Back to Journals » Medical Devices: Evidence and Research » Volume 12
Length of stay after introduction of a new total knee arthroplasty (TKA)—results of a German retrospective database analysis
Authors Brüggenjürgen B , Muehlendyck C , Gador LV, Katzer A
Received 19 October 2018
Accepted for publication 30 April 2019
Published 7 August 2019 Volume 2019:12 Pages 245—251
DOI https://doi.org/10.2147/MDER.S191529
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Scott Fraser
Bernd Brüggenjürgen,1 Christian Muehlendyck,2 Laura-Valentina Gador,2 Alexander Katzer3
1Faculty Leadership and Management, Steinbeis Hochschule Berlin GmbH, Berlin, Germany; 2Johnson & Johnson MEDICAL GmbH, Norderstedt, Germany; 3Orthoclinic Hamburg GbR, Hamburg, Germany
Background: Although total knee arthroplasty (TKA) procedures are increasing, patient satisfaction is still inferior compared to total hip arthroplasty. The ATTUNE® Knee System was designed to reduce pain and improve function, leading to greater patient satisfaction and decreased resource utilization in TKA. The objective of this study was to compare length of stay (LOS) of TKA with ATTUNE knee versus LCS® knee implants.
Methods: A retrospective chart review analysis in a German center was conducted between 2008 and 2016. All patients without prior ipsilateral knee operation, treated with a cemented LCS or ATTUNE knee were included. Endpoints captured included gender, age, availability of home support, prior contralateral TKA, ASA grade and LOS. Statistical analyses included chi-squared test for differences in patient demographics and Welch two-sample t-test for difference in LOS.
Results: Mean LOS in the ATTUNE Knee group (N=85) was 8.3 days (SD: 1.79) compared to 10.4 days (SD: 1.91) in the LCS knee group (N=85). No significant differences in gender, age, availability of home support, prior contralateral TKA, or ASA grade between both cohorts were observed. The 2.1 days reduction was statistically significant (P<0.001; 95%CI: 2.7–1.6). A sensitivity analysis outlined the impact of the study duration: even when assuming that 1.3 days reduction resulted from the observed national LOS decrease, the remaining 0.8 reduction in days LOS reduction was still significant (P<0.01).
Conclusion: When comparing two cohorts with similar sociodemographic and medical factors, LOS of ATTUNE knee patients was 2.1 days shorter than patients treated with the LCS knee.
Keywords: total knee arthroplasty, ATTUNE Knee System, length of stay, Germany
Introduction
Patients suffering from osteoarthritis of the knee are characterized by increasing pain, reduced function and decreasing range of motion. When all conservative treatment options have been exhausted, patients typically receive a total knee arthroplasty (TKA) if clinically justified.
However, 16% of primary knee replacement patients rate their satisfaction as poor or fair and up to 25% of patients have anterior knee pain following TKA.1,2 Beverland reports long-term discrepancies between the outcomes of total hip arthroplasty and TKA: 55% of hip replacement patients achieved positive results after 10 years, whereas only in 4% of TKA patients positive long-term results, ie resulting in a “forgotten” knee, could be observed.3
Approaches to improve the situation have to address several aspects, as factors influencing the outcomes of a TKA procedure are multifactorial including patient demographics, comorbidities, the hospital setting, surgical process (ie the instruments that help surgeons implant total knee devices), implant design and recovery principles.4 Furthermore streamlining of both the TKA treatment as well as the recovery process is required to reduce utilization of health-care resources and to meet increasing patient demand for improved functioning.5
The ATTUNE® Knee System (DePuy Synthes, Warsaw, IN, USA) has been designed to accommodate patient variation, soft tissue interaction and to optimize patella tracking.6 Amongst other features a gradually reducing femoral radius allows for a smooth transition during knee bending to produce high stability of the knee by minimizing unnatural sliding of the femur on the tibia.7 First clinical studies and registry results comparing the ATTUNE knee and other knee systems indicate clinically relevant improvements in a wide range of patient-reported outcomes and confirm surgeons’ reports of less pain, increased range of motion and earlier mobility with the ATTUNE Knee System.8,9
