Chuna therapy were the treatments most commonly applied to patients, on the following grounds: Acupuncture is reported to improve spinal cord injury by inhibiting the Notch signaling pathway and stimulating endogenous neural stem cell proliferation.29 A systematic review also confirmed that acupuncture is effective in treating spinal cord injuries.30 The most widely used herbal regimen was cheongpajeon (Ostericum koreanum, Eucommia ulmoides, Acanthopanax sessiliflorus, Achyranthes japonica, Psoralea corylifolia, Saposhnikovia divaricata, Cibotium barometz, Lycium chinense, Boschniakia rossica, Cuscuta chinensis, Glycine max, and Atractylodes japonica), and multiple studies have documented its effectiveness in reducing pain in patients with spinal joint diseases.31–33 The active ingredient of cheongpajeon, GCSB-5, has anti-inflammatory,34,35 neuroprotective, and neuroregenerative effects,36 thus reducing inflammation, promoting pain relief, and stimulating tissue regeneration in spinal joint diseases.
Pharmacopuncture is a treatment that integrates herbal medicine with acupuncture, where the mechanical and chemical effects of both acupuncture and herbal medicine are achieved by utilizing acupoint access. Pharmacopuncture enables the direct absorption of herbal extracts at the site of pain, as opposed to having to pass through the digestive tract. This ensures a rapid onset of action and allows patients who have difficulty taking oral medicine to reap the benefits of herbal medicine.37 Pharmacopuncture has been shown to be significantly effective in treating various musculoskeletal disorders,38 with proven safety.39 Persistent CM compresses the proximal nerve roots and may cause radiculopathy.40 If the muscles innervated by a cervical nerve at the lesion repeatedly undergo abnormal tension and relaxation, induration may develop at the site, exacerbating the symptoms of radiculopathy.41 As shown in a previous study, where the symptoms of radiculopathy caused by nerve compression from a cervical disc herniation were alleviated by Shinbaro pharmacopuncture,42 high-dose pharmacopuncture applied at the cervical Hyeopcheok point in this study probably contributed to alleviating pain and promoting functional recovery.
It is believed that the combined effects of the various treatments used in this study helped the recovery of nerve damage caused by CM, pain reduction, and functional recovery, but it is not possible to distinguish how much each effect contributed.
It is difficult to treat and follow-up patients with CM continuously at a hospital that primarily focuses on conservative treatment, because CM is generally accepted as an indication for surgery. However, we performed a retrospective analysis of multicenter inpatient data for CM and performed a long-term follow-up of the patients over the telephone. The mean time from discharge to follow-up was 983.5 ± 423.4 days. Our findings in relation to the long-term effects of the treatments is one of the notable aspects of this study. Furthermore, given that 20 of the 21 patients who participated in the follow-up survey stated that their symptoms had improved, the results are promising. Of these 21 patients, 15 patients were recommended to undergo surgery, but only six underwent the surgery, and only four patients were receiving treatment for persistent pain that lasted for more than 3 months, which is a relatively low number considering the severity of the disease and the likelihood of exacerbation. Compared with other studies, surgery for CM, such as laminectomy (which is the most common surgical treatment) reduced NRS of pain (−2.0), and in this study, non-surgical inpatient treatment resulted in a decrease in NRS (−1.65 at discharge; −2.92 at follow-up). Although there was no control group in our study design, compared to the previous study, KM treatment was considered to have an effect comparable to that of the existing surgical treatment.
This study had some limitations. Because CM is a not a common condition, with a prevalence of about 1.6 per 100,000 population,43 and as there are cases in which conservative treatment cannot be selected, because surgery is indicated for cases with rapid progression of the acute phase, oriental medicine is rarely chosen as treatment. For this reason, the sample size was small, and only half of these patients were enrolled in the long-term follow-up, for reasons such as changes in contact numbers. The small sample size posed limitations in terms of the statistical analysis. Another limitation of this study was that we could not pinpoint the specific treatment that primarily led to the improvement of symptoms, because an integrative treatment approach was applied. The possibility of spontaneous regression of the disease cannot be completely eliminated since the study design lacked a control group.
