Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Long-term cost and utility consequences of short-term clinically important deterioration in patients with chronic obstructive pulmonary disease: results from the TORCH study
Authors Paly VF , Naya I, Gunsoy NB, Driessen MT, Risebrough N, Briggs A , Ismaila AS
Received 27 September 2018
Accepted for publication 22 February 2019
Published 3 May 2019 Volume 2019:14 Pages 939—951
DOI https://doi.org/10.2147/COPD.S188898
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Victoria Federico Paly,1 Ian Naya,2 Necdet B Gunsoy,3 Maurice T Driessen,4 Nancy Risebrough,5 Andrew Briggs,6 Afisi S Ismaila7,8
1ICON Health Economics, ICON, Philadelphia, PA, USA; 2Global Respiratory Franchise, GSK, Brentford, Middlesex, UK; 3Value Evidence and Outcomes, GSK, Uxbridge, Middlesex, UK; 4Value Evidence & Outcomes, GSK, Brentford, Middlesex, UK; 5ICON Health Economics, ICON, Toronto, ON, Canada; 6Health Economics and Health Technology Assessment, Institute of Health and Wellbeing, University of Glasgow, Glasgow, UK; 7Value Evidence & Outcomes, GSK, Collegeville, PA, USA; 8Department of Health Research Methods, Evidence and Impact, McMaster University, Hamilton, ON, Canada
Purpose: Clinically important deterioration (CID) in chronic obstructive pulmonary disease (COPD) is a novel composite endpoint that assesses disease stability. The association between short-term CID and future economic and quality of life (QoL) outcomes has not been previously assessed. This analysis considers 3-year data from the TOwards a Revolution in COPD Health (TORCH) study, to examine this question.
Patients and methods: This post hoc analysis of TORCH (NCT00268216) compared costs and utilities at 3 years among patients without CID (CID-) and with CID (CID+) at 24 weeks. A positive CID status was defined as either: a deterioration in forced expiratory volume in 1 second (FEV1) of ≥100 mL from baseline; or a ≥4-unit increase from baseline in St George’s Respiratory Questionnaire (SGRQ) total score; or the incidence of a moderate/severe exacerbation. Patients from all treatment arms were included. Utility change was based on the EQ-5D utility index. Costs were based on healthcare resource utilization from 24 weeks to end of follow-up combined with unit costs for the UK (2016 GBP), and reported as per patient per year (PPPY). Adjusted estimates were generated controlling for baseline characteristics, treatment assignment, and number of CID criteria met.
Results: Overall, 3,769 patients completed the study and were included in the analysis (stable CID- patients, n=1,832; unstable CID+ patients, n=1,937). At the end of follow-up, CID- patients had higher mean (95% confidence interval [CI]) utility scores than CID+ patients (0.752 [0.738, 0.765] vs 0.697 [0.685, 0.71]; difference +0.054; P<0.001), and lower costs PPPY (£538 vs £916; difference: £378 [95% CI: £244, £521]; P<0.001). The cost differential was primarily driven by the difference in general hospital ward days (P=0.003).
Conclusion: This study demonstrated that achieving early stability in COPD by preventing short-term CID is associated with better preservation of future QoL alongside reduced healthcare service costs.
Keywords: direct medical costs, EQ-5D, resource utilization, utilities
Plain language summary
Chronic obstructive pulmonary disease (COPD) is a complex and heterogeneous disease. Consequently, it would be helpful to evaluate disease stability and potential progression using outcomes that reflect this. Recently, clinically important deterioration (CID) was developed as an endpoint to capture important short-term changes in key clinical features (lung function, health status, and exacerbations), which indicate worsening of disease or disease instability. Studies have shown that early CID (assessed up to 26 weeks) can predict adverse long-term clinical outcomes. However, the impact of early CID on a patient’s future quality of life, healthcare service use and associated costs, is unknown. Data from the 3-year TOwards a Revolution in COPD Health (TORCH) clinical trial in moderate-to-very-severe COPD was examined in patients with early stability (CID- patients) or early instability (CID+ patients) during 6 months of treatment. In the current analysis, we compared the outcomes between CID- and CID+ patients in terms of subsequent annual costs, use of healthcare services and quality of life from the time their short-term CID status was confirmed until the end of the study (up to 2.5 years). Compared with CID+ patients, stable CID- patients had a better future quality of life and had lower future annual costs mainly due to lower hospital admission costs. These results suggest that achieving early disease stability in COPD might lead to better quality of life and healthcare cost savings in the long term.
