Back to Journals » Vascular Health and Risk Management » Volume 11
Lipid-modifying therapy in the elderly
Authors Hamilton-Craig I, Colquhoun D, Kostner K, Woodhouse S, d'Emden M
Received 11 September 2014
Accepted for publication 17 October 2014
Published 14 May 2015 Volume 2015:11 Pages 251—263
DOI https://doi.org/10.2147/VHRM.S40474
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Daniel Duprez
Ian Hamilton-Craig,1,2 David Colquhoun,3,4 Karam Kostner,4,5 Stan Woodhouse,4,6 Michael d'Emden4,7
1Griffith University School of Medicine, Griffith Health Institute, Gold Coast, QLD, Australia; 2Flinders University School of Medicine, Adelaide, SA, Australia, 3Wesley Medical Centre, Auchenflower, QLD, Australia; 4University of Queensland, Brisbane, QLD, Australia; 5Department of Cardiology, Mater Hospital, Woolloongabba, QLD, Australia; 6Taylor Medical Centre, Woolloongabba, QLD, Australia; 7Department of Endocrinology, Royal Brisbane Hospital, Herston, QLD, Australia
Abstract: Cardiovascular disease (CVD) mortality and morbidity increases with increasing age, largely as a result of increased lifetime exposure as well as increased prevalence of CVD risk factors. Hospitalization for CVD increases by a factor of over 18× for those aged 85+ years versus those aged <30 years. In spite of this, life expectancy continues to increase, and in Australia for people reaching the age of 65 years, it is now 84 years in men and 87 years in women. The number of people for whom lipid management is potentially indicated therefore increases with aging. This is especially the case for secondary prevention and for people aged 65–75 years for whom there is also evidence of benefit from primary prevention. Many people in this age group are not treated with lipid-lowering drugs, however. Even those with CVD may be suboptimally treated, with one study showing treatment rates to fall from ~60% in those aged <50 years to <15% for those aged 85+ years. Treatment of the most elderly patient groups remains controversial partly from the lack of randomized trial intervention data and partly from the potential for adverse effects of lipid therapy. There are many complex issues involved in the decision to introduce effective lipid-lowering therapy and, unfortunately, in many instances there is not adequate data to make evidence-based decisions regarding management. This review summarizes the current state of knowledge of the management of lipid disorders in the elderly and proposes guidelines for management.
Keywords: lipid management, elderly, statins
Introduction
The average life expectancy of people in Western cultures has increased significantly over the last 50 years with the average age of death for a person reaching the age of 65 now being 85 years for men and 87 years for women. Persons living past the age of 65 (the elderly) can now expect to live for nearly a further 19–22 years. Importantly, cardiovascular disease (CVD) accounts for >75% of deaths in the elderly. Effective lipid management in the elderly should reduce the risk of developing CVD with improvement of quality of life and potentially a further increase in longevity. There are many complex issues involved in the decision to introduce effective lipid-lowering therapy, but, unfortunately, in many instances there is not adequate data to make evidence-based decisions regarding management. In this paper, we review the current state of knowledge of the management of lipid disorders in the elderly.
Current suboptimal management of the elderly
Management of hyperlipidemia in the elderly may be suboptimal for several reasons:
- The statistical relationship between blood cholesterol and CVD is less strong in the elderly compared to the middle-aged.1
- Physician uncertainty exists with regard to the benefits of lipid management.
- There are concerns about adverse drug reactions (ADRs) including increased risk of statin-associated myalgia and other statin-related ADRs.2,3
- CVD risk calculators are unreliable in elderly patients, in whom physicians may either underestimate or overestimate CVD risk.4
In view of these factors, the elderly are treated less frequently with lipid-lowering therapy. For example, Massing et al analyzed 56,320 medical records from 296 medical practices in the US, and showed that lipid medication rates in patients with coronary artery disease (CAD) declined with increasing age from ~60% in those aged 50 years to <15% in those aged ≥85 years.5 Dose titration of statins was inversely related to age; doses above the starting dose were given to 60% of patients aged 21–44 years and to 35% of patients aged ≥85 years. Rates of prescribing non-lipid medications were similar at all ages, however. Figure 1 shows the mean odds ratios (ORs) for treatment with lipid therapy according to age.5 The ratio declined with advancing age and was lowest in the age group >85 years.
