Back to Journals » Clinical Ophthalmology » Volume 15
Long-Term Follow-Up of Combined Photorefractive Keratectomy and Corneal Crosslinking in Keratoconus Suspects
Authors Kymionis G, Kontadakis G , Grentzelos M, Petrelli M
Received 30 November 2020
Accepted for publication 6 April 2021
Published 9 June 2021 Volume 2021:15 Pages 2403—2410
DOI https://doi.org/10.2147/OPTH.S294775
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
George Kymionis,1 George Kontadakis,1,2 Michael Grentzelos,1 Myrsini Petrelli1
1Department of Ophthalmology, University of Lausanne, Jules-Gonin Eye Hospital, Fondation Asile des Aveugles, Lausanne, Switzerland; 2Laboratory of Vision and Optics, University of Crete, Heraklion, Greece
Correspondence: George Kontadakis
Laboratory of Vision and Optics, University of Crete, Heraklion, Greece
Email [email protected]
Purpose: To present the long-term outcomes of photorefractive keratectomy (PRK) combined with accelerated corneal cross-linking (CXL) for refractive error correction in a series of keratoconus suspects.
Setting: University practice.
Design: Retrospective case series.
Methods: A series of patients with topographic findings suspicious for keratoconus underwent simultaneous PRK and prophylactic accelerated CXL (5 minutes with intensity of 18 mW/cm2) for the correction of their refractive error. The results were recorded for more than 4 years postoperatively.
Results: Ten eyes of 5 patients were included. Mean follow-up was 58.2 months (range from 54 to 62 months). Mean age at presentation was 25 years (range from 22 to 32 years). Mean spherical equivalent (SE) refraction was − 2.76 (standard deviation [SD] 0.97D, range from − 1.25 to − 4.00 diopters [D]), while mean central corneal thickness was 511μm (SD 13μm, range from 485 to 536 μm). At last, follow-up 9 out of 10 eyes had SE refraction within ± 0.50D and all eyes had SE within ± 1.00D. None of the eyes lost any line of corrected distance visual acuity (CDVA), whereas 1 eye gained one line of CDVA. All eyes demonstrated stability of their results during the follow-up period.
Conclusion: Simultaneous PRK followed by prophylactic accelerated CXL (PRK plus) appeared to be a safe and effective option for the correction of the refractive error in this series of keratoconus suspect patients, without compromising corneal stability for up to 5 years postoperatively.
Keywords: corneal crosslinking, photorefractive keratoplasty, forme fruste keratoconus, corneal topography, irregular astigmatism
Introduction
Photorefractive keratectomy (PRK) is a well-established surface ablation technique for the correction of myopia and astigmatism.1 In certain cases, such as in patients with inadequate corneal thickness and/or abnormal corneal topography, PRK may be preferable to LASIK in order to decrease the possibility of postoperative corneal ectasia. Cases of corneal ectasia after LASIK in one eye and a stable result following PRK in the fellow eye indicate that PRK may pose a lower risk for the development of corneal ectasia.2,3 Nevertheless, corneal ectasia after PRK has been reported4,5 in literature. Although some studies have reported stable results after PRK in eyes with abnormal topography, the majority of refractive surgeons would avoid to perform even PRK to a patient with increased risk for ectasia.6,7
Corneal cross-linking (CXL) represents a minimally invasive surgical procedure used to strengthen the ectatic cornea thus resulting in corneal stabilization.8,9 Accelerated CXL protocols have been developed as an alternative to conventional CXL and have been shown to be effective in halting keratoconus progression.10,11 Combined PRK and CXL is an alternative surgical technique for the management of keratoconic patients resulting not only in corneal stabilization but also in visual improvement.12–17 Combining PRK with CXL, could therefore be an alternative option for refractive error correction in patients with topographic findings suspicious of keratoconus in an attempt to decrease the possibility of postoperative corneal ectasia.
Herein, we evaluate the long-term visual, refractive and topographic outcomes after simultaneous photorefractive keratectomy (PRK) and accelerated CXL in keratoconus suspects.