Introduction
Chronic obstructive pulmonary disease (COPD) is a complex and heterogenous disease, characterized by persistent respiratory symptoms, specifically airway obstruction.1 COPD is a major cause of chronic morbidity and mortality worldwide,2–4 and is associated with a significant economic burden.2,5 In the European Union, COPD accounts for 56% (€38.6 billion) of the total cost of respiratory disease.2 In the United States, the estimated direct costs of COPD are $32 billion and indirect costs were estimated at $20.4 billion in 2010.2,6
Comprehensive assessment of COPD symptoms is recommended, including determination of the extent of airflow limitation, the impact of airflow limitation/dyspnea on the patient’s health status, and the risk of future events, thus allowing treatment to be individualized based on symptom severity and exacerbation risk.2,7 Developing a reliable method by which the potential for COPD progression in individuals could be routinely monitored, similar to identifying poor control in asthma patients,8,9 is a key objective on the pathway towards personalizing current clinical care.10 It will enable healthcare professionals to identify high-risk patients earlier, as well as identify the variety of factors that can best predict COPD outcomes. Given the complexity and heterogeneity of COPD, it is important that the method of measurement be multidimensional, to assemble a comprehensive picture of the potential for COPD progression.11,12
A novel composite endpoint assessing three dimensions of clinically important deterioration (CID) in COPD has been developed to assess and quantify individual levels of disease deterioration on treatment, and has been utilized to compare the effects of various therapies on maintaining short-term COPD stability.13 The CID endpoint has been used to demonstrate improved disease stability with dual fixed-dose long-acting muscarinic antagonist (LAMA)/long-acting β2-agonist (LABA) combination therapies compared with placebo, inhaled corticosteroid (ICS)/LABA dual therapy and LAMA or LABA monotherapies,13–17 and with triple therapy (ICS/LAMA/LABA in single or multiple inhaler[s]) compared with ICS/LABA18,19 and placebo added to ICS/LABA.20
While the clinical aspects of CID have been extensively studied, the economic and quality of life (QoL) impact of avoiding CID remains unclear. This study is the first to consider the costs and utilities associated with CID, in order to investigate if prevention of short-term instability may be associated with preservation of future QoL and reduced healthcare service costs, with consequent benefits to patients and payers.
Materials and methods
Objectives
The objective of this post hoc analysis of data prospectively collected over 3 years was to compare the long-term economic outcomes and utility consequences of COPD by patient CID status at Week 24, using data from the TOwards a Revolution in COPD Health (TORCH) study.21,22
Design and key results of the TORCH study
The TORCH study (NCT00268216)21,22 was a 3-year, multicenter, placebo-controlled, double-blind, randomized parallel group study conducted in 42 countries to examine the impact of COPD treatment on all-cause mortality. Study design and outcomes have been previously reported.21,22 In brief, after a 2-week run-in period, patients were randomized to one of four different treatment arms: fluticasone propionate (FP) 500 mcg; salmeterol (SAL) 50 mcg; FP/SAL 500/50 mcg; or placebo for 3 years. All-cause mortality rates were highest in the FP 500 mcg group (16.0%) and lowest in the FP/SAL 500/50 mcg group (12.6%). However, no significant reduction in all-cause mortality was observed with combination therapy, or either monotherapy, versus placebo.22 Secondary endpoints included QoL, assessed by total St George’s Respiratory Questionnaire (SGRQ) and Euro quality-of-life (EuroQoL) scores, lung function (assessed as the mean change in pre- and post-bronchodilator forced expiratory volume in 1 second [FEV1] from baseline to 3 years), and the frequency of moderate and severe exacerbations.
