Back to Journals » Journal of Pain Research » Volume 12
Local ozone (O2–O3) versus corticosteroid injection efficacy in plantar fasciitis treatment: a double-blinded RCT
Authors Bahrami MH, Raeissadat SA, Barchinejad M, Elyaspour D , Rahimi-Dehgolan S
Received 24 January 2019
Accepted for publication 27 June 2019
Published 24 July 2019 Volume 2019:12 Pages 2251—2259
DOI https://doi.org/10.2147/JPR.S202045
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor E Alfonso Romero-Sandoval
Mohammad Hassan Bahrami,1 Seyed Ahmad Raeissadat,2 Mahboobeh Barchinejad,2 Dariush Elyaspour,2 Shahram Rahimi-Dehgolan3
1Physical Medicine and Rehabilitation Department and Research Center, School of Medicine, Shohada-e-tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 2Clinical Development Research Center of Shahid Modarres Hospital, Physical Medicine and Rehabilitation Department and Research Center, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 3Physical Medicine and Rehabilitation Department, School of Medicine, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences (TUMS), Tehran, Iran
Purpose: To compare the efficacy of local ozone injection versus corticosteroid in plantar fasciopathy treatment.
Patients and methods: This double-blinded randomized trial was performed on 44 adult patients with plantar fasciopathy. One group (23 patients) received local injection of 40 mg methylprednisolone, while a local injection of 3 cc oxygen-ozone solution was performed for the other group (21 subjects). Severity of pain, functional level, and pressure-pain threshold (PPT) were measured before treatment and 1, 4, and 12 weeks after injection using VAS, Foot and Ankle Ability Measure (FAAM) questionnaire, and algometer for PPT, respectively.
Results: The majority (65.9%) of the total 44 patients analyzed, were women. Both treatments efficiently relieved patients’ pain and improved their functions at 1 and 3 months follow-up time-points. But one week after injection, the improvement in VAS (p<0.001) and FAAM (p<0.001) was significant only in the corticosteroid group. During the first month, VAS (p=0.35) and PPT (p=0.003) were still better in the corticosteroid group. However, FAAM revealed no remarkable difference between the two groups (p=0.083). Eventually, at the third month of follow-up, there was no remarkable preference between the treatments regarding any of the outcome measures (p>0.05). Nevertheless, both methods efficiently improved patients’ symptoms, ie, over the 50% of pain reduction and 30% improvement in functional status.
Conclusion: The present results showed no remarkable superiority between the two groups. In other words, although ozone injection showed a slower efficacy than methylprednisolone, it could be used in plantar fasciitis management as an appropriate alternative.
Keywords: plantar fasciopathy, ozone, steroids, heel
Introduction
Plantar fascia, as a thick fibrous sheet, supports the longitudinal arch of the foot and acts as a powerful shock absorber.1,2 The inflammation of this fascia is called “plantar fasciitis” or more recently plantar fasciopathy, which is usually accompanied by heel spurs resulting from deposition of calcium with tension and inflammation of the attachment site to the calcaneus.3 Although the definite pathology is still unknown, some probable etiologies include repetitive microtrauma, degeneration, chronic inflammation, prominent heel spurs, entrapment of lateral plantar nerve, overuse, and seronegative arthritis-induced inflammation. It is primarily diagnosed based on symptoms of worsening pain upon morning arising and after long periods of sitting, plus signs of point tenderness in the origin of the fascia and increased pain with passive stretching of the plantar fascia.4–13
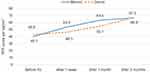 |
Figure 3 Therapeutic trajectory based on PPT changes within the two groups. |
Plantar fasciopathy is the most common cause of heel pain,14 with a 7–10% lifetime incidence.15 Despite being self-limiting, its spontaneous resolution takes quite a long time and it significantly affects health-related quality of life.16 There are several common first-line treatments for this condition, including NSAIDs, night splinting, and therapeutic exercise. Some less common non-invasive methods such as extracorporeal shock wave therapyand platelet-rich plasma (PRP) injection have also been utilized which lack sufficient evidence for routine use.17,18 Injection of corticosteroid is also a popular treatment.19,20 It should be noted that although corticosteroid injection can induce a remarkable symptom relief in plantar fasciopathy, might result in a number of complications, including rupture in plantar fascia or local fat-pad atrophy.21
A more recent therapeutic option is ozone injection which is now available as a solution of O2–O3. Its precise mechanism is not well understood. However, it may contribute to reduction of inflammation and pain, namely by downregulation of tumor necrosis factor α and TNFR2, and blocking phosphodiesterase-A2.22–27 It has previously been proven to be effective in the management of knee osteoarthritis, myofascial pain syndrome (MPS), and several other conditions.28–30 To the best of our knowledge,31–35 except for one article,31 there are no prospective studies comparing the efficacy of local steroid injection with ozone for the treatment of plantar fasciopathy. Therefore, in this trial we aimed to compare the efficacy and safety of these two injections added to standard conservative treatments available for plantar fasciopathy.