The economic burden associated with osteoarthritis is substantial and increasing. In Germany expenditures for osteoarthritis (ICD-10 M15–M19) accrued to €7.62 billion in 2008.10 Osteoarthritis is the main cause for a primary TKA accounting for 96% of all cases.10 Whilst these surgeries are considered highly cost effective and clinically beneficial they result in an average inpatient cost of €7,106 per patient to be borne by the statutory health insurance.11 In Germany, the number of TKAs performed has consistently increased since early 2000, with 173,304 TKAs performed in 2015, making knee joint replacement among the 20 most common hospital procedures in Germany.12 Due to changes in demography as well as morbidity, such as the aging society or increasing prevalence of obesity, the overall incidence of TKA is expected to rise further in the coming decades even in conservative estimate scenarios.13
Hospitals are subject to strong cost pressures and pursue several measures in an effort to contain costs. In US settings some of the rising costs in TKA surgery could be offset by reducing length of stay (LOS) as one of the major cost drivers.14 Also in Germany the reduction in length of hospitalization is one of the key cost-controlling factors.15 Hence, improving patient outcomes while reducing LOS in TKA patients would support cost containment. For this reason, a wide variety of approaches, eg complex enhanced recovery programs, have been initiated in many centers. First results for the ATTUNE Knee System with primary TKA in the UK indicate that a strong potential to LOS can be associated with the ATTUNE Knee System. At the Nottingham University Hospital a reduction of 1 day from 6.6days with the ATTUNE Knee System compared to the Columbus® Knee (95%CI: 0.1–1.9, P=0.0197) and of 0.8 days from 6.4 days compared to the SIGMA® Knee (95%CI: 0.1–1.5, P=0.0212) could be achieved whilst improving patient outcomes.16
To our knowledge no published LOS analyses are available for the German setting. Hence, the objective of this study was to analyze the potential impact on LOS after the introduction of the ATTUNE Knee System in a German hospital.
Methods
Our analysis is based on a single center chart review of the hospital controlling system of a single surgeon team and applied a retrospective cohort study design, where the type of knee system was changed as the cohort intervention. No other organizational or procedural changes took place during the study period and no enhanced recovery programs were implemented. Proactive patient mobilization under full weight was driven by physiotherapists twicedaily according to their individual ability from day 1 after surgery. Criteria for discharge for all patients were: uncomplicated wound healing, flexion of 0-0-90 and ability to walk stairs on crutches.
The patients were operated either in intubation anesthesia (ITN) or spinal anesthesia. There was no change in the pain or wound care management. Postoperatively all patients received nonsteroidal antiinflammatory drugs (NSAIDs) (1–1–1 600 mg ibuprofen) as base medication and if required Targin (Mundipharma Deutschland GmbH & Co. KG, Frankfurt, Germany) (oxycodon + naloxon) (20/10 mg 1–0–1) upon individual requirement. None of the patients were catheterized or received blood transfusion. No intra-articular pain management was applied. Skin was closed with surgical staples. The wound was inspected daily.
Patients with potential risk of intensive care unit (ICU) requirements were operated on ata different hospital. As the patient data was derived from the hospital controlling system and not from the patients’ medical records no information on complications was available.
The implants were applied according to the instructions for use. No change of the surgical technique took place. All patients were operated based on the concept of tibia first and according to the geometry of the implant.
Between July 2008 and May 2013, the standard of care for primary TKAs in this center was the LCS Knee System, which changed in June 2013 with the first implantation of the ATTUNE Knee System. Each cohort comprised a total of 88 consecutively enrolled patients. Patients were only included if no prior surgical procedures had been performed on the affected knee. Patients were excluded if the reported LOS was more than 15 and less than 5 days as due to privacy requirements these were provided only as a categorical value. Hence, 5 cases (3 LCS knees and 2 ATTUNE knees) with more than 15 days and 1 ATTUNE knee-case with less than 5 days LOS were excluded from further analyses.
