Back to Journals » Nature and Science of Sleep » Volume 13
Long-Term Adherence to Positive Airway Pressure Therapy in Saudi Ambulatory Patients with Obesity Hypoventilation Syndrome and Severe Obstructive Sleep Apnea: A One-Year Follow-Up Prospective Observational Study
Authors Almeneessier AS , Aleissi S , Olaish AH , BaHammam AS
Received 4 November 2020
Accepted for publication 22 December 2020
Published 14 January 2021 Volume 2021:13 Pages 63—74
DOI https://doi.org/10.2147/NSS.S290349
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sarah L Appleton
Aljohara S Almeneessier,1,2 Salih Aleissi,1 Awad H Olaish,1 Ahmed S BaHammam1
1The University Sleep Disorders Center, Department of Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia; 2Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Correspondence: Ahmed S BaHammam
Medicine, University Sleep Disorders Center, Department of Medicine, College of Medicine, King Saud University, Box 225503, Riyadh 11324, Saudi Arabia
Tel +966-11-467-9495
Fax +966-11-467-9179
Email [email protected]
Purpose: Long-term studies assessing positive airway pressure (PAP) therapy adherence in patients with obesity hypoventilation (OHS) are limited. The aim of this study was to assess PAP therapy adherence in Arab (Saudi) patients with OHS and an apnea-hypopnea index (AHI) > 30/h.
Methods: A prospective cohort study of consecutive adult patients diagnosed with OHS between March 2010 and September 2019 was conducted. During the therapeutic sleep study, all OHS patients were started on continuous PAP (CPAP). Patients who failed to maintain oxygen saturation ≥ 88% despite the elimination of obstructive respiratory events were shifted to bi-level PAP (BPAP). Objective assessment of adherence was performed at 1, 6, and 12 months after initiating PAP therapy. We adopted the American-Thoracic-Society criteria for PAP adherence.
Results: The study included 101 patients (women = 65 patients) with OHS, an AHI ≥ 30/h, and a mean age of 54.9 ± 12.7 years. Successful titration on CPAP was achieved in 64.4% of the patients and BPAP was required for 35.6% of the patients who failed CPAP titration. At the end of the study, 43.6% of the patients used PAP therapy in an acceptable manner. Adherence after 1 and 6 months was the only independent predictors of adherence at 12 months.
Conclusion: PAP adherence among Saudi patients with OHS and severe obstructive sleep apnea was relatively low. Almost two-thirds of patients tolerated CPAP titration with the elimination of respiratory events and desaturation. Early adherence to PAP therapy was the only predictor of PAP therapy adherence at the end of the study.
Keywords: CPAP, bi-level positive airway pressure, compliance, obstructive sleep apnea, desaturation, titration
Introduction
Obesity hypoventilation syndrome (OHS) is characterized by chronic awake hypercapnia (PaCO2>45 mmHg, at sea level) and obstructive sleep apnea (OSA) in obese individuals (BMI>30kg/m2) in the absence of other causes of chronic hypercapnia.1 Burwell et al2 first described this condition as a “Pickwickian Syndrome” and limited treatment options were available, including weight loss, tracheostomy, and short-term breathing stimulants. Over the last 10 years, obesity rates increased worldwide,3 accompanied by increasing awareness of the high healthcare costs,4 morbidity, and mortality associated with OHS.4–6 Consequently, interest in the early diagnosis and treatment of OHS increased,7,8 and investigation into the long-term adherence to PAP therapy in OHS patients is essential.