Methods
In this retrospective case series, we included patients with suspicious topographic findings that had undergone combined PRK and CXL for the correction of their refractive error and have been followed for at least four years after the procedure. All cases included in our study were classified as being at moderate risk for developing postoperative ectasia (cumulative risk scale score 3) according to the Ectasia Risk Score System.18,19 After appropriately informed about the surgical technique, the possibilities of favourable outcome and the possible complications, the patients provided written informed consent according to the institutional guidelines and the Declaration of Helsinki. The study has been approved by the research ethics committee of the Medical School of the University of Crete.
Surgical Technique and Evaluation
All procedures were performed at the Vardinoyiannion Eye Institute of Crete by the same surgeon (G.D.K.) under sterile conditions. After administration of topical anesthesia with proxymetacaine hydrochloride 0.5% eye drops (Alcaine; Alcon Laboratories Inc, Ft Worth, TX), corneal epithelium was removed mechanically using a rotating brush at an intended zone of 8.0 mm. Conventional PRK (6.5 mm optical zone) was performed using the Allegretto Wavelight excimer laser (Wavelight Technologies, Erlangen, Germany) with postoperative target emmetropia. Following this, 0.1% riboflavin (0.1% solution of 10 mg riboflavin-5-phosphate in 10mL dextran-T-500 20% solution, Medicross, Medio-Haus Behrensbrook, Neudorf, Germany) was instilled every 3 minutes for approximately 15 minutes. Ultraviolet-A (UVA) irradiation was performed using a UVA optical system (CCL-365, Peschke Meditrade GmbH, Huenenberg, Switzerland). Before treatment, an irradiation intensity of 18.0 mW/cm2 was calibrated using the UVA light meter YK-35UV (Lutron Electronic, Coopersburg, PA), which is supplied with the UV-X device. Irradiation was performed for 5 minutes, corresponding to a total fluence of 5.4 J/cm2. During UVA irradiation, riboflavin solution was applied once at 2.5 minutes to maintain corneal saturation with riboflavin. At the end of the procedure, a silicone-hydrogel (Lotrafilcon B, Air Optix, Ciba Vision, Duluth, GA) bandage contact lens (BCL) was applied until total re-epithelialization.
Postoperative medication included ofloxacin (Exocin, Allergan Pharmaceuticals Ltd, Westport, Ireland) and chloramphenicol/dexamethasone drops (Dispersadron, Thea Laboratories, Inc, Clermont-Ferrand, France), both four times daily until re-epithelialization was complete. After the removal of the BCL, patients received steroid drops (fluorometholone 0.1%, FML; Falcon Pharmaceuticals, Fort Worth, TX) that were tapered gradually over the next 3 months. Patients were encouraged to use artificial tears at least six times per day for 3 months postoperatively.
Patients were followed daily until complete reepithelialisation, when the CL was removed. Following this we have been evaluating the patients at postoperative day 15, months 1, 3, 6, 9, 12 and then annually. In each of the postoperative visits after the epithelialization the VA and refraction were measured, and corneal topography was performed in all visits starting from the 1st postoperative month. We evaluated the demarcation line depth in the 1st month visit with anterior segment optical coherence tomography (Visante OCT, Carl Zeiss, Germany). For the purpose of this study we described the rate of epithelialization and the occurrence of complications, the refractive stability, the safety and the accuracy of the procedure in all eyes. Additionally, we included the demarcation line and we assessed topographic stability by means of comparative topography maps in order to assess any progression based on previously described criteria for topographic progression of keratoconus.14
Results
Ten eyes of 5 patients were included in this case series. All eyes were keratoconus suspects with asymmetric steepening and/or skewed axis in corneal topography. Mean follow-up of the patients was 58.2 months (range from 54 to 62). Mean age of the patients at presentation was 25 years (range from 22 to 32 years). Mean spherical equivalent refraction of all eyes preoperatively was −2.76 (standard deviation [SD] 0.97D, range from −1.25 to −4.00 D), while mean central corneal thickness was 511μm (SD 13 μm, range from 485 to 536 μm). Preoperative corrected distance visual acuity (CDVA) was 20/20 in 9 eyes and 20/25 in one eye.