The following base case characteristics, to support subsequent analysis, were documented: gender, age, availability or lack of support at home after discharge, previous contralateral TKA and ASA-risk categories. Due to data privacy regulations, date of TKA surgery was not provided in the dataset and age was provided in 10-year categories (41–50 years, 51–60 years, 61–70 year, 71–80 years). With disclosing date of procedure as well as date of birth and due to the pseudonymization of the retrospective data which did not allow for re-identification of the patients, the ethics committee of the Hamburg Medical Association did not require further approval.
The primary objective of this analysis was the change in LOS when switching from the LCS Knee System to the ATTUNE Knee System. Distributions and measures of central tendency were analyzed for both cohorts in order to evaluate the need to adjust for potential bias. Differences in independent variable distributions depending on the applied knee system were tested with the chi-squared test and the Mann–Whitney U test. If a significant difference (5% level) was observed, an adjusted analysis of the difference in LOS via an ANOVA was to be conducted. If a comparable distribution of independent variables was observed a Welch two-sample t-test was to be performed.
Results
170 (97%) of 176 patients provided LOS information (85 ATTUNE knees, 85 LCS knees). Sixty percent of all TKApatients were women. Five percent of all patients were 41–50 years old, 13% 51–60 years, 30% 61–70 years, 44% 71–80 years, and 8% were older than 80 years. Eighteen percent of all TKApatients had a previous TKA in the contralateral knee. Mean LOS of the total cohort (N=176) was 9.3 days.
Both TKA cohorts revealed a similar gender distribution (see Figure 1) No significant differences could be observed (χ2=0.025, P=0.86).
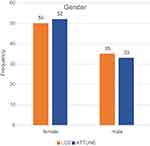 |
Figure 1 Gender distribution by knee system. |
Minor differences were observed when comparing the age distribution of each TKA cohort. For the LCS Knee System more patients were observed in the age category 61–70 years, whereas ATTUNE knee patients were represented more often in the groups 51–60 and 71–80 years (see Figure 2). However, differences were statistically non-significant (Mann–Whitney U test, P=0.80).
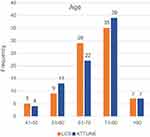 |
Figure 2 Age distribution by knee system. |
The availability of home support and perioperative ASA physical status classification system were comparable for both cohorts with no statistically significant difference reported (availability of home support: χ2=0.24, P=0.62; ASA: χ2=0, P=1) (see Figures 3 and 4). Previous TKA in the contralateral knee were reported in 12 LCS patients and 19 ATTUNE knee patients also reaching no statistically significant difference (χ2=1.420283 d.f.=1 P=0.23).
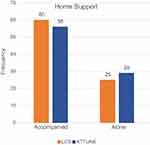 |
Figure 3 Distribution of home support by knee system. |
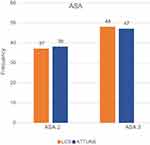 |
Figure 4 Distribution of ASA-categories by knee system. |
When analyzing the dependent primary variable LOS the histogram shows a left shift of LOS for the ATTUNE Knee System(see Figure 5).
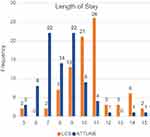 |
Figure 5 Frequency distribution of length of stay by knee system. |
Mean LOS was 10.4 (SD: 1.91) in the LCS knee group and 8.3 in the ATTUNE knee group (SD:1.79). This equals a LOS reduction of 20%. As both TKA-cohorts showed no difference in distributions of independent patient variables, differences in LOS for both cohorts were analyzed using the Welch two-sample t-test. This analysis revealed a statistically significant reduction in LOS of 2.1 days (P<0.001; 95%CI: 2.7–1.6) when changing from LCS to the ATTUNE Knee System.