Study design
Population
Eligible patients for the TORCH trial were ≥40 years of age, with a diagnosis of COPD,23 current or former smokers (≥10-pack-year history), with a pre-bronchodilator FEV1<60% of the predicted value, <10% reversibility in predicted FEV1, and a ratio of pre-bronchodilator FEV1 to forced vital capacity of ≤70%. In this post hoc analysis, patients from the TORCH study population were included if they had complete available data to allow for determination of CID status on treatment at Week 24. This required at least one clinic visit after starting treatment, in which a lung function test and SGRQ were administered. A complete case analysis was conducted for all patients who did not withdraw from the study; therefore, patients were excluded from the analysis if they withdrew from the TORCH study at any time, or if they had incomplete data.
CID status was evaluated based on data collected until a maximum of 182 days (expected Week 24 visit +2 weeks) on randomized treatment, and was determined based on the absence (CID-) or presence (CID+) of at least one of the following three criteria denoting instability at or before Week 24: FEV1 ≥100 mL decline from baseline; or SGRQ total score ≥4-unit increase from baseline; or a moderate or severe exacerbation. Long-term economic outcomes and utility consequences were reported after 3 years of follow-up (Figure 1). No minimum or maximum window for the end of follow-up (Week 156 visit) was applied for patients who completed the study.
 | Figure 1 Study design. Abbreviation: CID, clinically important deterioration. |
Baseline variables used within this analysis were age, sex, body mass index (BMI), race, region, smoking status, number of pre-treatment COPD medications, number of prior exacerbations, modified Medical Research Council (mMRC) dyspnea score, FEV1, SGRQ, and EuroQol 5-dimensional scale (EQ-5D) utility index.
Outcomes
All outcomes were presented by short-term CID status (stable CID- or unstable CID+ patient subgroups) and stratified by the treatments investigated within the TORCH study.22
Resource utilization
Patient resource utilization was assessed from Week 24 to the end of follow-up and included: hospitalizations (number of general ward days and number of intensive care unit [ICU] days), the number of emergency department (ED) visits, the number of office visits, the number of home visits, and the number of outpatient visits.
Costs
All costs were based on 2016 Great British Pounds (GBP) and total direct medical costs were estimated based on reported healthcare resource utilization with unit costs applied for the United Kingdom (Table S1). Unit costs were sourced from the National Health Service (NHS) reference costs 2015–2016,24 or the Personal Social Service Research Unit.25
Utilities
Utility values were estimated from the EQ-5D health index using the recommended tariffs derived from a UK population survey.26 Utility change based on EQ-5D utility index was calculated from baseline to the end of follow-up, and from Week 24 to the end of follow-up. EQ-5D utility index data were only collected in 21 of the 42 participating countries for which validated translations of the instrument were available, so analyses of utility were restricted to study patients from those countries.
Statistical analyses
Multivariable adjustment was performed for all endpoints to account for possible selection bias due to only including patients who did not withdraw and for differences in patient characteristics given that categorization occurred post randomization. Adjusted analyses were conducted using the following covariates: age, sex, BMI, race, region, smoking status at baseline, number of prior COPD treatments, number of prior exacerbations, mMRC at baseline, FEV1 at baseline, CID status, treatment, CID status*CID type, and CID status*treatment. CID type was defined by the type (FEV1, SGRQ, or exacerbation CID) and number of CID criteria met by the patient. Baseline EQ-5D was also included as a covariate in the analyses of utilities. Linear regression was conducted for the utility outcomes. For resource use counts, generalized linear models with a negative binomial distribution were used. Missing data were assumed to most likely be due to withdrawal from the study. As data from patients who withdrew from the study were likely to be informative, inverse probability-weighting (IPW) was applied for all adjusted analyses.
Cost estimates were generated using a two-part modeling approach to properly account for patients with either zero observed costs or outlier costs from the top 3 costing patients. The two-part model was conducted as follows: part 1: run logistic regression to predict probability of having positive costs (P[Y>0], where Y=costs); part 2: run generalized linear model with a gamma distribution and log link among patients with positive costs (Y>0), then predict costs for the whole sample (E [Y|Y>0]). Adjusted mean cost estimates for each patient were calculated using the following equation: P(Y>0)*(E [Y|Y>0]); 95% confidence intervals (CI) were generated via 5,000 bootstrapped samples (sampling with replacement).