Materials and methods
Participants
This double-blinded randomized controlled trial (RCT) was conducted in physical medicine and rehabilitation clinic of Shahid Modarres and Shohaday-e-Tajrish Hospitals in 2017. The study sample consisted of 44 patients aged 20–65 years with at least 3 months of symptoms that was nonresponsive to first-line conservative therapies, such as foot orthoses, stretching exercises, and oral analgesics. The exclusion criteria were as follows: 1) pregnancy; 2) recent use of oral corticosteroids in the previous 2 weeks, or steroid injection in the site of plantar fascia within 6 months prior to the study; 3) vasovagal syncope, or hemodynamic instability; 4) recent skin or soft tissue infection at the site of injection; 5) neuropathy or radiculopathy associated with heel pain; 6) history of diabetes mellitus; 7) fracture of the surrounding bones; 8) secondary causes of heel pain such as ankylosing spondylitis, other inflammatory joint diseases, or surgery on plantar fascia; 9) glucose-6-phosphate dehydrogenase (G6PD) deficiency; and 10) use of angiotensin-converting enzyme inhibitors. The latter two were the relative contradiction of ozone injection.
Study design
According to the Declaration of Helsinki issued by the World Medical Association, investigators received ethics approval from Ethics Committee of Shahid Beheshti University of Medical Sciences (No. IR.SBMU.SM.REC.1395.384). After obtaining a written informed consent, the complete history was taken from each of the participants and full physical examination was performed. Demographic data including age, sex, height, weight, job difficulty level, level of education, and pain chronicity were recorded. Subsequently, patients were randomly divided into two parallel groups using a computer-based software of random number generation. In addition to injection, patients in both groups commonly received usual treatments including foot orthoses, ice massage, and stretching exercises for gastrosoleus muscles. One group of patients received a mixture of 1 mL corticosteroid (40 mg methylprednisolone) and 1 mL 2% lidocaine, while the other group received a mixture of 3 mL ozone gas (15 µg/mL) (generated using a Ozonibaric P® machine; Sedecal, Spain) mixed with 1 mL of lidocaine 2%. Injections were done in the maximal point of tenderness by a senior physiatrist with 15 years of experience in musculoskeletal injections (the second author, SA. R). Patients, as well as the physicians responsible for performing injections and assessments, were totally blinded to the groups. In other words, the syringes of administered mixture were placed in concealed envelopes by a nurse.