  | Figure 1 Mean odds ratios for treatment with lipid therapy according to age. |
More recent studies have also shown significant lipid treatment gaps in primary care, as in the AusHEART study in middle-aged patients aged ≥55 years in which patients aged >75 years were excluded.6
Simons and Chung used records of the Pharmaceutical Benefits Scheme between 2006 and 2013 in 276,212 patients at high CVD risk and mean age 66 years. Of this group, 42% had not received lipid-lowering drugs during the study period.7 There was a U-shaped relationship with age, with the proportions not receiving drugs being highest in those aged <41 years and >81 years.7
We previously observed in a survey of general practice in Australia that about 50% of patients with severe hypercholesterolemia (total cholesterol [TC] >7.5 mmol/L) were not treated with lipid-lowering therapy.8 This proportion was similar for all age groups, and it appeared (at least for severe hypercholesterolemia) that physician inertia may not only be confined to the elderly but may apply to other age groups as well.8
Appropriateness of therapy
Holmes et al have proposed a process for medication prescribing in patients late in life that builds on the principles of appropriate prescribing and includes consideration of the remaining life expectancy, goals of care, quality of life, and potential benefits of medications (Table 1).9
  | Table 1 The Medication Appropriateness Index9 |
In their model, four steps in medication decision making form a pyramid, visually representing the appropriate medications at any level. The model identifies patients for whom statin therapy is the least appropriate (limited life expectancy, palliative goals of care, treatment targets focused on symptom management) versus patients most appropriate for statin therapy (longer life expectancy, longer time until benefit, more aggressive goals of care focused on preventive strategies).9
Life expectancy
Life expectancy in most countries including Australia is increasing progressively. For those aged 65 years, life expectancy is a further 19 years and 22 years – to 84 years in men and 87 years in women.10 For men and women aged 85 years, further life expectancy is 5.9 years and 7.1 years, respectively.11
There are, however, no reliable tools for predicting life expectancy in elderly Australians, other than through extrapolation of parameters known to affect survival such as CVD risk factors, family history, and other intuitive variables. Attempts to develop prognostic indices in older adults have met with varied success, and few indices have been independently validated.4 Use of the Lloyd-Jones algorithm for predicting CVD risk up to age 80 years is recommended by the International Atherosclerosis Society (IAS).12
Recent reviews have suggested the need for contemporary and comprehensive health care guidelines in the elderly.13,14 In this paper, we review the evidence for lipid therapy in the elderly and propose guidelines for therapy.
Cardiovascular risk in the elderly
Epidemiological studies have consistently shown that CVD risk increases with age in both sexes, and that increasing age is one of the most powerful factors predicting CVD risk. CVD in older patients is also associated with worse outcomes.
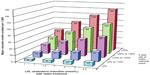
Figure 2 shows the CVD risk in the Australian population according to age and sex.15 Those aged 75 years or more have several-fold higher rates of CVD than those aged <50 years, the relationship between age and CVD risk being semiexponential.
  | Figure 2 Hospitalizations for CVD per 100,000 people in the Australian population according to age and sex. |
CVD risk factors in the elderly
With increasing age, the burden of CVD risk factors (other than cigarette smoking, TC, and body mass index [BMI]) increases progressively, as shown in Table 2.16
  | Table 2 Prevalence of CVD risk factors (%) by age and sex in the Framingham Study16 |
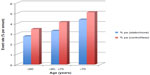
In the elderly, gradients in CVD risk depend on the number of risk factors present, as in younger age groups. Data from the Dubbo study are shown in Figure 3.1
The Prospective Studies Collaboration showed that the strength of the relationship between usual cholesterol levels and vascular mortality was inversely related to age (Figure 4).17
  | Figure 4 Vascular mortality according to age and total cholesterol level in the Prospective Studies Collaboration. |
These data show a much steeper gradient between the hazard ratio (HR) for vascular mortality in younger compared to older patients.
In Figure 4, the HR increased from ~0.8 (with TC 4.5 mmol/L) to ~12 (with TC 8.0 mmol/L) in patients aged 40–49 years, while in patients aged 80–89 years the HR rose from ~128 to 256 for the same TC levels.
Figure 4 also suggests that lowering cholesterol in younger patients will result in greater relative risk reduction (RRR, by a factor of ~15) compared to the oldest group (by a factor of ~2). Absolute risk reduction, however, is greater in older patients, with HR falling by ~128 in patients in the oldest age group and by ~11 in the youngest.