Nevertheless, while most studies on conservative treatment for CM have been case series reporting fragmentary findings, this study indicated that a large-scale study on the topic is warranted and it shed light on the possibility that intensive KM treatment can produce long-term therapeutic effects, even without surgery, in some mild cases of CM with no progression of neurological symptoms. Furthermore, the fact that intensive inpatient care with KM provides sufficient time for clinicians to observe the patients to ascertain whether there is progression or improvement in neurological symptoms and to identify patients who do not require surgery illustrates its potential as a conservative treatment for CM. Subsequently, studies on CM should utilize a prospective design with a large sample in the light of these findings.
Conclusion
This study provided evidence, from a long-term perspective, that integrative KM treatment can be considered to be helpful in reducing pain and improving function in CM patients, as well as in improving their quality of life.
Abbreviations
CI, confidence interval; CM, cervical myelopathy; EQ-5D-5I, 5-level EuroQol 5-dimension; HIVD, herniated intervertebral disc; KM, Korean medicine; MRI, magnetic resonance imaging; NDI, neck disability index; NRS, numeric rating scale; OPLL, ossification of the posterior longitudinal ligament; PGIC, patient global impression of change; RCT, randomized clinical trial.
Institutional Review Board Statement
The study protocol was approved by the Institutional Review Board of Jaseng Hospital of Korean Medicine (approval no.: JASENG 2018-11-003-012) and was registered at ClinicalTrials.gov (NCT04655833).
Data Sharing Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy/ethical restrictions.
Informed Consent Statement
Informed consent was obtained from the patients for research purposes before the follow-up survey.
Funding
This study was supported by grants from the project of the Korea Institute of Oriental Medicine (KSN2022210).
Disclosure
The authors declare no conflicts of interest for this work.
References
1. Clarke E, Robinson PK. Cervical myelopathy: a complication of cervical spondylosis. Brain. 1956;79(3):483–510. doi:10.1093/brain/79.3.483
2. Epstein J, Janin Y, Carras R, Lavine L. A comparative study of the treatment of cervical spondylotic myeloradiculopathy. Acta Neurochir. 1982;61(1–3):89–104. doi:10.1007/BF01740074
3. Chang H. Cervical spondylotic myelopathy. J Korean Soc Spine Surg. 1999;6(2):194–200.
4. Chang H, Won-Jong B, Jae-Goo A, Kyu-Ho C. Pre an postoperative evaluation of cervical myelopathy using MR imaging. J Korean Soc Spine Surg. 1994;1(2):326–336.
5. Rhee JM, Shamji MF, Erwin WM, et al. Nonoperative management of cervical myelopathy: a systematic review. Spine. 2013;38(22S):S55–S67. doi:10.1097/BRS.0b013e3182a7f41d
6. Tetreault L, Goldstein CL, Arnold P, et al. Degenerative cervical myelopathy: a spectrum of related disorders affecting the aging spine. Neurosurgery. 2015;77(suppl_1):S51–S67. doi:10.1227/NEU.0000000000000951
7. Kadaňka Z, Bednařík J, Voháňka S, et al. Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study. Eur Spine J. 2000;9(6):538–544. doi:10.1007/s005860000132
8. Kadaňka Z, Bednařík J, Novotný O, Urbánek I, Dušek L. Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. Eur Spine J. 2011;20(9):1533–1538. doi:10.1007/s00586-011-1811-9
9. Tracy JA, Bartleson J. Cervical spondylotic myelopathy. Neurologist. 2010;16(3):176–187. doi:10.1097/NRL.0b013e3181da3a29
10. Kim J, Cho J, Nam D, Kang JW, Lee S. Integrative Korean medicine as a possible conservative treatment for mild cervical spondylotic myelopathy: one-year follow-up case report (CARE-compliant). Medicine. 2018;97(36):e12249.