Discussion
The present study is the first analysis of LOS for TKApatients comparing the LCS and ATTUNE Knee Systems in Germany. Each cohort comprised of 85 evaluable patients, treated in one single center by a single surgeon team which applied consistent pre-, intra- and postoperative treatment and mobilization principles. All patients were mobilized according to their individual ability and as quickly as possible from day 1 after surgery. The patients were comparable with regard to baseline characteristics; age, gender, availability of home support, prior contralateral TKA, and perioperative ASA-classification categories. Hence, no adjustment was needed from a statistical point of view. Mean LOS for patients with LCS knees was 10.4 days and 8.3 days for ATTUNE knee patients.
Length of stay is known to be influenced by surgical factors (such as demand for blood transfusions) as well as presurgical patient characteristics, such as age, body mass index (BMI) and ASA-classification categories.17 With the exception of BMI, all relevant presurgical influencing factors could be analyzed in this study and no significant differences in variable distribution between cohorts were observed. Hence, it can be assumed that a bias due to sociodemographic or medical factors impacting the LOS difference is low.
Length of stay reduction is influenced both by regional and by national health-care settings. This center is located in Hamburg and the state of residence (Bundesland) might have had an impact on LOS changes. In Bremen, for example, LOS reduced by 10% between 2007 and 2011, whereas in Hamburg and Thüringen a 4% reduction was reported in the same time period only, resulting in a negligible potential impact of the external regional setting on LOS.18 From a national point of view an average national decline in LOS was reported for Germany.19 Hence, we performed a sensitivity analysis for the potential impact of a parallel nationwide reduction in LOS. Due to data privacy regulations, exact date of surgery was not provided and only whole cohort periods could be analyzed (LCS Knee System, from July 2008 to May 2013 and ATTUNE Knee System, from May 2013 to June 2016). The average LOS in Germany for the implantation of bicondylar knee endoprothesis (DRG I44B) was 12.6 days during the LCS knee period and 11.3 days during the ATTUNE knee period resulting in an average national LOS decrease of 1.3 days.19 Even when assuming 1.3 days of the total 2.1 day reduction observed resulted from national decrease, the remaining 0.8 days in LOS reduction in the ATTUNE knee cohort is highly significant (P<0.01) and represents a 38% greater reduction in LOS compared to the nationally reported decrease. As the decline of overall LOS in Hamburg was among the lowest reported, the assumption that a part of the LOS reduction was caused by the nationwide reduction is a very conservative sensitivity estimate.
A comparative analysis of five different TKA prostheses identified device type as the major determinant with regard to change in cost-effectiveness ratios of TKA and impact on patient outcomes, such as function and quality of life.20 The ATTUNE Knee System has shown significant improvements in several patient-reported outcome measures and is known to be associated with reduced patellofemoral pain and crepitus compared to other knee systems.21–23 A US database study comparing a total of 1,178 ATTUNE knee patients and 5,707 Triathlon® knee patients reported a significant reduction of unadjusted mean LOS reduction of 0.19 days from 3.13 days for the Triathlon® knee patients to 2.94 days (P<0.001) for the ATTUNE knee patients.24
In addition, the study showed that the adjusted odds for ATTUNE knee patients being discharged to a skilled nursing facility (SNF) were 39% lower than for Triathlon® knee patients (OR=0.61; 95%CI: 0.50–0.75; P<0.001).24 A prospective UK study observed a statistically significant reduction in LOS by 1.2 days (95%CI: 0.5–1.9, P<0.001) when comparing the SIGMA knee with the ATTUNE knee. The same study also reported a significantly greater improvement in the Knee Society Knee Score (KSKS) in the ATTUNE knee group (difference: 8.4, 95%CI: 0.1–16.7, P=0.049) after 1 year compared to the SIGMA knee.25 A study at Nottingham University Hospital in the UK (719 patients with primary TKA) reported a reduction of 1 day with the ATTUNE Knee System (N=238) compared to the Columbus® knee (N=149) (95%CI: 0.1–1.9) and 0.8 days compared to the SIGMA knee (N=332) (95%CI: 0.1–1.5) resulting in up to 15% reduction from baseline.16 A retrospective analysis in Italy observed a 29% LOS reduction. Patients implanted with the ATTUNE knee demonstrated a 4-day reduction in adjusted mean LOS compared to patients with the SIGMA knee (95%CI: 3.5–4.5, P<0.0001). Adjusted mean LOS for ATTUNE knee patients was 9.7 days (SD: 1.2) vs adjusted mean LOS of 13.7 days (SD: 1.9) for SIGMA knee patients.26 Hence, the observed reduction of 20% in LOS in our study is in the scope of international results.