Results
Study population
In total, 8,554 patients were enrolled in the TORCH study, 6,184 (72.3%) were randomized and 6,112 (71.5%) were included in the efficacy population.22 Of the randomized patients, 3,769 patients completed the study and had data available at Week 24 for determination of CID status and thus were included in the post hoc analysis (stable CID- subgroup: N=1,832; unstable CID+ subgroup: N=1,937) (Figure 2). A summary of patient demographics and baseline characteristics is provided in Table 1.
 | Table 1 Baseline demographics and characteristics |
Resource utilization
From Week 24 to the end of follow-up, the stable CID- subgroup had significantly lower mean (95% CI) resource use per patient per year (PPPY) across a number of endpoints compared with the unstable CID+ subgroup, including the number of general ward days (mean difference −0.410; P=0.003), office visits (mean difference −0.191; P<0.001), home visits (mean difference −0.008; P<0.001) and outpatient visits (mean difference −0.067; P=0.029) (Table S2). Resource use by CID status and by treatment is presented in Table 2.
 | Table 2 Healthcare resource utilization by CID status and by treatment |
Costs
The total mean (95% CI) costs PPPY in the stable CID- subgroup were significantly lower than those in the unstable CID+ subgroup (£538 [458, 628] vs £916 [806, 1,050]; P<0.001) (Figure 3A). Similar results were seen when costs were analyzed by randomized treatment type, with the exception of SAL 50 mcg (Figure 3B).
Utilities
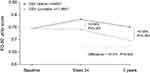
EQ-5D utilities were significantly higher in the stable CID- subgroup compared with the unstable CID+ subgroup at Week 24 (mean difference +0.043; P<0.001), and at end of the 3-year follow-up period (mean difference +0.054; P<0.001) (Figure 4). The mean (95% CI) change from baseline at 3 years was 0.005 (−0.009, 0.019) for the CID- subgroup and −0.049 (−0.061, −0.036) in the CID+ subgroup (difference: +0.054; P<0.001) (Table S2). There was no significant difference between the CID- and CID+ subgroups in change in utility from Week 24 to the end of follow-up (Figure 4/Table S2).
When analyzed by treatment, the difference in EQ-5D utility at the end of the 3-year follow-up between CID- and CID+ subgroups was statistically significant in all treatment groups (Table 3). Similar results were observed for the difference between CID status subgroups in EQ-5D utility change from baseline to end of follow-up in each treatment group (Table 3). The mean difference between CID subgroups was lowest within the FP 500 mcg treatment group, as a result of the lower utility scores within the stable CID- subgroup for this treatment (Table 3).22 Utilities at Week 24 were higher in the CID- versus the CID+ subgroup for all treatments, although the difference was not statistically significant for FP 500 mcg (Table 3). There was no significant difference between the CID- and CID+ subgroup in change in utility from Week 24 to end of follow-up in any of the treatment groups (Table 3).
 | Table 3 EQ-5D utility changes by CID status and by treatment |
Discussion
The results of this analysis suggested that overall, patients who were more stable (CID-) at the 6-month time point (Week 24) in the TORCH study had significantly better economic and QoL outcomes throughout the remaining period of assessment compared with those patients with a short-term CID (CID+). Patients with early CID events showed significantly lower EQ-5D utilities compared with more stable patients who remained free of CID events at 24 weeks. Early loss in utility established at Week 24 was still apparent at the end of the 3-year follow-up, highlighting that early loss in health status was not recovered in the follow-up period and may continue to be compounded with additional events. In addition, while these results demonstrated that CID- patients had significantly higher EQ-5D utilities compared with CID+ patients, the utility scores from 24 weeks to 3 years were generally stable with marginal subsequent changes, indicating that the key impact of CID was seen early in the study. Furthermore, the loss in EQ-5D in the CID+ subgroup was largely consistent across all treatment groups from Week 24 to the end of follow-up, indicating that CID status could be used as a measure of short-term responsiveness to treatment that may have long-term predictive value.
A study by Nolan et al suggested that change of >0.050 in EQ-5D utility can be considered clinically relevant.27 In the analysis presented here, the mean difference between the CID- and CID+ subgroups in EQ-5D utility change from baseline to the end of the 3-year follow-up period was +0.054, which suggests that avoiding early CID may be associated with higher EQ-5D utility scores and improvements in the patient’s subsequent perception of health. In terms of costs, the total mean costs PPPY in the CID- and CID+ subgroups were £538 and £916, respectively, resulting in a mean PPPY cost difference of £378 (41% lower costs for stable CID- patients). In comparison, the cost of a moderate exacerbation according to the NHS reference costs for 2010–2011, as used in a retrospective cohort study by Punekar et al, was £85.28 When adjusted to 2016 GBP,29 this cost would be £83, indicating that the observed annual cost saving PPPY associated with avoiding an early CID would be over 4 times higher than that of avoiding one moderate exacerbation.