11. Lee T-G, Kim K-H, Kim T-Y, et al. Clinical study on 2 cases of cervical spondylotic myelopathy treated by Korean traditional medicine. J Korean Med Rehabil. 2019;29(3):141–148. doi:10.18325/jkmr.2019.29.3.141
12. Lee M-J, Kim K-W, Nam J-H, et al. Clinical observation of the change with radiological view on cervical myelopathy patient treated by Korean medical treatments. J Acupunct Res. 2012;29(1):159–167.
13. Zhang P, Wu X, Hu Z, Zhou C. Clinical observation on the treatment of cervical spondylotic myelopathy with needle-knife therapy. Hubei J Tradit Chin Med. 2014;36(9):62–63.
14. Chai S, Zhou B. Clinical observation of scalp acupuncture combined with abdominal acupuncture for cervical spondylotic myelopathy in early stage. J New Chin Med. 2018;50(4):166–168.
15. Li J, Zhao B, Bai G, et al. Clinical study of comprehensive treatment by traditional Chinese medicine for cervical spondylotic myelopathy. China Med Herald. 2014;11(32):77–82.
16. Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14(7):409–415.
17. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), McGill pain questionnaire (mpq), short‐form McGill pain questionnaire (sf‐mpq), chronic pain grade scale (CPGs), short form‐36 bodily pain scale (sf‐36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res. 2011;63(S11):S240–S252.
18. Solodiuk JC, Scott-Sutherland J, Meyers M, et al. Validation of the Individualized Numeric Rating Scale (INRS): a pain assessment tool for nonverbal children with intellectual disability. Pain. 2010;150(2):231–236. doi:10.1016/j.pain.2010.03.016
19. Vernon H. The Neck Disability Index: state-of-the-art, 1991–2008. J Manipulative Physiol Ther. 2008;31(7):491–502. doi:10.1016/j.jmpt.2008.08.006
20. Kim S-H, Ahn J, Ock M, et al. The EQ-5D-5L valuation study in Korea. Qual Life Res. 2016;25(7):1845–1852. doi:10.1007/s11136-015-1205-2
21. Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1):9–19. doi:10.1016/j.pain.2004.09.012
22. Manzano GR, Casella G, Wang MY, Vanni S, Levi AD. A prospective, randomized trial comparing expansile cervical laminoplasty and cervical laminectomy and fusion for multilevel cervical myelopathy. Neurosurgery. 2012;70(2):264–277. doi:10.1227/NEU.0b013e3182305669
23. Suk K-S, Kim K-T, Lee J-H, Lee S-H, Kim J-S, Uh J-H. The surgical treatment of the cervical myelopathy with laminectomy and posterior fusion by using lateral mass screw fixation. J Korean Orthop Assoc. 2009;44(1):123–129. doi:10.4055/jkoa.2009.44.1.123
24. Ghogawala Z, Benzel EC, Riew KD, Bisson EF, Heary RF. Surgery vs conservative care for cervical spondylotic myelopathy: surgery is appropriate for progressive myelopathy. Neurosurgery. 2015;62(CN_suppl_1):56–61. doi:10.1227/NEU.0000000000000781
25. Fujiwara K, Yonenobu K, Ebara S, Yamashita K, Ono K. The prognosis of surgery for cervical compression myelopathy. An analysis of the factors involved. J Bone Joint Surg Br. 1989;71(3):393–398. doi:10.1302/0301-620X.71B3.2722928
26. Fukushima T, Ikata T, Taoka Y, Takata S. Magnetic resonance imaging study on spinal cord plasticity in patients with cervical compression myelopathy. Spine. 1991;16(10 Suppl):S534–S538. doi:10.1097/00007632-199110001-00016
27. Bakhsheshian J, Mehta VA, Liu JC. Current diagnosis and management of cervical spondylotic myelopathy. Global Spine J. 2017;7(6):572–586. doi:10.1177/2192568217699208