The development of awake hypercapnia in OHS is the culmination of a complex interplay of factors, which vary from individual to individual. Factors contributing to hypercapnia in OHS patients include decreased lung volumes, increased respiratory system elastance, increased upper airway narrowing during wakefulness and sleep, subnormal respiratory drive to compensate for obesity, weakened inspiratory muscle function, and impaired chemoreceptor sensitivity to hypercarbia and hypoxia.9 Obstructive breathing during sleep is consistently present in most patients with OHS and is associated with periods of hypoventilation, particularly during rapid eye movement (REM) sleep.10 OSA occurs in approximately 90% of the OHS patients. The pure hypoventilation phenotype occurs in 10–15% of the patients.11
The aim of positive airway pressure (PAP) therapy is to normalize breathing and gas exchange during sleep. In OHS, this involves maintaining upper airway patency, improving alveolar ventilation, reducing the work of breathing, and eliminating hypoxemia. Patients with OHS can be divided into those with comorbid OSA and those with pure OHS and different PAP modes can be successfully used depending on the clinical phenotype and setting. Several studies compared the short or medium-term (up to 3 months) physiological outcomes of continuous positive airway pressure (CPAP) versus non-invasive ventilation (NIV) in patients with OHS and reported no superiority of either modality.12
Limited long-term studies have assessed adherence to PAP therapy in patients with OHS in Western societies. However, race is a predictor of adherence to PAP therapy in OSA patients.13–16 Thus, assessing PAP adherence in Arab (Saudi) patients with OHS is essential in understanding the impact on this patient population. To date, no study has reported adherence to PAP therapy in Arab patients with OHS. Due to the significant comorbidities and cognitive impairment associated with OHS,17 adherence to PAP therapy may be lower than adherence among OSA patients. We hypothesized that adherence of OHS patients with concomitant severe OSA [apnea-hypopnea index (AHI)≥30/h] to PAP therapy is below the standard recommendations (at least 4 hours per night, 70% of the recorded period). Therefore, this study sought to assess the adherence to PAP therapy in Arab (Saudi) patients with OHS and AHI≥30/h accompanied by close follow-up and monitoring with easy access to medical and technical support.
Methods
Subjects
This study is a part of a larger project, with prospectively collected data, to assess OHS.18–20 Consecutive patients (>18 years) who were diagnosed with OHS at the University Sleep Disorders Center (USDC) at King Saud University Medical City at King Saud University between March 2010 and September 2019 were approached to participate in the study (n=310). Exclusion criteria were chronic illnesses that may affect breathing, such as chronic neurological, muscular, or pulmonary disorders, deformity of the vertebral column or thoracic wall, decompensated congestive heart failure, and being on medications that suppress the respiratory drive such as hypnotics.
PAP adherence in OHS patients was compared with adherence in an age-, BMI-, and major comorbidity-matched group of OSA patients. In compliance with the USDC therapeutic policies, all patients had spirometric measurements based on the American Thoracic Society/European Respiratory Society (ATS/ERS) task force guidelines using a Master Screen (Jaeger, Germany).21 As an OHS diagnosis criterion, arterial blood samples were obtained from all patients with suspected OHS after 15 minutes of rest while awake, seated, and breathing room air using a GEM® Premier™ 4000 analyzer (Instrumentation Laboratory, Lexington, MA). The Epworth sleepiness scale (ESS) was used to assess daytime sleepiness.22 Incomplete data were completed by calling patients or relatives to obtain missing items. Comorbidities were obtained from patient histories and electronic medical records.
Polysomnography
As part of the clinical work-up, all patients with sleep-disordered breathing underwent a standard overnight sleep study (Type 1). The type 1 sleep study includes collection of neurological, cardiac, respiratory, and muscular data using EEG, chin and leg EMG, ECG, pulse oximeter, end-tidal CO2, and respiratory monitoring. Alice® diagnostic equipment (Philips, Respironics Inc., Murrysville, PA, USA) was used to acquire sleep study data. The scoring of raw data was performed manually and rechecked by certified staff according to the latest American Academy of Sleep Medicine (AASM) scoring criteria.23 The severity of obstructive sleep-disordered breathing was assessed using the AHI, which quantifies the number of apneas and hypopneas (obstructive events) per hour of sleep.
OHS Diagnosis
The third edition of the International Classification of Sleep Disorders Manual (ICSD-3) criteria was used to diagnose OHS. Diagnostic criteria included: 1) daytime hypercarbia (arterial PaCO2 >45 mm Hg), 2) obesity based on the World Health Organization (WHO) definition (BMI >30 kg/m2), and 3) exclusion of other causes of hypoventilation and daytime hypercarbia, such as chronic lung disease, chest wall deformity, respiratory suppressant medications, neuromuscular disorders, or idiopathic or congenital central alveolar hypoventilation syndrome.24 Patients with OHS were divided into two groups: OHS with a major obstructive sleep disorder (AHI≥30/h) and OHS with AHI<30/hr. In this study, we only included patients with AHI≥30/h.