In this analysis, resource use in the CID- subgroup was significantly lower than in the CID+ subgroup from Week 24 to the end of follow-up, across a number of endpoints, including general ward days, office visits, home visits, and outpatient visits. The cost differential between the CID status subgroups was largely driven by the difference in general ward days. This analysis suggests that achieving disease stability by preventing short-term CID may be associated with a reduction in costs generally related with worsening COPD. Data from the World Health Organization from 2008 indicated that the cost per bed per day in the UK was slightly more expensive than equivalent costs in Spain and Italy, but slightly cheaper than equivalent costs in France, Germany, and the USA, therefore placing the UK costs as somewhat of an average.30 The results of this analysis and the identification of general ward days as the defining cost driver for CID+ patients, could therefore be broadly applicable to other countries in Europe and to the USA. Costs by treatment group were consistent with the overall CID analysis, whereby all treatment groups demonstrated a statistically significant mean difference in favor of CID- patients, with the exception of the SAL 50 mcg treatment arm, for which the difference in annual costs per patient by CID status was not significant.
The correlation of short-term characterization of CID status with long-term clinical outcomes has been previously reported, using the combined data of TORCH22 and the Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE; NCT00292552)31,32 studies, both of which evaluated patients over a 3-year period.33 In both studies, CID+ patients had a clinically significant protracted deficit in FEV1 and health status and a higher risk of moderate or severe exacerbation (P<0.001 vs CID- subgroup), together with a higher all-cause mortality risk (P<0.05 vs CID-).33 Similarly, a post hoc analysis of the 4-year Understanding Potential Long-Term Impacts on Function with Tiotropium (UPLIFT; NCT00144339)34 study demonstrated that CID events at a 6-month interval predicted future moderate and severe exacerbations, as well as all-cause mortality.35 The increased hospitalization risk in CID+ patients has therefore been demonstrated from a clinical perspective and the results of this study suggest that these clinical observations may be supported by their corresponding long-term economic impact.
This study is the first to consider the economic and QoL outcomes associated with the emerging concept of short-term CID. While previous publications have demonstrated that short-term CID is associated with poor clinical outcomes,33,35 an understanding of the cost and utility implications of avoiding short-term CID through better disease management further bolsters the relevance of a monitoring tool to assess short-term stability in COPD for healthcare professionals, patients and payers, in order to optimize therapy and reduce irrecoverable costs. Furthermore, the analysis of utilities within this study, and the significant differences identified in utilities between CID- and CID+ patient subgroups, could be utilized within health technology assessments and cost-effectiveness evaluations. However, further studies are required to validate CID as a potential surrogate endpoint for these longer-term outcomes. The consideration of CID status by treatment within this study also highlights the potential value of applying this composite endpoint to the evaluation of COPD treatments earlier in a treatment’s clinical program to better demonstrate the combined clinical and economic strengths of the treatment versus standard of care therapies in COPD.