All operations were uneventful. Re-epithelialization occurred in all eyes within 4 days after the operation. Any reported symptoms, including mild pain and discomfort, were similar to those observed following conventional PRK. Three out of 10 eyes developed haze grade 1 (on the Fantes corneal stromal haze scale20) which gradually resolved until the sixth postoperative month. All eyes had SE within ± 1.00 D as early as two weeks postoperatively.
At last follow-up 9 out of 10 eyes had SE refraction within ± 0.50 D and all eyes had SE within ± 1.00 D (Figures 1 and 2). All eyes had uncorrected distance visual acuity (UDVA) of 20/25 or more and 9 eyes had UDVA of 20/20 or more. None of the eyes lost any line of CDVA, whereas 1 eye gained one line of CDVA (Figure 3). All eyes demonstrated refractive stability after the six-month follow-up visit, as no fluctuations in SE refraction greater than 0.50 D were observed (Figure 4). Corneal topography also remained stable in all cases after the sixth postoperative month and up to the last follow-up (Figure 5). Mean depth of the CXL demarcation line at the central cornea was 163.7 μm (SD 14.94μm, range from 145 to 186 μm) at the first postoperative month (Figure 6).
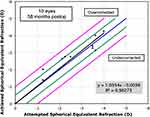 |
Figure 1 Chart of predictability, demonstrating the achieved spherical equivalent refraction as a function of attempted spherical equivalent refraction. |
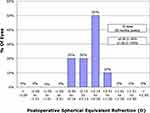 |
Figure 2 Graph of spherical equivalent (SE) accuracy. At last follow-up, nine out of ten eyes had SE within ± 0.50 D and all eyes were within ± 1.00 D. |
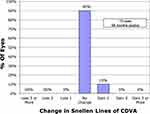 |
Figure 3 Graph of change in corrected distance visual acuity, demonstrating the gain of lines in 1 eye and stability in the rest of the eyes. |
Discussion
In this study, we present a novel technique for the correction of myopia in patients with corneas with suspicious topography findings and therefore at moderate risk of developing ectasia post refractive surgery. The risk of ectasia after LASIK has been correlated with certain preoperative parameters including asymmetric astigmatism, inferior steepening, skewed axis, low pachymetry and young age. In 90% of the post-LASIK ectasia cases, signs will have developed up to 4 years postoperatively.19 New, recently described parameters, based on corneal tomography and biomechanics have increased sensitivity and specificity in assessing high-risk corneas.21
It has been suggested that patients at moderate to high risk of developing ectasia after LASIK is preferable to be treated with surface ablation.19 Several studies have reported good refractive outcomes and corneal stability after PRK in eyes with abnormal topographic findings.6,7,22 Cases of post-LASIK corneal ectasia in one eye and a stable post-PRK result in the fellow eye suggest that the likelihood of ectasia may be lower after PRK.2,3 Nevertheless, post-PRK ectasia has previously been described in literature. Therefore, it is widely accepted that for patients at risk of developing ectasia, laser refractive surgery should be opted out or PKR should be implemented in carefully selected cases.4,5
Standard as well as accelerated CXL have shown to be effective in stabilizing the cornea and halting the progression of the ectatic disorder, in patients with either keratoconus or iatrogenic ectasia.8–11,23 Combined CXL with surface ablation has been used over several years for the treatment of patients with keratoconus in order not only to stabilize their corneal ectatic disorder but also to improve their functional vision.12–17 This combined technique has also been demonstrated as safe and effective regarding the stabilization in corneas with post-LASIK ectasia.24 Surface ablation in these studies has been applied in the form of topography guided PRK or conventional PRK for the correction of refractive error.12–17
Given these encouraging results of CXL in ectatic corneas, the prophylactic use of CXL has been introduced in patients that undergo refractive surgery and have high risk characteristics for developing ectasia. To date, CXL has been combined mainly with LASIK (LASIK-xtra), PRK and SMILE showing encouraging results.25–27 However, the risk of ectasia has not been eliminated as demonstrated by a report of ectasia after LASIK-xtra.28
In our series of patients, we combined PRK with accelerated prophylactic CXL. All patients were followed for more than 4 years postoperatively (average 5 years) in order to report on long-term results. The refractive outcomes of our patients remained relatively stable throughout the study period. Regarding safety, it is of great importance that none of the patients lost any line of CDVA.