PAP Therapy Titration Protocol
As per the USDC recommendations, all ambulatory patients with OHS were initially started on CPAP. If oxygen saturation could not be maintained at ≥88% despite the elimination of obstructive respiratory events, the patient was shifted to bi-level PAP (BPAP). All PAP devices had a built-in heated humidifier.
Definition of PAP Acceptance and Good Adherence
We adopted the American Thoracic Society (ATS) criteria for PAP adherence.25 The ATS criteria state that “good adherence” to PAP means “the use of PAP therapy regularly for more than 4 h/night for >70% of the recorded period” and “partial adherence” implies “the use of PAP therapy > 2 h/night that is accompanied by subjective improvement in OHS-related symptoms such as quality of life”.25 Patients who did not meet the above criteria were considered non-adherent.25 Adherence to PAP therapy was documented via downloading “mask-on time tracking” data from PAP devices. This technique permitted the objective estimation of adherence to PAP therapy.26
Follow-Up Protocol and PAP Adherence Assessment
As per the protocol of the USDC, patients with OHS were provided with information about the sleep study and PAP therapy by a health educationalist before undergoing the sleep study. A session was dedicated to selecting the best interface (mask) for PAP therapy. After the sleep study, a clinic visit was arranged for the patient and a family member, where a physician member of the USDC met patients and discussed the sleep study findings, diagnosis, known short-term and long-term complications of OHS, and the OHS complications and beneficial results and potential adverse events of PAP therapy. Following the clinic visit, an educational session was arranged with a health educationalist to have hands-on training for patients on the operation and components of PAP devices. Additionally, written educational material about OHS and PAP therapy was provided for all patients. During each subsequent follow-up visit, all practical educational points were repeated to patients.
Figure 1 demonstrates the study protocol. Patients spent two nights in the sleep laboratory; a diagnostic night was followed by a therapeutic night, where PAP was applied. The therapeutic study was performed within 2–3 weeks of the diagnostic study. Patients underwent three hands-on educational (training) sessions during the first month after the therapeutic sleep study. During these sessions, hands-on training sessions on operating PAP devices, interface application and removal, handling the humidifier and filter, and cleaning of PAP devices were reviewed. The following hands-on sessions were provided:
 |
Figure 1 A flowchart of the recruited patients. |
Session 1: The day they receive the PAP device
Session 2: Two weeks after initiating PAP therapy
Session 3: Four weeks after initiating PAP therapy
Outpatient follow-up of patients with OHS on PAP therapy was performed at 1, 6, and 12 months after initiating PAP therapy. During each visit, training and education were conducted and data about adverse events were collected. A dedicated sleep technologist worked with patients during each visit to solve PAP-related adverse events. Adherence to PAP therapy was objectively obtained from the PAP device during each visit. Patients were encouraged to adhere to treatment and the required adjustments were made to PAP settings and masks. Between follow-up visits, patients with OHS had direct access to medical and technical support by the USDC team via a direct phone number during daytime working hours and an accessible visit to the PAP therapy clinic if required within 1–2 weeks.
Statistical Analysis
Data are presented in the text and tables as mean ± standard deviation (SD) or number (%). Comparisons between groups were made using t-tests for continuous variables and Chi-square tests for dichotomous data. For three group comparisons, one-way analysis of variance (ANOVA) was used. To identify predictors of PAP adherence, we combined good adherence and partial adherence into a compliant group. A univariate logistic regression analysis was conducted whereby one independent variable was tested at a time in the model. Independent variables included demographics, clinical data, sleep study variables, and adverse events measured during each follow-up visit. Variables with significant p-values were included in the multivariable logistic regression analysis model. The correlation matrix assessed the multicollinearity between variables in the model, and no multicollinearity was detected. Moreover, the standard error in the model was used to reassess multicollinearity. A p-value < 0.05 was considered statistically significant. Data were analyzed using the SPSS statistical software (version 23; Chicago, IL, USA).