Severity of pain, the impact of pain on patients’ function, and pressure-pain threshold (PPT) were measured before the injection and after 1, 4, and 12 weeks by means of VAS , Foot and Ankle Ability Measure (FAAM) questionnaire, and an analog algometer (SM100 Sundoo®), respectively. VAS is a visual graphic-rating scale of 0–10 in which 0 indicates no pain and 10 shows the worst pain ever experienced. FAAM questionnaire is a self-report outcome instrument to assess physical function consisting of 29 items. Each item is scored on a 5-point Likert scale (4 to 0) from “4= no difficulty at all” to “0= unable to do”. Maximum possible score is 116 and the results have been reported in percent. PPT is defined as the minimum force applied which induces pain. The algometer was perpendicularly pressed against the skin with a an increment rate of 1 kg/cm2 per second until pain was elicited. Measurement was done three times with 30-s intervals in the same location and the average value was recorded. Oral tablets of acetaminophen were prescribed for all patients. Besides, the number of tablets used during 3 months was recorded.
Data analysis
Statistical analysis of data was performed using SPSS software version 22 (SPSS Inc., Chicago, IL, USA). Chi-square method was used to analyze and compare categorical data between the two groups. Also, Student’s t-test (independent samples t-test) was used for comparing continuous variables between the groups, initially and after each follow-up visit. Lastly, evaluation of post-treatment improvement in comparison to baseline level of variables was done using paired-samples t-test and repeated measure design across the follow-up time-points. The two-tailed p-value l<0.05 was considered significant.
Results
Seventy four patients initially enrolled, among them 50 participants were included in the study. Subjects were randomly divided (using a computer software for random-number generation) into two parallel groups of corticosteroid and ozone injection (25 in each group). However, two patients in the corticosteroid group and four in the ozone group discontinued the study (Figure 1). Two of them decided to receive dextrose prolotherapy, another three subjects failed to participate in the follow-up visits, and one subject asked to receive corticosteroid injection while randomly assigned to the ozone group. Therefore, these six patients received treatment but were excluded from the study. However, none of them exited because of a direct adverse event or other related complications; they were just unsatisfied with the treatment outcome. As a result, collected data from 44 patients including 23 participants in the corticosteroid group and 21 ones in the ozone group were finally analyzed.
 |
Figure 1 Flowchart of the study population. |
The majority of participants, ie, 29 patients (65.9%) were women and 15 subjects (34.1%) were men with a mean age of 47±9.0 years (28–68 years). With regard to job difficulty level, 16 patients (36.4%) had easy jobs (accountant, seller, clerk, manager, etc.); 20 ones (45.4%) had moderate jobs (teacher, police officer, driver, guard, housewife, etc.); and 8 subjects (18.2%) had difficult jobs (miner, barber, laborer, athletic, etc.). The average body mass index (BMI) calculated as weight/(height)2 was 28.6±3.2 kg/m2 (21.6–36.1 kg/m2). Mean duration of pain was 10.0±6.4 months (3–36 months). There was no significant difference between the groups regarding their demographic data, including age, sex, height, weight, BMI, job difficulty, level of education, pain duration, and the number of acetaminophen tablets used within 3 months (Table 1). Thus, the study population had homogeneously been distributed in the groups.
 |
Table 1 Demographic data as compared between the two groups |
The therapeutic trajectory (within-groups changes) for VAS, PPT, and FAAM scores at the four time-points (before injection, 1, 4, and 12 weeks after treatment) have been demonstrated in Table 2. Also, the inter-group comparisons (Table 3) revealed that VAS was relatively similar before treatment (p=0.841); while at the first week and month of follow-up period, it was significantly lower (p<0.001, and p=0.035, respectively) in the corticosteroid group, compared to the ozone group. In fact, VAS improvement, according to mean difference (MD) during the first week, was remarkably better following corticosteroid injection (MD=−3.0), compared to ozone injection (MD=0.3) (p<0.001). Similarly, VAS changes during the first month were slightly higher in the corticosteroid group but the difference was not clinically important between the groups (MD=−3.9 for steroid and −3.0 for ozone groups; p=0.063). VAS improvement was approximately 58% in both groups during 3 months, without any significant difference (p=0.890). Figure 2 demonstrates the therapeutic trajectory at the four time-points, based on VAS improvement in the two groups.