The “elderly paradox” is based on epidemiological studies and refers to the absolute benefit being greater in the elderly even though the risk attributable to cholesterol is much less. The number of patients needed to be treated to prevent a coronary event is therefore less in the elderly due to a higher absolute risk. There is potentially greater harm from drug therapy in the elderly and potentially less benefit due to other illnesses that impact on the quality of life and survival. Obviously, the very elderly have reduced life expectancy compared to middle-aged patients. As a result of these general considerations, the elderly may be denied lipid treatments that could have a significant positive effect on morbidity and the associated quality of life.
Measurement of lipids in the elderly
The proportion of private lipoprotein tests in Queensland in 1 year increases linearly with increasing age (Figure 5).8 The lowest proportion of lipoprotein tests occurs under age 25 years (~12%), compared with ~50% for age 45–54 years, >80% for age 65–74 years, and 92% for age >74 years. Measurement of lipids would not seem to be a limiting step to treatment in older patients.
  | Figure 5 Proportion of private lipoprotein tests in Queensland in 1 year according to age. |
Estimating CVD risk in the elderly
The IAS recently recommended use of lifetime (long-term) risk prediction from age 50 years to 80 years for clinical intervention on low-density lipoprotein cholesterol (LDL-C) and atherogenic lipoproteins (Table 3).18 The exclusion of patients older than 80 years reflects the lack of data in this age group.
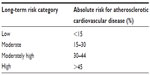  | Table 3 Long-term risk for atherosclerotic cardiovascular disease by age 80 (from age 50) |
For primary prevention, risk to age 80 for atherosclerotic CVD can be stratified into high (>45%), moderately high (30%–44%), moderate (15%–30%), and low (<15%) (Table 3).
According to the IAS, QRISK (a prediction algorithm for CVD) appears to be reliable for Western Europe and is ethnicity specific (for the UK).19 For world populations, the IAS recommends the Lloyd-Jones/Framingham algorithm for estimating absolute risk for total atherosclerotic CVD to age 80.20 Calculated risk can be recalibrated based on the coefficients determined by national comparisons with Framingham estimates. If recalibration values were unavailable, treatment can be focused on individual risk factors.
Coronary calcium score
In the elderly, risk profiling using variations of the Framingham equations overestimate risk due to the weighting of age in the calculation. Many clinicians do not use risk calculators and believe that the impression of risk is as accurate, and to some extent this is correct.21
Coronary calcium scoring has emerged as an independent predictor of CAD and it may be more useful in the elderly in terms of predicting risk. Recently, a review of coronary calcium scoring in asymptomatic individuals assessing mortality in patients older than 75 years has been published.22 A zero coronary artery calcium (CAC) score is associated with a 5.6-year survival of 98%, similar to those in other groups with a cardiac calcium score of zero, which is approximately 99%. The study followed up 44,052 asymptomatic individuals in North America. The increasing CAC independently predicted an increased risk of all-cause mortality in all age groups. In the >75 age group, a CAC of >400 was associated with 16× greater mortality than a CAC equaling zero. In this study, CAC also predicted all-cause mortality in those aged <45 years. As this test is such a powerful predictor, many patients who would otherwise not be on therapy would be commenced on therapy to lower the CVD risk, and a significant number of elderly would not need to go on to drug therapy.
Lipid management in the elderly: evidence for benefit from statin trials
Roberts et al showed reduced total mortality (15% reduction), coronary heart disease (CHD) mortality (23% reduction), fatal or nonfatal stroke (24% reduction), and fatal or nonfatal myocardial infarction (MI) (26% reduction) in a meta-analysis of over 50,000 patients aged >60 years treated with statins (Figure 6).23 They concluded, “statin therapy should be offered to older patients at high risk”, and “statin treatment is associated with clearly reduced mortality risk of cardiovascular patients aged 75 years or older”.
  | Figure 6 Meta-analysis of patients with cardiovascular disease aged >60 years according to statin versus placebo treatment. |
Figure 7 shows the number of major CVD events avoided with statin therapy for all age groups, according to baseline 5-year risk of a CVD event in the meta-analysis of the Cholesterol Treatment Trialists’ Collaboration (CTTC).24
  | Figure 7 Predicted 5-year benefits of LDL cholesterol reductions with statin treatment at different levels of risk in Cholesterol Treatment Trialists’ Collaboration meta-analysis. |
Figure 8 shows the effects on major vascular events per 1.0 mmol/L reduction in LDL-C at different levels of risk, by baseline age, according to the CTTC meta-analysis.24 The event rate increased with increasing age from ≤60 years to >70 years, while the RRR was of a similar order of magnitude for all age groups.24 For every mmol/L reduction in LDL-C achieved with statin treatment, the relative risk reductions in major vascular events for the age groups <=60 years, >60 to <=70 years and >70 years were 0.77, 0.78 and 0.83, respectively (all P<0.001).