Results
During the study period, 129 patients were diagnosed with OHS with an AHI ≥30 and met the inclusion criteria; of whom 14 patients abandoned PAP therapy before the 12 months follow-up period, 13 did not show up for the final assessment, and one patient died during the follow-up period. These patients did not differ from those who completed the study regarding age, sex, BMI, comorbidities, AHI, mean nocturnal SpO2, baseline PaCO2, and PaO2, and type of PAP therapy prescribed. The remaining 101 patients (including 65 women) completed the study. All included patients were Arabs. The mean age of the study group was 54.9 ± 12.7 years, and the mean BMI of 43.4 ± 9.8 kg/m2. Patient characteristics at baseline are summarized in Table 1. Successful titration on CPAP was achieved in 64.4% of the patients; 35.6% failed CPAP titration and required BPAP. The mean CPAP and BPAP pressures were 12.6 ± 3.8 cmH2O and 18.5 ± 2.3/13.9 ± 3.1 cmH2O, respectively.
 |
Table 1 Baseline Characteristics of the Study Group According to PAP Adherence at 12 Months |
Figure 2 shows patient adherence at 1, 6, and 12 months of follow-up. At the end of the study, 43.6% of the patients were still using PAP therapy in an acceptable manner. Adherence in men and women is shown in Figures 3 and 4, respectively. At the end of the study, 49.3% of the women (Figure 3) and 33.3% of the men were still using PAP therapy in an acceptable way (good adherence + partial adherence). As patients were recruited from 2010 to 2019, improvements in PAP devices technology might have affected adherence. Therefore, we compared adherence across the 10 study years; no difference in adherence was detected between years from 2010 to 2019.
 |
Figure 2 PAP therapy adherence at 1, 6, and 12 months in the whole group. |
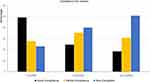 |
Figure 3 PAP therapy adherence at 1, 6, and 12 months in women. |
 |
Figure 4 PAP therapy adherence at 1, 6, and 12 months in men. |
No differences in the general characteristics, blood gases, spirometric parameters, PSG findings, comorbidities, the level of PAP used were observed in patient groups with good adherence, partial adherence, and non-adherence at the 12-month follow-up (Table 1). A comparison of adherence parameters in CPAP and BPAP users is shown in Table 2. No differences in adherence parameters were observed between the two groups.
 |
Table 2 Comparison of Adherence Between CPAP and BPAP Users |
Table 3 shows the univariate and multivariate regression analyses for the predictors of good adherence at 1, 6, and 12 months of follow up. At 1 month, no independent predictor could be identified. At 6 months, time with SpO2 <90% (mins), absence of side effects, and adherence (after 1 month) were the independent predictors of PAP adherence. Adherence after 1 month and adherence after 6 months were the only independent predictors of adherence at 12 months.
 |
Table 3 Independent Predictors of Good CPAP Adherence Using Univariate and Multivariate Logistic Regression at 1, 6, and 12 Months |
Table 4 shows a comparison of PAP adherence at 1, 6, and 12 months between patients with OHS and an age-, BMI-, and comorbidity-matched group of OSA patients. OHS patients had higher AHI and more desaturations compared to OSA patients. No differences in adherence between the two groups were detected.
 |
Table 4 Comparison of Demographics, Comorbidities, and PAP Adherence Between Patients with OHS and Age- and Body Mass Index-Matched OSA |
Discussion
This prospective observational study demonstrated that even with intensive education, support, and close monitoring, only 43.6% of the patients with OHS adhered to PAP therapy after 12 months of initiating therapy. This is much lower than the PAP adherence that our team has previously reported in Saudi patients with OSA (80%) after applying the same educational and follow-up program.27 However, the previously reported OSA patients were younger and had lower BMI and fewer comorbidities. Therefore, we compared OHS patients in this study with an OSA group matched for age, BMI, and major comorbidities. No difference in adherence was detected between the two groups.