However, the combination of CXL with PRK presents the same risks as CXL, including corneal haze and flattening. Corneal flattening may lead to a progressive hyperopic shift and that in turn can decrease the refractive accuracy of the combined technique. In our study, we used an accelerated protocol of CXL with intensity of 18 mW/cm2 for a 5-minute treatment time. Most studies in the current literature have demonstrated that accelerated CXL does not show progressive flattening in the extend of the Dresden protocol.11 Accordingly, in our patients, we did not observe any significant progressive flattening during our long-term follow-up.
The risk of haze formation following PRK is usually minimized with the use of mitomycin-C (MMC).1 In this series of patients MMC was not applied since we considered that the cytotoxic effect of CXL on keratocytes would be sufficient to prevent haze formation.29 Previous experience from combining PRK with standard CXL on keratoconus corneas has shown absence of anterior stromal haze due to PRK, but in some cases, development of posterior stromal haze was observed, that gradually decreases its density and was attributed to the combination of techniques.30 Nevertheless, our cases did not demonstrate significant haze formation.
Up to now, only few reports of PRK combined with CXL for correction of myopia have been published in the literature with promising results. Follow-up in these studies was up to 2 years and the authors had used different protocols. Lee et al27 treated patients with intensity 30 mW/cm2 and total fluence of 2.7J/cm2. Sachdev et al31 used the same protocol, but with no reported application of MMC. In the aforementioned studies patients were followed for one year and no significant complications were reported. Ohana et al32 used UV intensity of 9 mW/cm2 for 3min (5.4J/cm2) and described stable refractive outcomes for two years. In our pilot study, we implemented UV intensity of 18 mW/cm2 for 5 minutes thus achieving total fluence of 5.4J/cm2. During the 5-year follow-up period all of the eyes demonstrated stability in terms of refraction and keratometry.
Our study, albeit having the advantage of the long-term follow-up, has some significant limitations. At first, this study has a retrospective design and includes a relatively small number of patients. A larger number of participants would be preferable to add a sensitivity analyses and more firmly support the results. In addition, there was no control group consisting of patients treated only with PRK. Both eyes of each patient instead of one randomly selected were included in the study, thus conferring a possible cluster effect. Lastly, a contralateral eye study with patients operated with PRK in one eye and PRK-plus in the fellow eye would provide even stronger evidence for the efficacy of the procedure.
In conclusion, to our knowledge this is the first report of patients with suspected keratoconus findings treated with PRK followed by accelerated CXL with irradiation intensity of 18 mW/cm2 for 5 minutes, followed for more than 4 years postoperatively. Our study demonstrates that the described procedure might represent a safe and effective option, with good long-term outcomes, for refractive error correction in keratoconus suspects. A large cohort of patients is required in order to confirm our results and demonstrate efficacy in lowering the ectasia risk.
Abbreviations
CXL, corneal crosslinking; PRK, photorefractive keratectomy; UDVA, uncorrected distance visual acuity; UVA, ultraviolet-A; SE, spherical equivalent; CDVA, corrected distance visual acuity; SD, standard deviation; MMC, mitomycin-C.
Summary: Value Statement
Corneal crosslinking (CXL) combined with photorefractive keratectomy may offer refractive improvement and stabilization of corneas with progressive keratoconus. Such patients and also patients with topographic findings suspicious for keratoconus without progression cannot undergo refractive surgery without increased risk of progression to more advanced stages of ectasia. In this long-term case series, we sought to investigate the refractive results and the long-term effect of combined CXL with PRK in patients that feature findings suspicious of keratoconus. We included patients that are considered as keratoconus suspects with low to moderate myopia and astigmatism who underwent refractive correction with PRK followed by accelerated CXL and followed them for up to 5 years postoperatively. Our follow-up demonstrated that his technique offered predictable results that remained stable for up to 5 years. The combined technique might offer an alternative for safe refractive correction in such patients. More extensive prospective comparative studies are needed to confirm our results.