  | Figure 8 Major vascular event rate with statin treatment according to age in Cholesterol Treatment Trialists’ Collaboration meta-analysis. |
The CTTC data strongly support use of statins in the elderly for CVD risk reduction.24
One trial (PROSPER) was designed to test the benefits of statin therapy specifically in the elderly.25 In 5,804 men and women aged 70–82 years (2,520 Scottish subjects), a significant benefit occurred with pravastatin therapy compared with placebo. There was 19% reduction in coronary events after a mean of 3.2 years (P=0.006), with no impact on stroke or total mortality and a suggestion of increased cancer risk.25 The recently published long-term follow-up of the PROSPER study over 8.6 years showed 20% reduction in coronary events with no effect on cancer, stroke, or total mortality.25 It was suggested that the lack of benefit for survival possibly reflected competing mortality from other causes.
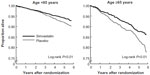
Figure 9 shows the reduction in coronary death or hospitalization for MI with pravastatin therapy in the Scottish cohort of the PROSPER study.25
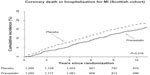  | Figure 9 Reduction in coronary death or hospitalization for myocardial infarction with pravastatin versus placebo treatment. |
Other data showing benefit from statin therapy in elderly patients are shown in Figures 10 and 11.26,27 Allen Maycock et al showed that statin therapy was associated with reduced mortality across all age groups of individuals with significant coronary disease, including very elderly patients (Figure 10).26
  | Figure 10 Mortality reduction in cardiovascular disease patients with statin treatment according to age. |
  | Figure 11 Benefits of simvastatin versus placebo treatment in Scandinavian Simvastatin Survival Study. |
Miettinen et al investigated the benefits of simvastatin therapy compared with placebo in elderly subjects with CHD of the Scandinavian Simvastatin (4S) Study (Figure 11).27 The cohort of 4,444 subjects included 1,021 patients aged ≥65 years, with 5.4 mean years of follow-up. In the elderly cohort, there were significantly lower rates of total mortality (34%), CHD mortality (43%), major CHD events (34%), and revascularizations (41%).
In the LIPID study of 9,014 subjects, 3,514 were aged 65–75 years. Patients had previous MI or unstable angina and were treated with pravastatin or placebo for 6 years.28 Similar RRR was observed with pravastatin therapy for older (65–75 years) and younger (<65 years) age groups. For every 1,000 older patients treated, pravastatin prevented 45 deaths, 33 MIs, 32 unstable angina events, 34 revascularizations, 13 strokes, and 133 major CVD events compared with 22 deaths and 107 major CVD events in younger patients.28 It was concluded that the absolute benefit of treatment is significantly greater in older patients with previous CHD because they are at greater risk.
In a substudy of the Cholesterol and Recurrent Events (CARE) trial, Lewis et al investigated the effect of pravastatin on cardiovascular events in older patients aged ≥65 years with previous MI and cholesterol levels <6.2 mmol/L (240 mg/dL) and LDL-C levels 3.0–4.5 mmol/L (115–174 mg/dL).29 Over 5 years in 1,283 subjects, pravastatin therapy compared with placebo reduced CHD and stroke by 32% and 40% (P<0.001 and P=0.03), respectively. For every 1,000 patients treated, pravastatin prevented 225 hospitalizations in older patients compared to 121 in younger patients.29
Adherence in the elderly
Adherence is the key to obtaining benefit of proven drug therapy. Age is a factor, and within the elderly age bracket, probably the “very old” have even poorer long-term persistence with therapy. Webster packs and similar aids by pharmacies have been shown to improve adherence.