Almost two-thirds of the patients in this study attained successful CPAP titration, indicating that CPAP can be successfully titrated in a majority of stable ambulatory OHS patients with AHI ≥ 30 events/h. However, age and comorbidities may influence PAP adherence in patients with sleep-disordered breathing. Studies have shown that patients with OHS have progressive disease paths, higher healthcare consumption, poorer prognoses, and increased likelihood of hospitalization and death compared with obese subjects without OHS and pure OSA patients.28,29
In a recent multicenter randomized controlled trial (RCT) of patients with OHS and an AHI >30 events/h, patients were followed for more than 5 years. This study reported a median treatment adherence for CPAP and NIV of 6 h per day, and among CPAP and NIV users, the percentage of those who used the device >4 h per day was 76% and 63%, respectively.30 In general, previous RCTs and observational studies in Western societies reported daily PAP use (among OHS patients) ranging from 4 to 6 h per day.31–33 Adherence to PAP among Saudi patients with OHS is lower than that reported in the West. This lower adherence is not related to access to medical care or the availability of the PAP devices. All Saudis and all government employees have free access to government-funded healthcare services and PAP devices.34 Additionally, studies in Western countries that showed high adherence to PAP therapy were RCTs. A prospective observational study in the US that used a study design comparable to our study reported objective adherence less than that reported in RCTs of 56%, which is closer to our study’s adherence rate.35 In the current study, PAP-related side effects were significantly high among non-adherents. Therefore, educational and support programs in local sleep disorders centers are needed to improve PAP therapy adherence among OHS patients. Additionally, close follow-up of patients on PAP therapy, particularly in the first few weeks of PAP use, is essential to resolve PAP-related side effects and enhance PAP adherence; poor adherence to PAP treatment has been linked to increased mortality.36 Moreover, good adherence to PAP therapy at 1 and 6 months was a predictor of adherence to PAP at 12 months, which further stresses the importance of early and close follow-up.
Telemedicine is a potentially powerful tool in improving adherence to PAP therapy, where actual adherence can be distantly measured.37,38 This technology may be beneficial in patients with OHS who usually have several comorbidities and have difficulties attending sleep disorders clinics.
In the current study, we found that two-thirds of OHS patients with AHI ≥30 events/h accepted and tolerated CPAP during titration, and there was no difference between adherence in the CPAP and BPAP groups. Several studies comparing the effectiveness of CPAP and NIV in OHS reported no superiority of one modality over the other on physiological outcomes and respiratory failure resolution in OHS patients with severe OSA.12 CPAP provides static pressure during both inspiration and expiration and does not directly augment minute ventilation. However, CPAP helps patients with OHS by eliminating upper airway repetitive obstructions during sleep and, hence, decreasing the mechanical load.1 By maintaining upper airway patency and removing the recurrent obstructive events, CPAP minimizes the cycle of low ventilation during upper airway obstructive periods and, subsequently, the resulting hypoxemic burden, CO2 accumulation, and longer-term bicarbonate preservation.39 Moreover, increased lung volume reduces airway resistance and flow limitations, leading to reduced work of breathing, particularly when in the recumbent position.40 In general, 50–80% of ambulatory stable OHS patients with comorbid OSA respond to CPAP.5,33,41,42 Additionally, CPAP is more cost-effective than BPAP and other modes of NIV.43 Therefore, CPAP should be the initial treatment for stable ambulatory patients with OHS associated with severe OSA due to its relatively simple application, low cost, and efficacy. If alveolar hypoventilation persists despite the elimination of obstructive events, patients should be switched to BPAP treatment.
The current study demonstrated no difference in adherence between patients on CPAP or BPAP. Our results concur with Howard et al, who reported no difference in adherence to CPAP and BPAP therapy among 60 OHS patients over three months.31 On the other hand, in a long-term prospective observational study, Bouloukaki et al reported that patients using BPAP adhered better to therapy than patients using CPAP [40].35 However, this study included OHS patients with mild, moderate, and severe OSA. In the current study, we only included patients with severe OSA. Our results also concur with a previous paper that assessed adherence to PAP among Saudi patients with moderate to severe OSA and reported no difference in adherence between CPAP and BPAP.27
Several studies have reported associations and predictors of PAP adherence among patients with OSA.15 However, limited data are available on the adherence to PAP therapy among patients with stable OHS. Age, BMI, daytime sleepiness (measured by the ESS), PAP pressure, and AHI did not predict subsequent PAP use in the current study. At month 6, the presence of side effects was an independent predictor of PAP adherence. Despite the progress in the design of PAP devices and interfaces, about 60% of the patients experience PAP-related side effects, which could affect long-term adherence.26 Therefore, patients should understand and report the side effects of PAP therapy so the treatment team can solve these problems to enhance treatment adherence.