Disclosure
The authors have no financial or proprietary interest in any materials or methods described herein.
References
1. Diakonis VF, Kankariya VP, Kymionis GD, et al. Long term follow up of photorefractive keratectomy with adjuvant use of mitomycin C. J Ophthalmol. 2014;2014:821920. doi:10.1155/2014/821920
2. Rao SK, Srinivasan B, Sitalakshmi G, Padmanabhan P. Photorefractive keratectomy versus laser in situ keratomileusis to prevent keratectasia after corneal ablation. J Cataract Refract Surg. 2004;30:2623–2628. doi:10.1016/j.jcrs.2004.09.037
3. Kymionis GD, Tsiklis N, Karp CL, et al. Unilateral corneal ectasia after laser in situ keratomileusis in a patient with uncomplicated photorefractive keratectomy in the fellow eye. J Cataract Refract Surg. 2007;33:859–861.
4. Randleman JB, Caster AI, Banning CS, Stulting RD. Corneal ectasia after photorefractive keratectomy. J Cataract Refract Surg. 2006;32:1395–1398. doi:10.1016/j.jcrs.2006.02.078
5. Malecaze F, Coullet J, Calvas P, et al. Corneal ectasia after photorefractive keratectomy for low myopia. Ophthalmology. 2006;113:742–746. doi:10.1016/j.ophtha.2005.11.023
6. Sun R, Gimbel HV, Kaye GB. Photorefractive keratectomy in keratoconus suspects. J Cataract Refract Surg. 1999;25:1461–1466. doi:10.1016/S0886-3350(99)00234-5
7. Guedj M, Saad A, Audureau E, Gatinel D. Photorefractive keratectomy in patients with suspected keratoconus: five-year follow-up. J Cataract Refract Surg. 2013;39:66–73. doi:10.1016/j.jcrs.2012.08.058
8. Kymionis GD, Grentzelos MA, Liakopoulos DA, et al. Long-term follow-up of corneal collagen cross-linking for keratoconus—The Cretan Study. Cornea. 2014;33:1071–1079. doi:10.1097/ICO.0000000000000248
9. Kymionis GD, Grentzelos MA, Kankariya VP, et al. Long-term results of combined transepithelial phototherapeutic keratectomy and corneal collagen crosslinking for keratoconus: Cretan protocol. J Cataract Refract Surg. 2014;40:1439–1445. doi:10.1016/j.jcrs.2014.01.040
10. Toker E, Çerman E, Özcan DÖ, Seferoğlu ÖB. Efficacy of different accelerated corneal crosslinking protocols for progressive keratoconus. J Cataract Refract Surg. 2017;43:1089–1099. doi:10.1016/j.jcrs.2017.05.036
11. Kymionis GD, Kontadakis GA, Hashemi KK. Accelerated versus conventional corneal crosslinking for refractive instability: an update. Curr Opin Ophthalmol. 2017;28. doi:10.1097/ICU.0000000000000375
12. Kanellopoulos AJ, Asimellis G. Keratoconus management: long-term stability of topography-guided normalization combined with high-fluence CXL stabilization (The Athens protocol). J Refract Surg. 2014;30:88–93. doi:10.3928/1081597X-20140120-03
13. Grentzelos MA, Kounis GA, Diakonis VF, et al. Combined transepithelial phototherapeutic keratectomy and conventional photorefractive keratectomy followed simultaneously by corneal crosslinking for keratoconus: Cretan protocol plus. J Cataract Refract Surg. 2017;43:1257–1262. doi:10.1016/j.jcrs.2017.06.047
14. Kontadakis GA, Kankariya VP, Tsoulnaras K, et al. Long-term comparison of simultaneous topography-guided photorefractive keratectomy followed by corneal cross-linking versus corneal cross-linking alone. Ophthalmology. 2016;123(5):974–983. doi:10.1016/j.ophtha.2016.01.010
15. Kymionis GD, Kontadakis GA, Kounis GA, et al. Simultaneous topography-guided PRK followed by corneal collagen cross-linking for keratoconus. J Refract Surg. 2009;25.