In a recent study of 259 patients discharged after an acute MI, persistence was assessed.30 At discharge, 99.2% were prescribed antiplatelets, 86.5% betablockers, 95% statins, and 90.4% angiotensin-converting enzyme (ACE) inhibitors. Persistence at 1 year post discharge was worse in those >75 years, dropping from 74.1% for the combination of all drug classes to 37.8%.30
Triglycerides in the elderly
In a study of triglycerides (TGs) as risk factors for CHD, the adjusted ORs of association were 1.57 (95% CI, 1.10–2.24) and 1.76 (CI, 1.39–2.21) for the EPIC-Norfolk and Reykjavik studies, respectively, in which the mean ages were 74 years and 70 years, respectively.31 Meta-analyses of these and other studies confirm that TGs are independent risk factors for CVD.31,32 Risk of CHD increases with fasting TGs above 1.7 mmol/L (~150 mg/dL). About one-third of adults have TGs in this range.33
No randomized trials of therapy with fibrates have been shown to benefit patients with elevated TG and low high-density lipoprotein cholesterol (HDL-C) in elderly subjects. However, recent meta-analyses of the five prospective, randomized, placebo-controlled trials demonstrate robust and consistent benefit for reducing CHD events in patients with fasting TCs >2.3 mmol/L (≈200 mg/dL), OR =0.65 (0.54–0.78 [95% CI]).34
The European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) Guidelines recommend use of drugs to lower triglycerides if after lifestyle measures fasting triglycerides are >2.3 mmol/L (≈200 mg/dL).35 Treatment is meant to be for patients deemed at “high total CV risk”. High total CV risk is defined as either markedly elevated single risk factors such as familial dyslipidemia and severe hypertension, or a calculated SCORE ≥5% and <10% for a 10-year risk of fatal CVD.35 When fasting TGs are very high >10 mmol/L (≈500 mg/dL), risk of pancreatitis is clinically significant. The ESC/EAS guidelines note “actions to prevent acute pancreatitis are mandatory”. Actions are to restrict fat (10%–15% of total daily energy intake), abstinence of alcohol, fibrate therapy (fenofibrate), and n-3 fatty acids (2–4 g/day of eicosapentaenoic acid [EPA] and docosahexaenoic [DHA]) or nicotinic acid. ESC/EAS recommendations for drug treatment of elevated TGs are Class I/Level B for fibrates, Class IIa/Level B for n-3 fatty acids, Class IIa/Level C for statin and fibrate, and Class IIb/Level B for fibrate and n-3 fatty acids.35
National and international guidelines for lipid management in the elderly
Several recent guidelines on lipid management include sections on the elderly. They show some differences in approach but are generally consistent with each other (Table 4).14
  | Table 4 Guidelines on lipid management in the elderly by different groups: summary |
American College of Cardiology/American Heart Association
The American College of Cardiology/American Heart Association (ACC/AHA) 2013 guideline recommends the use of Pooled Cohort Equations for the estimation of the 10-year risk in those 76–79 years old to help guide treatment decision making.36 Evidence from randomized clinical trials supports continuing statin therapy beyond 75 years of age in patients already taking and tolerating them. Moderate-intensity statin use was supported for secondary prevention, but, for primary prevention in this age group, comorbidities, safety, and priorities of care should all be considered. Before initiating statins for primary prevention, therefore, discussion of CVD reduction benefits, risk of ADR, drug–drug interactions, and patient preference is recommended.36
European Society of Cardiology/European Atherosclerosis Society
The ESC/EAS guidelines include a significant section on lipid management of the elderly.35 Summary statements were: “Risk reduction in individuals older than 65 years is essential because two-thirds to three-quarters of them have either clinical CAD or subclinical atherosclerotic disease. Almost 25% of men and 42% of women older than 65 years have a TC level >6 mmol/L”, and “According to published data, elderly individuals are a high risk group who could benefit significantly from lipid-lowering therapy to reduce CV morbidity and mortality. Evidence for treatment above the age of 80–85 years is very limited, and clinical judgment should guide decisions in the very old”.35
Primary prevention in the elderly was supported by the CTTC and other meta-analyses, in that RRR was similar in older and younger patients.
Because of the increased risk of drug ADR and drug–drug interactions, the ESC/EAS recommends that statins be started at low doses and then titrated to achieve optimal LDL-C levels.
Reduced compliance in the elderly was also discussed, which may result from perceived lack of benefit, drug ADR, cost, and CVD events occurring while on therapy. Improved explanation of benefits of treatment and treatment regimens may improve compliance.
