Back to Journals » Clinical Ophthalmology » Volume 8
Long-lasting effects of anti-VEGF/photodynamic combination therapy in the treatment of exudative age-related macular degeneration: a retrospective chart review
Authors Silva-Garcia R, McLellan C, Shaya F, Small K
Received 20 May 2014
Accepted for publication 4 July 2014
Published 15 December 2014 Volume 2014:8 Pages 2529—2532
DOI https://doi.org/10.2147/OPTH.S68028
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Rosemary Silva-Garcia, Colleen McLellan, Fadi S Shaya, Kent W Small
Macula and Retina Institute, Molecular Insight Research Foundation, Cedars-Sinai Medical Towers, Glendale, CA, USA
Purpose: To examine the potential long-term benefit of an anti-VEGF/photodynamic therapy (PDT) combination on patients treated for wet age-related macular degeneration (AMD).
Methods: A retrospective chart review was conducted on 29 eyes (subjects) from 26 patients (eight male and 18 female) that showed sustained, positive response to combination therapy for exudative AMD for a minimum of 1 year. Collected data included: visual acuity, central retinal thickness, intraocular pressure and history of glaucoma, wet AMD onset and treatment history, concomitant use of anticoagulants and past history or development of cerebrovascular or cardiovascular disease while receiving combination therapy.
Results: Subjects underwent an average of five injections and two PDT treatments in total over 16 months before the choroidal neovascular membrane (CNVM) stabilized and became inactive for at least 1 year. Prior to the effective anti-VEGF/PDT combination therapy the median Snellen visual acuity ranged from 20/200 to 20/250 and presented at no worse than 20/200 at 1 year after treatment. Some subjects were followed for up to 5 years and remained inactive.
Conclusion: Combination therapy can cause long-lasting closure of the CNVM, even with advanced disease resistant to anti-VEGF monotherapy.
Keywords: anti-vascular endothelial growth factor, photodynamic therapy, age-related macular degeneration, bevacizumab, visual acuity, intraocular pressure
Introduction
The US Food and Drug Administration (FDA) standard of care for neovascular age-related macular degeneration (AMD) includes photodynamic therapy (PDT) and intravitreal injections of anti-VEGF.1 Studies have shown that anti-VEGF injections are more effective than PDT when used as a monotherapy, still; anti-VEGF injections given at intervals ranging from every 4 to every 6 weeks are usually required in order to control neovascular membranes in wet AMD. Intravitreal injections are performed by retina specialists on a daily basis and the overall risk for complication is low when performed properly. However, some complications could be associated with severe vision loss. Known complications include subconjunctival hemorrhage and retinal tears, as well as the more serious retina detachments, vitreous hemorrhage, uveitis, and endophthalmitis.2–4 Previous research has suggested that visual acuity (VA) outcomes are comparable between anti-VEGF monotherapy and anti-VEGF/PDT combination treatment, the latter with significantly fewer interventions.3,5 With further study, a combination approach may reduce the overall need for AMD treatments as well as their potential for ocular or systemic complications.
Methods
The study consisted of a retrospective chart review (26 patients, 29 study eyes) from a solo retina specialty practice in Los Angeles, California (two different locations) for whom combination treatment with anti-VEGF injection (bevacizumab) and PDT effectively halted the growth of neovascular membranes and the need for further treatments in one or both eyes for at least 1 year. Charts were reviewed for up to 5 years for the eyes remaining during this period. Institutional Review Board approval for this study was obtained. The review included only the charts of patients who completed combination therapy with PDT and an anti-VEGF intravitreal injection within 1 week. The study only included the eyes that resulted in lasting (minimum of 1 year) lack of evidence of active choroidal neovascular membranes (CNVM) after combination therapy. In most of the subjects the following elements were used to determine inactivity of the CNVM; retina examination notes including extended ophthalmoscope, VA, fluorescein angiography and optical coherence tomography (OCT) assessment records.
VA was recorded using the Snellen chart. In cases where VA was below 20/400, VA was estimated by the individual’s precision in calling the number of fingers presented or perception of hand motion at an estimated distance. VA statistics are expressed as a median value per year since the effective combination treatment. Central macula thickness in μm was measured by OCT; variances from baseline were analyzed per year. Charts from two different office locations were reviewed. Hence, the use of two different OCT instruments: a Carl Zeiss OCT 3 Stratus (Carl Zeiss Meditec AG, Jena, Germany) or OPKO SD-OCT (OPKA Health Inc., Miami, FL, USA).
Intraocular pressures were measured by applanation tonometry. Intraocular pressure readings and glaucoma medication use prior to effective combination therapy and yearly afterwards for up to 5 years were registered, accounting for whether the eye treated for glaucoma was also being treated for wet AMD.