16. Kanellopoulos AJ. Ten-year outcomes of progressive keratoconus management with the Athens protocol (Topography-guided partial-refraction PRK combined with CXL). J Refract Surg. 2019;35(8):478–483. doi:10.3928/1081597X-20190627-01
17. Al-Mohaimeed MM. Combined corneal CXL and photorefractive keratectomy for treatment of keratoconus: a review. Int J Ophthalmol. 2019;12:1929–1938. doi:10.18240/ijo.2019.12.16
18. Randleman JB, Trattler WB, Stulting RD. Validation of the ectasia risk score system for preoperative laser in situ keratomileusis screening. Am J Ophthalmol. 2008;145:813–818.e2. doi:10.1016/j.ajo.2007.12.033
19. Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008;115:37–50. doi:10.1016/j.ophtha.2007.03.073
20. Fantes FE, Hanna KD, Waring GO, et al. Wound healing after excimer laser keratomileusis (Photorefractive keratectomy) in monkeys. Arch Ophthalmol. 1990;108. doi:10.1001/archopht.1990.01070070051034
21. Ambrósio R, Lopes BT, Faria-Correia F, et al. Integration of scheimpflug-based corneal tomography and biomechanical assessments for enhancing ectasia detection. J Refract Surg. 2017;33:434–443. doi:10.3928/1081597X-20170426-02
22. Kymionis GD, Kankariya VP, Grentzelos MA, et al. Outcomes of refractive surgery in patients with topographic superior corneal steepening. J Refract Surg. 2012;28:462–467.
23. Vinciguerra P, Camesasca FI, Albe E, Trazza S. Corneal collagen cross-linking for ectasia after excimer laser refractive surgery: 1-year results. J Refract Surg. 2010;26:486–497. doi:10.3928/1081597X-20090910-02
24. Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the Athens protocol. J Refract Surg. 2011;27:323–331.
25. Konstantopoulos A, Liu Y-C, Teo EP, et al. Corneal stability of LASIK and SMILE when combined with collagen cross-linking. Transl Vis Sci Technol. 2019;8(3):21. doi:10.1167/tvst.8.3.21
26. Kanellopoulos AJ, Asimellis G, Salvador-Culla B, et al. High-irradiance CXL combined with myopic LASIK: flap and residual stroma biomechanical properties studied ex-vivo. Br J Ophthalmol. 2015;99(6):870–874. doi:10.1136/bjophthalmol-2014-306411
27. Lee H, Yong Kang DS, Ha BJ, et al. Comparison of outcomes between combined transepithelial photorefractive keratectomy with and without accelerated corneal collagen cross-linking: a 1-Year Study. Cornea. 2017;36:1213–1220. doi:10.1097/ICO.0000000000001308
28. Taneri S, Kiessler S, Rost A, Dick HB. Corneal ectasia after LASIK combined with prophylactic corneal cross-linking. J Refract Surg. 2017;33:50–52. doi:10.3928/1081597X-20161019-03
29. Kymionis GD, Diakonis VF, Kalyvianaki M, et al. One-year follow-up of corneal confocal microscopy after corneal cross-linking in patients with post laser in situ keratosmileusis ectasia and keratoconus. Am J Ophthalmol. 2009;147. doi:10.1016/j.ajo.2008.11.017
30. Kymionis GD, Portaliou DM, Diakonis VF, et al. Posterior linear stromal haze formation after simultaneous photorefractive keratectomy followed by corneal collagen cross-linking. Investig Ophthalmol Vis Sci. 2010;51:5030–5033.
31. Sachdev GS, Ramamurthy S, Dandapani R. Comparative analysis of safety and efficacy of photorefractive keratectomy versus photorefractive keratectomy combined with crosslinking. Clin Ophthalmol. 2018;12:783–790. doi:10.2147/OPTH.S156500
32. Ohana O, Kaiserman I, Domniz Y, et al. Outcomes of simultaneous photorefractive keratectomy and collagen crosslinking. Can J Ophthalmol. 2018;53:523–528. doi:10.1016/j.jcjo.2017.12.003
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