Australian National Vascular Disease Prevention Alliance
The National Vascular Disease Prevention Alliance guidelines for the management of absolute risk in CVD 2012 recommends that patients with estimated 5-year CVD risk ≥15% require lipid-modifying therapy.37 For patients aged >74 years, who are not known to have CVD or to be at clinically determined high risk, “absolute risk over the next 5 years should be assessed using the Framingham Risk Equation Calculator using the age 74 years. Although this may underestimate the risk in this population, available evidence suggests that this approach will provide an estimate of minimum CVD risk”.37
For those aged >74 years, “The decision to initiate therapy should be based on clinical judgment which takes into account the likely benefits and risks of treatment, life expectancy, co-morbidities and quality of life, personal values”.37
Table 5 lists the ESC/EAS recommendations for treatment of dyslipidemia in the elderly.35
  | Table 5 ESC/EAS recommendations for treatment of dyslipidemia in the elderly |
National Institute for Clinical Excellence (UK)
The following statements were made in National Institute for Clinical Excellence (NICE) guidelines for lipid management in the elderly: “For the primary prevention of CVD in primary care, a systematic strategy should be used to identify people aged 40–74 who are likely to be at high risk”; “People aged 75 or older should be considered at increased risk of CVD, particularly people who smoke or have raised blood pressure. They are likely to benefit from statin treatment. Assessment and treatment should be guided by the benefits and risks of treatment, informed preference and comorbidities that may make treatment inappropriate”.38
International Atherosclerosis Society
The recent IAS guidelines include a comprehensive section on lipid management in the elderly.17 Estimation of lifetime risk was recommended, in which it is assumed that CV risk burden remains constant beyond age 50 years. Because CV risk factors actually increase with age (Table 2), this may underestimate lifetime risk nevertheless. Calibration of estimates was recommended according to the country of residence, eg, CVD risk is lower in southern Europe and Asia compared with Northern Europe.
The IAS guidelines recommend estimating hard CHD risk in patients aged >65 years using Framingham scoring, recalibrated for country (http://hp2010.nhlbihin.net/aptiii/calculator.asp?usertype=prof). Total CVD can be estimated by increasing the CHD risk by one-third, and the result should assist in deciding on statin therapy.17
Other considerations
Abelhafiz et al reviewed the relationship between cholesterol levels and outcomes in elderly patients especially with regard to body weight and frailty, suggesting that low body weight and frailty are important determinants of increased CVD and that these were associated with low cholesterol levels.39 While their discussion does not address the issue of statin therapy for CVD prevention, caution would appear appropriate in considering lipid treatment in frail and thin elderly patients.39
Proposed guidelines for lipid management in the elderly
All patients aged 65 years or more with one or more of the following CVD risk factors should be considered for treatment with lipid-modifying therapy:
- Previous atherothrombotic cardiovascular disease (ATCVD).
- Hypertension (BP>150/80 or on hypertensive therapy).
- Low HDL-C (<1.0 mmol/L).
- Diabetes mellitus.
- Renal impairment (estimated glomerular filtration rate <60 mL/min).
- Metabolic syndrome (central obesity with one or more of low HDL-C <1.0 mmol/L, high TGs >2.3 mmol/L, fasting glucose >6 mmol/L).
- Fasting TGs >2.3 mmol/L (and high CVD risk).
- Coronary calcium score >300 Agaston units.
- Peripheral vascular disease (including demonstration of atherosclerotic plaques on arterial ultrasound).
- Patients considered for statin therapy are required to have appropriate life expectancy for benefits of statin therapy to be realized. In most situations, a life expectancy of 5 years or more is reasonable.
- Patients considered for statin therapy are required to have clear explanation of the rationale for statin therapy, the potential benefits and side effects, and the need for monitoring efficacy and tolerability.
- Possible exceptions to the use of statins include the following:
- Patients with low life expectancy <5 years
- Patients with no recognized CVD risk factors in addition to one or more of the following:
- Low coronary calcium score (<100 Agaston units)
- Low LDL-C (<2.5 mmol/L) in the absence of secondary causes such as extreme weight loss, gastrointestinal disorders, or malignancy
- Patients at increased risk of statin side effects
- Low body mass (BMI <18 kg/m2)
- Women aged >80 years
- Severe comorbidities
- Previous ADRs with statins.
- Statins should be used at minimal effective doses in order to achieve the required (target) LDL-C levels.