Additional documentation about the patient’s age at time of effective combination therapy, the total number of anti-VEGF injections and PDT received per study eye throughout the review period and concomitant anticoagulant use such as, aspirin, clopidogrel, Coumadin or a combination of any of those preparations, was also logged. Descriptive statistical analyses were performed as the dataset was too small for meaningful comparative statistical analyses.
Results
Eight out of the 29 eyes studied were from four patients with bilateral exudative AMD. The overall mean age at the time of effective combination therapy (PDT plus anti-VEGF) was 80.2 years, with a range from 67 to 92 years of age. Prior to effective combination therapy, the study eyes were treated with monotherapy of an anti-VEGF intravitreal injection in an average of 5 (range; 1–18) or PDT in an average of 2 (range; 1–8). All of these eyes would be considered to be refractory to anti-VEGF therapy alone and most eyes had large chronically active CNVM. Such monotherapy was administered for an average of 16.13±17.35 months before the CNVM was stabilized by combination therapy and required no further treatment for at least 1 year.
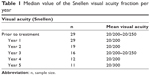
Median VA before the effective combination treatment was between 20/200 and 20/250 (n=29). One year post effective combination treatment the median VA was 20/200 (n=29), and at the end of the second, third, fourth, and fifth year the median VA consisted of 20/200 (n=19), 20/200–20/250 (n=16), 20/200 (n=12) and 20/300 (n=11) respectively as seen in Table 1.
|
Table 1 Median value of the Snellen visual acuity fraction per year |
The mean changes in central macula thickness from baseline (prior to effective combination therapy) throughout the 5 years are represented in Figure 1. The values for each year are the following: first year post combination treatment mean 49.22±73.79 (range; −198 to 79 μm) (n=23), the second year mean of 85.70±102.10 (range; −255 to 166 μm) (n=12), the third year mean of 43.11±95.92 (range; −208 to 77 μm) (n=9), the fourth year mean of 75.33±123.78 (range; −209 to 167) (n=5) and the fifth year with a mean of 62.00±141.11 (range; −228 to 116 μm) (n=6).
 
|
Figure 1 Mean value of the changes in central macula thickness (expressed in microns and measured by optical coherence tomography) per year. |
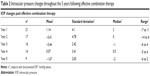
Mean changes in intraocular pressure readings from baseline were 1.14±4.16 mmHg (n=21) in the first year, −0.41±4.78 mmHg (n=17) in the second year, −0.44±2.42 mmHg (n=16) in the third year, 0.07±3.41 mmHg (n=14) in the fourth year and −1.67±2.65 mmHg (n=9) in the fifth year, evident in Table 2. The error bars on the graphs represent the standard deviation. The study produced a wide range of scores with respect to treatment administration period, changes in intraocular pressures and central macula thickness that led to the standard deviations being large.
|
Table 2 Intraocular pressure changes throughout the 5 years following effective combination therapy |
Missing data and lost to follow-up resulted in inconsistent “n” value throughout the 5 years with respect to VA, intraocular pressure, and central macula thickness variables.
At baseline, the following anticoagulants were used concomitantly: aspirin (13 eyes), clopidogrel (two eyes), and Coumadin (three eyes). Reason for anticoagulation therapy was not documented. No records of new onset of cerebrovascular accidents or ischemic heart disease were found during the 5 years following effective combination therapy with the exception of one report of atrial fibrillation. No documentation was found with respect to a new anticoagulation treatment being established during the 5 year period for any of the subjects or in the new case of atrial fibrillation.
Two study eyes were receiving glaucoma medication prior to combination therapy and two additional study eyes began using glaucoma drops during the 5 years following combination treatment. The study did not include data on the fellow eyes except, it is worth mentioning that three fellow eyes began using glaucoma medication during the review period concomitantly with anti-VEGF intravitreal injections as a single therapy.
Discussion
In managing any patient disease, one goal of a physician is to achieve the best outcome possible for the patient with the fewest interventions, therefore minimizing risk. Combination therapy of anti-VEGF injections with PDT may offer such a possibility.
Between 2005 and 2008, nearly 21,000 anti-VEGF injections were administered to 6,154 Medicare patients age 68 and over, an age group which is anticipated to more than double in size by 2040.4,6 Treatments with anti-VEGF medications have been a great advance in managing patients with wet AMD; nonetheless, this also implies an increase in care expenses.7 Besides the financial concern, the need for frequent injections places a burden on patients, families, and physician offices. Most complications from anti-VEGF injections are rare. However, there are new data suggesting that these treatments are associated with increasing risk of glaucoma in addition to the risks mentioned above. One study found that with two or more intravitreal anti-VEGF injections, an intraocular pressure elevation of >5 mmHg from the baseline becomes more likely.8 The abovementioned event about the three fellow eyes starting glaucoma treatment while receiving anti-VEGF intravitreal injections during the review period, may suggest that secondary glaucoma is related to injection treatment, thus supporting that study.8 Secondary glaucoma and other aforementioned side effects are substantial factors in determining the duration and frequency of a patient’s care for exudative AMD.