 |
Table 2 Within-groups comparisons for VAS, PPT, and FAAM scores in four time-points |
 |
Table 3 Between-groups comparisons for VAS, PPT, and FAAM scores in four time-points |
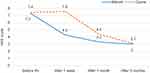 |
Figure 2 Therapeutic trajectory based on VAS changes within the two groups. |
In a similar pattern [Figure 3], PPT was not significantly different between groups before treatment (p=0.337). However, it was significantly higher in the corticosteroid group at both the first week and month after injection (p=0.019 and p=0.003, respectively). Again, at the end of the study, there was not any remarkable difference between groups with regard to their PPT (MD=26.5 [66%] and 24.5 [57%] for corticosteroid and ozone groups, respectively; p=0.848). Indeed, PPT changes during the first month after corticosteroid injection were significantly better than ozone injection (p<0.001). The therapeutic trajectory on PPT improvement at different time-points has been depicted within the two groups.
Scores of FAAM questionnaire were not significantly different between groups before treatment (p=0.393). However, FAAM scores were lower in the corticosteroid group 1 week and 1 month after treatment (p<0.001 and p=0.083, respectively). However, the difference between groups was statistically significant only after 1 week follow-up. Besides, there was no clinically important difference between the two groups in their total changes from the baseline at the first month visit (MD=−29.4 and −21.7 for corticosteroid and ozone groups, respectively; p-value=0.041). After 3 months, FAAM score changes were similar between groups (MD=−22.5 [34%] and −17.9 [28%], for corticosteroid and ozone groups, respectively; p=0.217). To summarize, Figure 4 has demonstrated FAAM score changes initially and at three follow-up time-points.
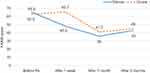 |
Figure 4 Therapeutic trajectory based on FAAM score changes within the two groups. |
Discussion
The results of this study showed that there was no significant difference between the two groups for VAS, PPT, and FAAM before treatment. However, 1 week after treatment, VAS (p<0.001), FAAM (p<0.001), and PPT (p=0.019) were significantly better in the corticosteroid group compared to the ozone group. One month after treatment, VAS (p=0.35) and PPT (p=0.003) were still better in the corticosteroid group. However, FAAM was not significantly different between the two groups (p=0.083). Eventually, there was no significant difference between groups concerning any of VAS, PPT, or FAAM scores at the third month of follow-up (p>0.05).
Few studies have been conducted on the efficacy of ozone injection in chronic inflammatory diseases, and there has been only one previous study,31 comparing the effects of local ozone injection versus the corticosteroids for plantar fasciopathy. Therefore, we have firstly compared our results with earlier studies on other treatment methods. McMillan et al evaluated the efficacy of ultrasoundguided injection of 1 mL corticosteroid (dexamethasone sodium phosphate with dosage 4 mg/mL) versus 1 mL normal saline (placebo), among plantar fasciopathy sufferers. They used the foot health status questionnaire for pain measurement at 4, 8, and 12 weeks.32 Similar to our study short-term (at 4 weeks) efficacy of corticosteroid was confirmed, and pain scores were not significantly different between groups after 12 weeks (3 months). However, pain questionnaires, type of corticosteroid, and follow-up intervals utilized in their study were relatively different.
In another study, Karimzadeh et al assessed local injection of autologous whole blood with corticosteroid in the treatment of plantar fasciopathy.33 The results were somewhat similar to the present study. The mean value of pain severity (measured by VAS) and average level of PPT in both groups significantly improved during 1 and 3 months after injection. However, the difference between study groups was not statistically significant.