- Target LDL-C levels are as follows:
- At least 30% reduction in LDL-C
- And/or LDL-C <2.5 mmol/L (patients without established CVD) and LDL-C <1.8 mmol/L (patients with established CVD).
- Patients on statins require more assiduous monitoring for adverse effects.
- Ezetimibe can be used if statins are not tolerated, and can be added to low to moderate dose statin therapy in order to achieve desired target LDL-C levels. In this way, ADRs are likely to be minimized and LDL-C reduction is enhanced. This recommendation is consistent with the results of the IMProved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE IT) (to be presented late 2014).40
- Fibrates are indicated to treat mild to moderate hypertriglyceridemia (>2.3 mmol/L) in the presence of low HDL-C (<0.9 mmol/L). Fibrates should be used for patients with TG >10 mmol/L to reduce the risk of pancreatitis as well as omega-3 fatty acids (EPA and DHA) 2–4 g/day.
- Maintaining optimal nutrition is an important consideration in elderly patients, and the involvement of a dietitian in lipid management is recommended.
These recommendations are a consensus of the authors after reviewing the literature and current guidelines for treating lipids in the elderly population and in view of their clinical experience.
Summary
The decision to prescribe lipid-lowering therapy in the elderly for the prevention of CVD presents challenges. Clinical trial data demonstrates similar RRR as in middle-aged subjects and greater absolute risk reduction consistent with greater baseline absolute risk. In the most elderly (>80 years), treatment decreases CVD events but not total mortality, consistent with high death rates from non-CVD illnesses. Our elderly warrant lipid-lowering therapy for primary and secondary prevention in the context of their absolute CV risk. The current therapeutic nihilism is not justified. It is time for clinicians to “Get with the Guidelines”.
Disclosure
The authors report no conflicts of interest.
References
Simons LA, Simons J, Friedlander Y, McCallum J, Palaniappan L. Risk functions for prediction of cardiovascular disease in elderly Australians: the Dubbo Study. Med J Aust. 2003;178:113–116. | |
Golomb BA. Implications of statin adverse effects in the elderly. Expert Opin1 Drug Saf. 2005;4:389–397. | |
Hamilton-Craig I. Statin-associated myopathy. Med J Aust. 2001;175:486–489. | |
Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA. 2012;307:182–192. | |
Massing MW, Foley KA, Sueta CA, et al. Trends in lipid management among patients with coronary artery disease: has diabetes received the attention it deserves? Diabetes Care. 2003;26:991–997. | |
Heeley EL, Peiris DP, Patel AA, et al. Cardiovascular risk perception and evidence – practice gaps in Australian general practice (the AusHEART study). Med J Aust. 2010;192:254–259. | |
Simons LA, Chung E. Are high coronary risk patients missing out on lipid-lowering drugs in Australia? Med J Aust. 2014;201:213–216. | |
Hamilton-Craig I, Michealides C, Kostner K, Van Bockxmeer F. Current initiatives for detecting patients with familial hypercholesterolemia in primary care. Lipid Spin. 2013;11:5–10. | |
Holmes HM, Hayley DC, Alexander GC, Sachs GA. Reconsidering medication appropriateness for patients late in life. Arch Intern Med. 2006;166:605–609. | |
Australian Institute of Health and Welfare 2012. Australia’s health 2012. Australia’s health series no13. Cat no AUS 156. Canberra: AIHW. Available from http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=10737422169. Accessed 19 January, 2015. | |
Australian Institute of Health and Welfare 2008. Australia’s health 2008. Cat no AUS 99. Canberra: AIHW. Available from http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=6442453674. Accessed 19 January, 2015. | |
Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. | |
Bang LM, Goa KL. Pravastatin: a review of its use in elderly patients. Drugs Aging. 2003;20:1061–1082. | |
Noaman S, Ibrahim JE, Grenfell R. Prescribing statins for cardiovascular disease prevention in the old: an absence of evidence and an absence of guidelines. Heart Lung Circ. 2014;23:619–624. | |
Treatment for cardiovascular disease. AIHW; 2013. Available from: http://www.aihw.gov.au/cardiovascular-health/treatment/. Accessed July 2, 2014. | |
Kannel WB. Coronary heart disease risk factors in the elderly. Am J Geriatr Cardiol. 2002;11(2):101–107. | |