The results of this analysis demonstrate that stable patients without short-term CID have reduced costs and improved QoL in the long-term, compared with unstable CID+ patients. There are three possible explanations for this: 1. the stable CID- and unstable CID+ subgroups were inherently different at baseline and as such had different short- and long-term outcomes; 2. treatments that are effective/ineffective in the short-term continue to be effective/ineffective in the long-term; 3. treatments that stabilize COPD in the short-term prevent longer-term irrecoverable deterioration. Based on the current clinical evidence, we think that explanation 1 is unlikely. Our multivariate analyses focused on the study survivor population at 6 months and adjusted for baseline characteristics of CID- and CID+ subgroups by treatment, CID type at Week 24, and interaction between CID status at Week 24 and treatment. Moreover, the published CID analyses of the TORCH and ECLIPSE studies, which focused on clinical outcomes, demonstrated that the demographics and baseline characteristics of CID- and CID+ patients were generally similar.33 In addition, in the landmark COPD studies TORCH, ECLIPSE and UPLIFT, patients who had a CID event (according to the same definition of CID) in the first 6–12 months of these studies were found to have worse long-term outcomes, including increased mortality.33,36 The ECLIPSE and UPLIFT studies allowed for standard of care therapy to be adjusted over 3 or 4 years,31,34 and in the UPLIFT prognostic CID analysis, adjusting for important baseline predictors of risk did not diminish the power of the composite CID or any of its individual components to detect consistent increased mortality risk between CID+ and CID- patients.36 Therefore, together the evidence indicates that explanations 2 or 3 or a combination of these are more likely, and that short-term treatment failure assessed using CID is linked to long-term treatment failure and potential sustained disease progression. While it does not negate the need for other baseline assessment of prognosis (eg, comorbidities, exercise tolerance), the CID endpoint could provide a framework for the monitoring of short-term treatment failure advocated by the GOLD report,2 and could help identify patients with a high risk of disease progression and sustained poor long-term outcomes.
While this is the first analysis to consider economic and QoL outcomes of short-term CID status, the follow-up analysis was limited to 3 years, which, due to the chronic nature of COPD, may be perceived as insufficient. However, as this endpoint was associated with increased hospital admission costs in the current analysis, and with increased all-cause mortality in several other post hoc analyses of long-term interventional studies,33,36 the results from this study should nevertheless be strongly considered and further validated. A multi-component stability assessment based on CID events in several disease measures may also be considered less focused than monitoring exacerbations alone. However, in a recent 3-year follow up of the Danish National COPD Registry, higher respiratory and all-cause mortality was observed in symptomatic low exacerbation risk patients than in patients with fewer symptoms and a high exacerbation risk.37 Thus, the concept of disease stability measured across multiple disease dimensions may be important to identify future risk beyond exacerbations.
A limitation of this analysis is that the TORCH study assessed health status at 6-monthly intervals, therefore in this study it was only possible to assess CID status at Week 24. Patients who may have deteriorated at an earlier or later time point were therefore not categorized as CID+, thereby potentially reducing the observed cost and utility difference between the CID status subgroups. Inclusion of other more frequent timepoints for CID assessment would likely shed further light on the true cost and utility differences between these subgroups.
Moreover, this analysis focused on unscheduled resource use and costs, as collected per the TORCH protocol. Treatment-specific costs were not included because patients were pooled across treatment arms to assess the differences between the CID subgroups independent of treatment. Additionally, regular monitoring costs were not included as these would have been dictated by the trial protocol rather than reflecting real-world practice. Nevertheless, these are costs that should be considered to more completely evaluate the economic impact of CID.
Analyses of economic and QoL outcomes were also subject to the completeness of patient data available from the TORCH study. IPW was applied to all complete cases to account for patient withdrawals after the 6-month cut-off. There may nevertheless be potential bias in the estimation of the treatment-specific effects of the presence of CID, due to the heterogeneity within the CID subgroups across treatment arms. However, multivariate analysis was used to adjust for baseline characteristics of CID- and CID+ patient subgroups by treatment, CID type at the Week 24 visit, and interaction between CID status at Week 24 and treatment. Finally, as CID status allocation was not a randomized decision, there may be additional confounding variables that were not captured in the TORCH study and could therefore not be adjusted for in this specific analysis.
Conclusion
This study is the first to consider the economic and QoL outcomes associated with short-term CID. The results demonstrate that the occurrence of short-term CID, in addition to having long-term clinical consequences, is associated with sustained poorer QoL and higher health service costs. The improvements in long-term QoL and economic outcomes associated with early optimization of therapy to stabilize COPD therefore confer benefits from both the patient and the payer perspective. Although short-term CID needs to undergo further prospective validation, particularly in relation to whether later optimization of therapy prevents irrecoverable deterioration (ie if treatment escalation after the event can fully reverse the CID), it nevertheless appears to be a useful endpoint to assess the benefits of early optimal therapy in future clinical trials in COPD.