The time spent with SPO2 less than 90% was a predictor of PAP adherence at 6 months. Several studies have demonstrated that increased OSA severity, measured by the AHI or oxygen desaturation index, may also affect adherence.15 An interesting finding is that adherence at 1 and 6 months were the only predictors of adherence at 12 months. Our findings concur with previous studies showing that early adherence to PAP in OSA patients could predict long-term adherence.44,45 Therefore, early support and interventions to troubleshoot problems are likely to improve adherence.46
A limitation of the current study is that the findings are from a single tertiary center. Hence, the data cannot be extrapolated to other sleep disorders centers in Saudi Arabia. Moreover, no data about the outcomes of physiological parameters were collected. Additionally, it would be interesting to show carbon dioxide levels during PSG monitoring in CPAP versus BPAP patients to detect differences in carbon dioxide levels during sleep in both groups and data on carbon dioxide levels or oxygen saturation among CPAP and BPAP users at the end of the study. Unfortunately, carbon dioxide levels are not available for all patients during PSG, nor arterial blood gases result at the end of the study. Future studies should monitor and report these parameters.
In summary, this is the first study to assess the acceptance and long-term adherence to PAP in Arab patients with OHS. The current long-term prospective study demonstrates that PAP adherence among Saudi patients with OHS and concomitant severe OSA is lower than the adherence reported in Western patients. The adherence reported in this study is also lower than adherence in Saudi patients with moderate to severe OSA. During this therapeutic study, almost two-thirds of OHS patients tolerated CPAP titration with the elimination of respiratory events and desaturation. Adherence to PAP therapy in the first and sixth month was the only predictor of PAP therapy adherence at the end of the study, indicating the importance of close follow-up of OHS patients on PAP therapy. In particular, close monitoring in the first few weeks of PAP therapy is important to resolve PAP therapy-related side effects and enhance adherence to PAP therapy. Future studies should assess the impact of PAP adherence on physiological parameters among Arab patients with OHS.
Data Sharing Statement
Data are available upon request. However, releasing data needs IRB approval.
Ethics Statement
Ethical approval of the study protocol was obtained from the Institutional Review Board (IRB) of the College of Medicine, King Saud University, and Medical City. All participants gave written informed consent. This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgment
This study was supported by a grant from the “Strategic Technologies Program of the National Plan for Sciences and Technology and Innovation in the Kingdom of Saudi Arabia (08-MED511-02)”. In this paper, we remember the coauthor Awad H. Olaish who passed away before the publication of the paper; we all miss you.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Piper AJ, BaHammam AS, Javaheri S. Obesity hypoventilation syndrome: choosing the appropriate treatment of a heterogeneous disorder. Sleep Med Clin. 2017;12(4):587–596. doi:10.1016/j.jsmc.2017.07.008
2. Bickelmann AG, Burwell CS, Robin ED, Whaley RD. Extreme obesity associated with alveolar hypoventilation; a Pickwickian syndrome. Am J Med. 1956;21(5):811–818. doi:10.1016/0002-9343(56)90094-8
3. Collaboration NCDRF. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–1396. doi:10.1016/S0140-6736(16)30054-X