Prospective Studies Collaboration. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55 000 vascular deaths. Lancet. 2007;370:1829–1839. | |
International Atherosclerosis Society. An International Atherosclerosis Society Position Paper: Global Recommendations for the Management of Dyslipidemia; 2013. Available from: http://www.athero.org/download/IASPPGuidelines_FullReport_2.pdf. Accessed July 2, 2014. | |
Hippisley-Cox J, Coupland C, Robson J, Brindle P. Derivation, validation, and evaluation of a new QRISK model to estimate lifetime risk of cardiovascular disease: cohort study using Q Research database. BMJ. 2010;341:c6624. | |
Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–329. | |
Jackson R, Kerr A, Wells S. Vascular risk calculators: essential but flawed clinical tools? Circulation. 2013;127:1929–1931. | |
Tota-Maharaj R, Blaha MJ, McEvoy JW, et al. Coronary artery calcium for the prediction of mortality in young adults <45 years old and elderly adults >75 years old. Eur Heart J. 2012;33:2955–2962. | |
Roberts CG, Guallar E, Rodriguez A. Efficacy and safety of statin monotherapy in older adults: a meta-analysis. J Gerontol A Biol Sci Med Sci. 2007;62:879–887. | |
Mihaylova B, Emberson J, Blackwell L, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–590. | |
Lloyd SM, Stott DJ, de Craen AJ, et al. Long-term effects of statin treatment in elderly people: extended follow-up of the PROspective Study of Pravastatin in the Elderly at Risk (PROSPER). PLoS One. 2013;8:e72642. | |
Allen Maycock CA, Muhlestein JB, Horne BD, et al. Statin therapy is associated with reduced mortality across all age groups of individuals with significant coronary disease, including very elderly patients. J Am Coll Cardiol. 2002;40:1777–1785. | |
Miettinen TA, Pyörälä K, Olsson AG, et al. Cholesterol-lowering therapy in women and elderly patients with myocardial infarction or angina pectoris. Circulation. 1997;96:4211–4218. | |
Hunt D, Young P, Simes J, et al. Benefits of pravastatin on cardiovascular events and mortality in older patients with coronary heart disease are equal to or exceed those seen in younger patients: results from the LIPID trial. Ann Intern Med. 2001;134:931–940. | |
Lewis SJ, Moye LA, Sacks FM, et al. Effect of pravastatin on cardiovascular events in older patients with myocardial infarction and cholesterol levels in the average range. Results of the cholesterol and recurrent events (CARE) trial. Ann Intern Med. 1998;129:681–689. | |
Al-Khadra S, Meisinger C, Amann U, et al. Secondary prevention medication after myocardial infarction: persistence in elderly people over the course of 1 year. Drugs Aging. 2014;31:513–525. | |
Sarwar N, Danesh J, Eiriksdottir G, et al. Triglycerides and the risk of coronary heart disease. Circulation. 2007;115:450–458. | |
Asia Pacific Cohort Studies Collaboration. Serum triglycerides as a risk factor for cardiovascular disease in the Asia-Pacific region. Circulation. 2004;110:2686–2687. | |
Kotseva K, Wood D, De Backer G, Pyorala K, Keil U, EUROASPIRE Study Group. EUROASPIRE III: A survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur J Cardiovasc Prev Rehabil. 2009; 16:121–137. | |
Jun M, Foote C, Lv J, et al. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet. 2010;375:1875–1884. | |
Catapano AL, Reiner Z, De Backer G, et al; ESC Committee for Practice Guidelines (CPG) 2008–2010 and 2010–2012 Committees, European Association for Cardiovascular Prevention and Rehabilitation. ESC/EAS Guidelines for the management of dyslipidaemias. The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis. 2011;217:3–46. | |
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–2934. | |
National Vascular Disease Prevention Alliance. Consensus statement for the prevention of vascular disease. Aust Fam Physician. 2004;33:235–239. | |
NICE clinical guideline. Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. NICE clinical guideline 67; 2010. Available from: http://www.nice.org.uk/guidance/cg67. Accessed July 2, 2014. | |
Abelhafiz AH, Loo BE, Hensey N, Bailey C, Sinclair A. The U-shaped relationship of traditional cardiovascular risk factors and adverse outcomes in later life. Aging Dis. 2012;3:454–464. | |
IMPROVE-IT: ‘Modest’ Benefit When Adding Ezetimibe to Statins in Post-ACS Patients. Available from: http://www.medscape.com/viewarticle/835030. Accessed 19 Jan 2015. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