Mahindra et al compared the effect of PRP versus corticosteroid and placebo in the treatment of chronic plantar fasciopathy.35 In this study, local injection of PRP was more, or at least as effective as corticosteroid. Both methods were significantly more effective than placebo. Similar to the corticosteroid group of our study, VAS score significantly decreased 3 weeks and 3 months after corticosteroid injection. Functional improvement was also observed with corticosteroid. However, a different functional questionnaire (AOFAS; The American Orthopedic Foot and Ankle Score) was used in their study. While treatment of plantar fasciopathy with ozone has not been studied, some research has been done to evaluate the effect of ozone injection in other musculoskeletal conditions. For instance, ozone has been proved to be effective in pain relief, local inflammation, and systemic inflammation in patients with disc herniation or knee osteoarthritis.28,36 In another study performed by Morelli et al it was shown that results of ozone therapy were significantly better than diathermy in the treatment of chronic low back pain.37 Additionally, the positive effect of ozone therapy on carpal tunnel syndrome, refractory headaches, and MPS has been confirmed.38,39 A very similar RCT by Babaei-Ghazani et al evaluated two groups of plantar fasciopathy patients with 15 subjects in each group. Participants received either of ozone or corticosteroid injection and were followed during a 3-month period. Finally, authors concluded that both methods were effective in the treatment of chronic fasciopathy patients. They also achieved the same result that steroid injection provided a more rapid and short-term therapeutic effect. On the other hand, they concluded that ozone (O2–O3) injection could be a beneficial option with slow onset and a longer durability.31 Among their findings, the latter was not supported by the present data. In fact, there was no remarkable difference between ozone and corticosteroid injection durability for any of the outcome measuring tools. In the current investigation, both methods efficiently improved patients' symptoms; ie, over the 50% of pain reduction and approximately 30% improvement in functional status, without any remarkable superiority between groups.
Limitations
The first drawback in this research was the absence of a real control group; it would better to recruit a larger sample and assign them into three groups. In addition to the two mentioned groups, we could consider another category receiving only the conservative treatments without any injection. Such a three-arm design could efficiently compare the actual effect size of ozone and corticosteroid injections. As the other limitation, loss to follow-up rate was relatively remarkable (6 patients; 12%) and could potentially result in attrition bias. However, intention to treat analysis was done that revealed no significant difference between the therapeutic trajectory of those participants who discontinued the study with the rest of population at 1 week and 1 month follow-up. In fact, none of them exited because of a direct adverse event or other related complications; they were just unsatisfied with the treatment outcome.
Conclusion
Our results proved that both groups significantly improved regarding their pain and level of function and PPT. The therapeutic efficacy in corticosteroid effects was more rapid compared to the ozone injection. The results were associated with a better short-term outcome in the corticosteroid group compared to the ozone category (at 1 week and 1 month follow-up), when added to a standard conservative treatment. However, the final outcomes were relatively similar at the third month. Therefore, local injection of ozone, plus the conventional treatments seems to be an appropriate alternative to traditional corticosteroids in plantar fasciopathy management.
Acknowledgments
This article has been extracted from the thesis written by Dr Mahboobeh Barchinejad in School of Medicine, Shahid Beheshti University of Medical Sciences (Registration No: 274). We gratefully acknowledge the dedicated efforts of the investigators, the coordinators, the volunteer patients who participated in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Karabay N, Toros T, Hurel C. Ultrasonographic evaluation in plantar fasciitis. J Foot Ankle Surg. 2007;46(6):442–446.
2. Roxas M. Plantar fasciitis: diagnosis and therapeutic considerations. Alt Med Rev. 2005;10(2):83–93.
3. Cornwall MW, McPoil TG. Plantar fasciitis: etiology and treatment. J Orthop Sports Phys Ther. 1999;29(12):756–760. doi:10.2519/jospt.1999.29.12.756
4. Davis PF, Severud E, Baxter DE. Painful heel syndrome: results of nonoperative treatment. Foot Ankle Int. 1994;15(10):531–535. doi:10.1177/107110079401501002