4. Jennum P, Kjellberg J. Health, social and economical consequences of sleep-disordered breathing: a controlled national study. Thorax. 2011;66(7):560–566. doi:10.1136/thx.2010.143958
5. Castro-Anon O, Perez de Llano LA, De la Fuente Sanchez S, et al. Obesity-hypoventilation syndrome: increased risk of death over sleep apnea syndrome. PLoS One. 2015;10(2):e0117808. doi:10.1371/journal.pone.0117808
6. Nowbar S, Burkart KM, Gonzales R, et al. Obesity-associated hypoventilation in hospitalized patients: prevalence, effects, and outcome. Am J Med. 2004;116(1):1–7. doi:10.1016/j.amjmed.2003.08.022
7. Egea-Santaolall AC, Javaheri S. Obesity hypoventilation syndrome. Curr Sleep Med Rep. 2016;2(12–19). doi:10.1007/s40675-016-0035-2
8. Piper A. Obesity hypoventilation syndrome: weighing in on therapy options. Chest. 2016;149(3):856–868. doi:10.1378/chest.15-0681
9. Piper AJ, Grunstein RR. Big breathing: the complex interaction of obesity, hypoventilation, weight loss, and respiratory function. J Appl Physiol (1985). 2010;108(1):199–205. doi:10.1152/japplphysiol.00713.2009
10. Berger KI, Ayappa I, Chatr-Amontri B, et al. Obesity hypoventilation syndrome as a spectrum of respiratory disturbances during sleep. Chest. 2001;120(4):1231–1238. doi:10.1378/chest.120.4.1231
11. Al Dabal L, Bahammam AS. Obesity hypoventilation syndrome. Ann Thorac Med. 2009;4(2):41–49. doi:10.4103/1817-1737.49411
12. Murphy PB, Piper AJ, Hart N. Obesity hypoventilation syndrome: is less really more? Lancet. 2019;393(10182):1674–1676. doi:10.1016/S0140-6736(19)30248-X
13. Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653–1658. doi:10.5665/sleep.1428
14. Means MK, Ulmer CS, Edinger JD. Ethnic differences in continuous positive airway pressure (CPAP) adherence in veterans with and without psychiatric disorders. Behav Sleep Med. 2010;8(4):260–273. doi:10.1080/15402002.2010.509255
15. Mehrtash M, Bakker JP, Ayas N. Predictors of continuous positive airway pressure adherence in patients with obstructive sleep apnea. Lung. 2019;197(2):115–121. doi:10.1007/s00408-018-00193-1
16. Scharf SM, Seiden L, DeMore J, Carter-Pokras O. Racial differences in clinical presentation of patients with sleep-disordered breathing. Sleep Breath. 2004;8(4):173–183. doi:10.1055/s-2004-860894
17. Masa JF, Pepin JL, Borel JC, Mokhlesi B, Murphy PB, Sanchez-Quiroga MA. Obesity hypoventilation syndrome. Eur Respir Rev. 2019;28:151. doi:10.1183/16000617.0097-2018
18. BaHammam AS. Prevalence, clinical characteristics, and predictors of obesity hypoventilation syndrome in a large sample of Saudi patients with obstructive sleep apnea. Saudi Med J. 2015;36(2):181–189. doi:10.15537/smj.2015.2.9991
19. BaHammam AS, Aleissi S, Olaish AH, Almeneessier AS, Jammah AA. Prevalence of hypothyroidism in a large sample of patients with obesity hypoventilation syndrome. Nat Sci Sleep. 2020;Volume 12:649–659. doi:10.2147/NSS.S263959
20. BaHammam AS, Pandi-Perumal SR, Piper A, et al. Gender differences in patients with obesity hypoventilation syndrome. J Sleep Res. 2016;25(4):445–453. doi:10.1111/jsr.12400
21. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
22. Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15(4):376–381. doi:10.1093/sleep/15.4.376
23. Berry RB, Brooks R, Gamaldo CE, et al., The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.1. American Academy of Sleep Medicine; Darien, Illinois: 2014. www.aasmnet.org.
24. American Academy of Sleep Medicine (AASM). International Classification of Sleep Disorders (ICSD).
25. Schwab RJ, Badr SM, Epstein LJ, et al. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188(5):613–620. doi:10.1164/rccm.201307-1282ST
26. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245–258.