Abbreviation list
CI, confidence interval; CID, clinically important deterioration; CID+, with CID; CID-, without CID; COPD, chronic obstructive pulmonary disease; ED, emergency department; EQ-5D, EuroQol 5-dimensional scale; EuroQol, Euro quality-of-life; FEV1, forced expiratory volume in 1 second; FP, fluticasone propionate; FVC, forced vital capacity; GBP, Great British Pounds; ICS, inhaled corticosteroid; ICU, intensive care unit; IPW, inverse probability-weighting; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; mMRC, modified Medical Research Council; NHS, National Health Service; PPPY, per patient per year; QoL, quality of life; SAL, salmeterol; SGRQ, St George’s Respiratory Questionnaire; TORCH, TOwards a Revolution in COPD Health.
Ethics approval and informed consent
This article is based on a previously conducted study and does not involve any new studies of human or animal subjects performed by any of the authors. The study presented was an integrated post hoc analysis of a clinical trial conducted in accordance with the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use Good Clinical Practice guidelines and the principles of the Declaration of Helsinki. All participants provided written informed consent before participation in the studies considered in this analysis.
Data availability
The corresponding author had full access to all data. Anonymized individual participant data and study documents can be requested for further research from
Acknowledgments
Data within this manuscript were presented at the International Society for Pharmacoeconomics and Outcomes Research - 23rd International Meeting (poster: PRS19), the American Thoracic Society - 114th International Conference (poster: 10748), and at the European Respiratory Society International Conference 2018 (oral presentation). Editorial support (in the form of writing assistance, assembling tables and figures, collating author comments, grammatical editing and referencing) was provided by Emma Hargreaves and Elizabeth Jameson, PhD at Fishawack Indicia Ltd, UK, and was funded by GSK. This study was funded by GlaxoSmithKline (GSK; study number HO-16-16345). The funders of the study had a role in study design, data analysis, data interpretation, and writing of the report.
Author contributions
All named authors meet the International Committee of Medical Journal Editors criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, contributed to the writing and reviewing of the manuscript, and have given final approval of the version to be published. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. All authors were involved in the conception and design of the study and data analysis and interpretation.
Disclosure
IN, NBG, and ASI are employees of GSK, and hold stock/shares in GSK. ASI is also an unpaid professor at McMaster University in Canada. MTD was employed by GSK at the time of this study. VFP and NR are employees of ICON Health Economics, who were contracted by GSK to conduct the study analysis. AB received consultancy fees from GSK and ICON Health Economics in relation to this study. AB and ICON employees were not paid for manuscript development. The authors report no other conflicts of interest in this work.
References
1. Bringsvor HB, Skaug K, Langeland E, et al. Symptom burden and self-management in persons with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2018;13:365–373. doi:10.2147/COPD.S151428
2.
3. Lopez AD, Shibuya K, Rao C, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27(2):397–412. doi:10.1183/09031936.06.00025805
4.
5. Chapman KR, Mannino DM, Soriano JB, et al. Epidemiology and costs of chronic obstructive pulmonary disease. Eur Respir J. 2006;27(1):188–207. doi:10.1183/09031936.06.00024505
6. Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res. 2013;5:235–245. doi:10.2147/CEOR.S34321
7.
8. Reddel HK, Bateman ED, Becker A, et al. A summary of the new GINA strategy: a roadmap to asthma control. Eur Respir J. 2015;46(3):622–639. doi:10.1183/13993003.00853-2015
9.
10. Cardoso J, Coelho R, Rocha C, Coelho C, Semedo L, Bugalho Almeida A. Prediction of severe exacerbations and mortality in COPD: the role of exacerbation history and inspiratory capacity/total lung capacity ratio. Int J Chron Obstruct Pulmon Dis. 2018;13:1105–1113. doi:10.2147/COPD.S155848
11. Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005–1012. doi:10.1056/NEJMoa021322
12. Oga T, Tsukino M, Hajiro T, et al. Multidimensional analyses of long-term clinical courses of asthma and chronic obstructive pulmonary disease. Allergol Int. 2010;59(3):257–265. doi:10.2332/allergolint.10-RA-0184
13. Singh D, Maleki-Yazdi MR, Tombs L, Iqbal A, Fahy WA, Naya I. Prevention of clinically important deteriorations in COPD with umeclidinium/vilanterol. Int J Chron Obstruct Pulmon Dis. 2016;11:1413–1424. doi:10.2147/COPD.S101612
14. Anzueto AR, Vogelmeier CF, Kostikas K, et al. The effect of indacaterol/glycopyrronium versus tiotropium or salmeterol/fluticasone on the prevention of clinically important deterioration in COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:1325–1337. doi:10.2147/COPD.S133307
15. Maleki-Yazdi M. Clinically important deterioration in patients with COPD using umeclidinium/vilanterol, tiotropium or placebo: pooled data. Eur Respir J. 2015;46:P1001.