Regardless of their extensive co-morbidities, no new events of cerebrovascular accidents or ischemic heart disease were reported in the years observed after effective combination therapy, with the exception of one case of new onset of atrial fibrillation. The risk of these adverse events has been reported to be higher in PDT monotherapy than in anti-VEGF injection monotherapy.9 Further research is needed to determine whether the benefits of combination therapy for exudative AMD may outweigh the slightly increased risk of stroke or heart attack with PDT. No cataract progression or endophthalmitis was observed during the combination treatment phase. In addition, the 13 eyes pretreated with aspirin showed no evidence of a correlation with the anti-VEGF/PDT combination therapy.
The data in this study were inconclusive as to why the eyes we studied responded effectively in the long-term to combination therapy. It appears that with combination therapy, exudative AMD can be effectively managed and a patient’s exposure to side effects minimized. When compared to indefinite treatment with mostly anti-VEGF injections, combination therapy may also improve a patient’s quality of life by shortening the overall duration of treatment.
The obvious weaknesses of this study are the relative small size, retrospective chart review, and the fact that we do not have the total number of patients treated with combination therapy. This latter point obviously introduces a selection bias but the major point of this study is that despite the results of the DENALI and MONT BLANC studies,10,11 there are a significant number of patients who do very well with combination therapy in the real world experience. As stated in the 12 month MONT BLANC and DENALI studies, non-inferiority of combination treatment over anti-VEGF monotherapy did not display any significance. Non-inferiority does not mean that there is not a significant number of patients who can benefit from combination therapy. As with any prospective randomized trial, MONT BLANC and DENALI give us general guidelines based on their specific study design, which can have limited application to the real world experience. Perhaps genotyping these subjects for AMD risk alleles might reveal other factors for favorable responders to combination therapy.
Disclosure
None of the authors have any conflicting interests to disclose. A small IST (Investigator Sponsored Trial grant) was provided by Valeant Pharmaceuticals International, Inc.
References
Ramulu PY, Do DV, Corcoran KJ, et al. Use of Retinal Procedures in Medicare Beneficiaries From 1997 to 2007. Arch Ophthalmol. 2010;128(10):1335–1340. | ||
Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group; Martin DF, Maguire MG, et al. Ranibizumab and Bevacizumab for Treatment of Age-Related Macular Degeneration: 2-Year Results. Ophthalmology. 2012;119(7):1388–1398. | ||
Bressler NM, Chang TS, Fine JT, et al. Improved Vision-Related Function After Ranibizumab vs Photodynamic Therapy: A Randomized Clinical Trial. Arch Ophthalmol. 2009;127(1):13–21. | ||
Day S, Acquah K, Mruthyunjaya P, et al. Ocular complications after anti-vascular endothelial growth factor therapy in Medicare patients with age-related macular degeneration. Am J Ophthalmol. 2011;152(2):266–272. | ||
Heier JS, Boyer DS, Ciulla TA, et al. Ranibizumab combined with verteporfin photodynamic therapy in neovascular age-related macular degeneration: year 1 result of the FOCUS study. Arch Ophthalmol. 2006;124(11):1532–1542. | ||
US Census Bureau [homepage on the Internet]. 2008 National Population Projections. US Census Bureau. Available from: https://www.census.gov/population/projections/data/national/2008/summarytables.html. Accessed August 20, 2012. | ||
Brechner RJ, Rosenfeld PJ, Babish D, Caplan S. Pharmacotherapy for Neovascular Age-Related Macular Degeneration: An Analysis of the 100% 2008 Medicare Fee-For-Service Part B Claims File. Am J Ophthalmol. 2010;151(5):887–895. | ||
Hoang QV, Mendonca LS, Della Torre KE, Jung JJ, Tsuang AJ, Freund KB. Effect on intraocular pressure in patients receiving unilateral intravitreal anti-vascular endothelial growth factor injections. Opthalmology. 2012;119(2):321–326. | ||
Curtis LH, Hammill BG, Schulman KA, Cousins SW. Risks of mortality, myocardial infarction, bleeding, and stroke associated with therapies for age-related macular degeneration. Arch Ophthalmol. 2010;128(10):1273–1279. | ||
Kaiser PK, Boyer DS, Cruess AF, et al. Verteporfin plus ranibizumab for choroidal neovascularization in age-related macular degeneration: Twelve-month results of the DENALI study. Ophthalmology. 2012;119(5):1001–1010. | ||
Larsen M, Schmidt-Erfurth U, Lanzetta P, et al. Verteporfin plus ranibizumab for choroidal neovascularization in age-related macular degeneration: Twelve-month MONT BLANC study results. Ophthalmology. 2012;119(5):992–1000. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