27. BaHammam AS, Alassiri SS, Al-Adab AH, et al. Long-term compliance with continuous positive airway pressure in Saudi patients with obstructive sleep apnea. A prospective cohort study. Saudi Med J. 2015;36(8):911–919. doi:10.15537/smj.2015.8.11716
28. BaHammam A. Acute ventilatory failure complicating obesity hypoventilation: update on a ‘critical care syndrome’. Curr Opin Pulm Med. 2010;16(6):543–551. doi:10.1097/MCP.0b013e32833ef52e
29. Berg G, Delaive K, Manfreda J, Walld R, Kryger MH. The use of health-care resources in obesity-hypoventilation syndrome. Chest. 2001;120(2):377–383. doi:10.1378/chest.120.2.377
30. Masa JF, Mokhlesi B, Benitez I, et al. Long-term clinical effectiveness of continuous positive airway pressure therapy versus non-invasive ventilation therapy in patients with obesity hypoventilation syndrome: a multicentre, open-label, randomised controlled trial. Lancet. 2019;393(10182):1721–1732. doi:10.1016/S0140-6736(18)32978-7
31. Howard ME, Piper AJ, Stevens B, et al. A randomised controlled trial of CPAP versus non-invasive ventilation for initial treatment of obesity hypoventilation syndrome. Thorax. 2017;72(5):437–444. doi:10.1136/thoraxjnl-2016-208559
32. Masa JF, Corral J, Alonso ML, et al. Efficacy of different treatment alternatives for obesity hypoventilation syndrome. Pickwick Study. Am J Respir Crit Care Med. 2015;192(1):86–95. doi:10.1164/rccm.201410-1900OC
33. Piper AJ, Wang D, Yee BJ, Barnes DJ, Grunstein RR. Randomised trial of CPAP vs bilevel support in the treatment of obesity hypoventilation syndrome without severe nocturnal desaturation. Thorax. 2008;63(5):395–401. doi:10.1136/thx.2007.081315
34. Almeneessier AS, BaHammam AS. Sleep medicine and sleep disorders in Saudi Arabia and the Arab World. In: Laher I, editor. Handbook of Healthcare in the Arab World. Cham: Springer; 2019:1–16. doi:10.1007/1978-1003-1319-74365-74363_74145-74361
35. Bouloukaki I, Mermigkis C, Michelakis S, et al. The association between adherence to positive airway pressure therapy and long-term outcomes in patients with obesity hypoventilation syndrome: a prospective observational study. J Clin Sleep Med. 2018;14(9):1539–1550. doi:10.5664/jcsm.7332
36. Pierce AM, Brown LK. Obesity hypoventilation syndrome: current theories of pathogenesis. Curr Opin Pulm Med. 2015;21(6):557–562. doi:10.1097/MCP.0000000000000210
37. Hwang D, Chang JW, Benjafield AV, et al. Effect of telemedicine education and telemonitoring on continuous positive airway pressure adherence. The Tele-OSA randomized trial. Am J Respir Crit Care Med. 2018;197(1):117–126. doi:10.1164/rccm.201703-200582OC
38. Pirzada A, Awadh AA, Aleissi SA, Almeneessier AS, BaHammam AS. Reopening sleep medicine services in the Conundrum of an ongoing COVID-19 pandemic: a global view. Sleep Vigil. 2020;4:1–8. doi:10.1007/s41782-41020-00100-w
39. Berger KI, Goldring RM, Rapoport DM. Obesity hypoventilation syndrome. Semin Respir Crit Care Med. 2009;30(3):253–261. doi:10.1055/s-0029-1222439
40. Onofri A, Patout M, Kaltsakas G, et al. Neural respiratory drive and cardiac function in patients with obesity hypoventilation syndrome following initiation of non-invasive ventilation. J Thorac Dis. 2018;10(Suppl 1):S135–S143. doi:10.21037/jtd.2017.12.129
41. Mokhlesi B, Tulaimat A, Evans AT, et al. Impact of adherence with positive airway pressure therapy on hypercapnia in obstructive sleep apnea. J Clin Sleep Med. 2006;2(1):57–62. doi:10.5664/jcsm.26436
42. Salord N, Mayos M, Miralda RM, et al. Continuous positive airway pressure in clinically stable patients with mild-to-moderate obesity hypoventilation syndrome and obstructive sleep apnoea. Respirology. 2013;18(7):1135–1142. doi:10.1111/resp.12131
43. Masa JF, Mokhlesi B, Benitez I, et al. Cost-effectiveness of positive airway pressure modalities in obesity hypoventilation syndrome with severe obstructive sleep apnoea. Thorax. 2020;75(6):459–467. doi:10.1136/thoraxjnl-2019-213622
44. Budhiraja R, Parthasarathy S, Drake CL, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep. 2007;30(3):320–324.
45. Sunwoo BY, Light M, Malhotra A. Strategies to augment adherence in the management of sleep-disordered breathing. Respirology. 2020;25(4):363–371. doi:10.1111/resp.13589
46. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430–435. doi:10.1378/chest.121.2.430
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