16. Singh D, D’Urzo AD, Chuecos F, Muñoz A, Gil EG. Reduction in clinically important deterioration in chronic obstructive pulmonary disease with aclidinium/formoterol. Respir Res. 2017;18(1):106. doi:10.1186/s12931-017-0583-0
17. Anzueto AR, Kostikas K, Mezzi K, et al. Indacaterol/glycopyrronium versus salmeterol/fluticasone in the prevention of clinically important deterioration in COPD: results from the FLAME study. Respir Res. 2018;19(1):121. doi:10.1186/s12931-018-0830-z
18. Lipson D, Compton C, Naya I. Prevention of early worsening of COPD with umeclidinium open triple therapy compared with inhaled corticosteroid/long-acting β2-agonist alone: a pooled post hoc analysis. Am J Respir Crit Care Med. 2017;195:A3608. doi:10.1164/rccm.201701-0150WS
19. Naya I, Compton C, Ismaila A, et al. Preventing clinically important deterioration with single-inhaler triple therapy in COPD. ERJ Open Res. 2018;4:00047–2018.
20. Naya I, Tombs L, Lipson DA, Compton C. Preventing clinically important deterioration of COPD with addition of umeclidinium to inhaled corticosteroid/long-acting β2-agonist therapy: an integrated post hoc analysis. Adv Ther. 2018;35(10):1626–1638. doi:10.1007/s12325-018-0771-4
21. Vestbo J;
22. Calverley PMA, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–789. doi:10.1056/NEJMoa063070
23. Celli BR, MacNee W, Agusti A, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932–946. doi:10.1183/09031936.04.00014304
24.
25.
26. Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095–1108.
27. Nolan CM, Longworth L, Lord J, et al. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax. 2016;71(6):493–500. doi:10.1136/thoraxjnl-2015-207782
28. Punekar YS, Shukla A, Müllerova H. COPD management costs according to the frequency of COPD exacerbations in UK primary care. Int J Chron Obstruct Pulmon Dis. 2014;9:65–73. doi:10.2147/COPD.S54417
29.
30.
31. Vestbo J, Anderson W, Coxson HO, et al. Evaluation of COPD longitudinally to identify predictive surrogate end-points (ECLIPSE). Eur Respir J. 2008;31(4):869–873. doi:10.1183/09031936.00111707
32. Agusti A, Calverley PM, Celli B, et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11(1):122. doi:10.1186/1465-9921-11-62
33. Naya IP, Tombs L, Muellerova H, Compton C, Jones PW. Long-term outcomes following first short-term clinically important deterioration in COPD. Respir Res. 2018;19(1):222. doi:10.1186/s12931-018-0928-3
34. Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–1554. doi:10.1056/NEJMoa0805800
35. Rabe KF, Halpin D, Martinez F, et al. Predicting long-term outcomes and future deterioration in COPD with a composite endpoint: post hoc analysis of the UPLIFT study. Am J Respir Crit Care Med. 2017;195:A2717. doi:10.1164/rccm.201701-0150WS
36. Han MK, Halpin DMG, Martinez FJ, et al. A composite endpoint of clinically important deterioration in chronic obstructive pulmonary disease and its association with increased mortality: a post hoc analysis of the UPLIFT study. Am J Respir Crit Care Med. 2018;197:A4245.
37. Gedebjerg A, Szépligeti SK, Wackerhausen L-MH, et al. Prediction of mortality in patients with chronic obstructive pulmonary disease with the new Global Initiative for Chronic Obstructive Lung Disease 2017 classification: a cohort study. Lancet Respir Med. 2018;6(3):204–212. doi:10.1016/S2213-2600(18)30002-X
Supplementary materials
 | Table S1 Direct medical costs included in the CID analysis |
 | Table S2 EQ-5D utility changes and health resource utilization by CID status |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.