5. Aldridge T. Diagnosing heel pain in adults. Am Family Physician. 2004;15(70):332–342.
6. Buchbinder R, Ptasznik R, Gordon J, Buchanan J, Prabaharan V, Forbes A. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. Jama. 2002;288(11):1364–1372. doi:10.1001/jama.288.11.1364
7. May TJ, Judy TA, Conti M, et al. Current treatment of plantar fasciitis. Curr Sports Med Rep. 2002;1(5):278–284. doi:10.1249/00149619-200210000-00005
8. Ogden JA. Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. Br J Sports Med. 2004;38(4):382. doi:10.1136/bjsm.2004.011601
9. Speed CA, Nichols D, Wies J, et al. Extracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trial. J Orthop Res. 2003;21(5):937–940. doi:10.1016/S0736-0266(03)00048-2
10. Theodore GH, Buch M, Amendola A, Bachmann C, Fleming LL, Zingas C. Extracorporeal shock wave therapy for the treatment of plantar fasciitis. Foot Ankle Int. 2004;25(5):290–297. doi:10.1177/107110070402500503
11. Wang CJ. An overview of shock wave therapy in musculoskeletal disorders. Chang Gung Med J. 2003;26(4):220–232.
12. Williams SK, Brage M. Heel pain-plantar fasciitis and Achilles enthesopathy. Clin Sports Med. 2004;23(1):123–144. doi:10.1016/S0278-5919(03)00094-2
13. Wang CJ, Chen HS, Huang TW. Shockwave therapy for patients with plantar fasciitis: a one-year follow-up study. Foot Ankle Int. 2002;23(3):204–207. doi:10.1177/107110070202300303
14. Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25(5):303–310. doi:10.1177/107110070402500505
15. Dunn JE, Link CL, Felson DT, Crincoli MG, Keysor JJ, McKinlay JB. Prevalence of foot and ankle conditions in a multiethnic community sample of older adults. Am J Epidemiol. 2004;159(5):491–498.
16. Irving DB, Cook JL, Young MA, Menz HB. Impact of chronic plantar heel pain on health-related quality of life. J Am Podiatr Med Assoc. 2008;98(4):283–289. doi:10.7547/0980283
17. Gollwitzer H, Saxena A, DiDomenico LA, et al. Clinically relevant effectiveness of focused extracorporeal shock wave therapy in the treatment of chronic plantar fasciitis: a randomized, controlled multicenter study. JBJS. 2015;97(9):701–708. doi:10.2106/JBJS.M.01331
18. Monto RR. Platelet-rich plasma efficacy versus corticosteroid injection treatment for chronic severe plantar fasciitis. Foot Ankle Int. 2014;35(4):313–318. doi:10.1177/1071100713519778
19. Landorf KB. Plantar heel pain and plantar fasciitis. BMJ Clin Evidence. 2015;2015:1111.
20. Pribut SM. Current approaches to the management of plantar heel pain syndrome, including the role of injectable corticosteroids. J Am Podiatr Med Assoc. 2007;97(1):68–74.
21. Tatli YZ, Kapasi S. The real risks of steroid injection for plantar fasciitis, with a review of conservative therapies. Curr Rev Musculoskelet Med. 2009;2(1):3–9. doi:10.1007/s12178-008-9036-1
22. Bocci VA. Scientific and medical aspects of ozone therapy. State of the art. Arch Med Res. 2006;37(4):425–435.
23. Mishra SK, Pramanik R, Das P, et al. Role of intra-articular ozone in osteo-arthritis of knee for functional and symptomatic improvement. Ind J Phys Med Rehabil. 2011;22(2):65–69.
24. Al-Jaziri AA, Mahmoodi SM. Painkilling effect of ozone-oxygen injection on spine and joint osteoarthritis. Saudi Med J. 2008;29(4):553–557.
25. Manoto SL, Maepa MJ, Motaung SK. Medical ozone therapy as a potential treatment modality for regeneration of damaged articular cartilage in osteoarthritis. Saudi J Biol Sci. 2018;25(4):672–679.
26. Chen H, Yu B, Lu C, Lin Q. The effect of intra-articular injection of different concentrations of ozone on the level of TNF-α, TNF-R1, and TNF-R2 in rats with rheumatoid arthritis. Rheumatol Int. 2013;33(5):1223–1227.