28. Byun D-Y, Lee G-E, Roh J-A, Kim H-J, Huh S-W, Han S-H. A review of the Korean traditional medicine for cervical spondylotic myelopathy. J Korean Med Rehabil. 2019;29(2):149–158. doi:10.18325/jkmr.2019.29.2.149
29. Geng X, Sun T, Li J-H, Zhao N, Wang Y, Yu H-L. Electroacupuncture in the repair of spinal cord injury: inhibiting the Notch signaling pathway and promoting neural stem cell proliferation. Neural Regen Res. 2015;10(3):394. doi:10.4103/1673-5374.153687
30. Heo I, Shin B-C, Kim Y-D, Hwang E-H, Han CW, Heo K-H. Acupuncture for spinal cord injury and its complications: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2013;2013:1–18. doi:10.1155/2013/364216
31. Park JJ, Shin J, Choi Y, et al. Integrative package for low back pain with leg pain in Korea: a prospective cohort study. Complement Ther Med. 2010;18(2):78–86. doi:10.1016/j.ctim.2010.02.003
32. Kim S-Y, Min K-S, Kim T-H, Jeong H-C, Jun B-C, Lee J-H. A case report of conservative treatment of the lumbar incomplete burst fracture. J Korea CHUNA Manual Med Spine Nerves. 2010;5(2):85–94.
33. Kim Y, Shin J-S, Kim D-W. The clinical effect of Cheongpa-jeon on the group of patients who were treated under conservative remedies for LBP (Low Back Pain). J Korea Chuna Manual Med. 2004;5(1):85–92.
34. Chung H-J, Lee H-S, Shin J-S, et al. Modulation of acute and chronic inflammatory processes by a traditional medicine preparation GCSB-5 both in vitro and in vivo animal models. J Ethnopharmacol. 2010;130(3):450–459. doi:10.1016/j.jep.2010.05.020
35. Kim S-H, Lee C-H, Lee J-S, et al. Anti-inflammatory activities of a herbal preparation GCSB-5 on acute and chronic inflammation. Korean J Pharmacogn. 2005;36(4):311–317.
36. Kim T-H, Yoon S-J, Lee W-C, et al. Protective effect of GCSB-5, an herbal preparation, against peripheral nerve injury in rats. J Ethnopharmacol. 2011;136(2):297–304. doi:10.1016/j.jep.2011.04.037
37. Luna SP, Angeli AL, Ferreira CL, Lettry V, Scognamillo-Szabo M. Comparison of pharmacopuncture, aquapuncture and acepromazine for sedation of horses. Evid Based Complement Alternat Med. 2008;5(3):267–272. doi:10.1093/ecam/nel096
38. Lee YJ, Shin J-S, Lee J, et al. Usage report of pharmacopuncture in musculoskeletal patients visiting Korean medicine hospitals and clinics in Korea. BMC Complement Altern Med. 2016;16(1):292. doi:10.1186/s12906-016-1288-5
39. Lee J-H, Chung H-J, Lee I-H, Lee J-W, Kim E-J, Kim M-J. Study on single-dose intramuscular toxicity of Shinbaro pharmacopuncture in Sprague-Dawley (SD) rats and beagle dogs. J Korean Med Rehabil. 2015;25(3):1–9.
40. Lindsay KW, Bone I, Fuller G. Neurology and neurosurgery Illustrated e-Book. Elsevier Health Sciences; 2010.
41. Lane K, Berkow R. The Merck Manual: a century of medical publishing and practice. CBE VIEWS. 1999;22:112–113.
42. Choi JH, Lee SH, Kim SM, et al. Effects of Korean medical combination treatment for 102 cases of cervical disc herniation: an observational study. Acupuncture. 2016;33(2):11–20. doi:10.13045/acupunct.2016013
43. Boogaarts HD, Bartels RH. Prevalence of cervical spondylotic myelopathy. Eur Spine J. 2015;24(2):139–141. doi:10.1007/s00586-013-2781-x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.