27. Giombini A, Menotti F, Di AC, et al. Comparison between intrarticular injection of hyaluronic acid, oxygen ozone, and the combination of both in the treatment of knee osteoarthrosis. J Biol Reg Homeost Agents. 2016;30(2):621–625.
28. Raeissadat SA, Tabibian E, Rayegani SM, Rahimi-Dehgolan S, Babaei-Ghazani A. An investigation into the efficacy of intra-articular ozone (O2–O3) injection in patients with knee osteoarthritis: a systematic review and meta-analysis. J Pain Res. 2018;11:2537. doi:10.2147/JPR.S175441
29. Raeissadat SA, Rayegani SM, Forogh B, Abadi PH, Moridnia M, Rahimi-Dehgolan S. Intra-articular ozone or hyaluronic acid injection: which one is superior in patients with knee osteoarthritis? A 6-month randomized clinical trial. J Pain Res. 2018;11:111. doi:10.2147/JPR.S142755
30. Raeissadat SA, Rayegani SM, Sadeghi F, Rahimi-Dehgolan S. Comparison of ozone and lidocaine injection efficacy vs dry needling in myofascial pain syndrome patients. J Pain Res. 2018;11:1273. doi:10.2147/JPR.S164629
31. Babaei-Ghazani A, Karimi N, Forogh B, et al. Comparison of ultrasound-guided local ozone (O2-O3) injection vs corticosteroid injection in the treatment of chronic plantar fasciitis: a randomized clinical trial. Pain Med. 2018. doi:10.1093/pm/pny066.
32. McMillan AM, Landorf KB, Gilheany MF, Bird AR, Morrow AD, Menz HB. Ultrasound guided corticosteroid injection for plantar fasciitis: randomised controlled trial. BMj. 2012;22(344):e3260. doi:10.1136/bmj.e3260
33. Karimzadeh A, Raeissadat SA, Erfani Fam S, Sedighipour L, Babaei-Ghazani A. Autologous whole blood versus corticosteroid local injection in treatment of plantar fasciitis: a randomized, controlled multicenter clinical trial. Clin Rheumatol. 2017;36(3):661–669. doi:10.1007/s10067-016-3484-6.
34. Vahdatpour B, Kianimehr L, Ahrar MH. Autologous platelet-rich plasma compared with whole blood for the treatment of chronic plantar fasciitis; a comparative clinical trial. Adv Biomed Res. 2016;5:84. Published 2016 May 11. doi:10.4103/2277-9175.182215.
35. Mahindra P, Yamin M, Selhi HS, Singla S, Soni A. Chronic plantar fasciitis: effect of platelet-rich plasma, corticosteroid, and placebo. Orthopedics. 2016;39(2):e285–289. doi:10.3928/01477447-20160222-01
36. Borrelli E, Alexandre A, Iliakis E, Alexandre A, Bocci V. Disc herniation and knee arthritis as chronic oxidative stress diseases: the therapeutic role of oxygen ozone therapy. J Arthritis. 2015;4(3):161.
37. Morelli L, Bramani SC, Cantaluppi M, Pauletto M, Scuotto A. Comparison among different therapeutic techniques to treat low back pain: a monitored randomized study. Ozone Ther. 2016;1(1):17–20. doi:10.4081/ozone.2016.5842
38. Clavo B, Santana-Rodriguez N, Gutierrez D, et al. Long-term improvement in refractory headache following ozone therapy. J Alt Compl Med. 2013;19(5):453–458.
39. Bahrami MH, Raeissadat SA, Nezamabadi M, Hojjati F, Rahimi-Dehgolan S. Interesting effectiveness of ozone injection for carpal tunnel syndrome treatment: a randomized controlled trial. Orthop Res Rev. 2019;11:61–67. Published 2019 May 6. doi:10.2147/ORR.S2027809.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