Limitations of this study are the historic cohort design, the long study period, the data privacy related lack of the specified date of surgery and the use of the hospital controlling data base vs the medical patient records. Hence, next to the introduction of the ATTUNE Knee System, factors such as surgical setting, comorbidities and health system changes, might have influenced the observed LOS to some degree. However, as discussed above, these factors had a low impact only. A further minor limitation is the unavailability of date of surgery due to the data privacy regulations. Although our surgical team reported a fast early “learning curve”, we could not statistically verify this with a surgery date based analysis. Such an initially modest reduction in LOS after introducing the new ATTUNE Knee System followed by a more pronounced LOS reduction later was already reported by Huey et al where the first 10 ATTUNE knee cases obtained a lesser decrease in LOS compared to the subsequent procedures.27
A strength of the present study is the unique application of only one device type as an institutional standard of care during each cohort study period. In addition, all surgeries during the study period were performed by a single unchanged surgical team consisting of only two skilled senior surgeons with a consistent treatment and proactive patient-adapted mobilization approach, which results in an exclusion of further potential bias. Furthermore, despite a long study period, TKA cohorts were comparable with regard to relevant patient variables.
National LOS of TKA patients in Germany of 11 days in 2016 is still high compared to other health-care systems. In 2011 Gaughan et al reported an average LOS of 6.9 days for the UK.28 In the US 80% of all TKApatients are discharged within 3 days of TKA surgery. These variations are largely driven by the differences in the health-care systems, but the lower LOS observed in some countries highlights the potential to further reduce LOS in Germany.29 The 2.1 day reduction observed in our study following the adoption of the ATTUNE knee is consistent with LOS reductions reported in studies from other geographical areas and might serve as an easy to implement factor to enhance further reductions in resource utilization while simultaneously guaranteeing advantageous patient outcomes.23,30 The potential benefits for the ATTUNE knee to achieve faster recovery and improve clinical outcomes are aligned to key aims of new hospital regulations; the Hospital Structure Act, including increased patient satisfaction, faster recovery and maximizing functional improvement. Furthermore the new guidelines for quality contracts by the German Federal Joint Committee (G-BA) state the choice of the implant is one of the relevant influencing factor of the treatment success which can be actively addressed by the hospital.31
The observed trend in reducing LOS when applying the ATTUNE Knee System should be confirmed in further prospective studies. These studies should either employ a propensity-score based matched-pair comparison or,as a best case, use a randomized prospective control design in order to identify the particular impact of the applied prosthesis on LOS while also considering the selected mobilization approach.
Conclusion
When comparing the LCS Knee System and ATTUNE Knee System in two consecutive primary TKA patient cohorts in a German center with early and individual mobilization, similar sociodemographic and medical patient characteristics, LOS in ATTUNE knee patients was 2.1 days shorter than patients treated with LCS knee. Sensitivity analysis confirmed the robustness of the results. The observed trend in reducing LOS when applying the ATTUNE Knee System is in line with international results but should ideally be confirmed in prospective randomized studies.
Acknowledgments
The authors thank Johnson & Johnson for an unrestricted grant for data analysis, data extraction and publication.
Disclosure
Prof. Dr B Brüggenjürgen reports grants from J&J Medical, during the conduct of the study. Dr C Mühlendyck is an employee of Johnson and Johnson Medical, Germany. Mrs LV Gador is an employee of Johnson and Johnson Medical, Germany. Prof. Dr A Katzer reports no conflicts of interest in this work.
This paper/the abstract of this paper was presented at:
- ISPOR Europe 2017 as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Value in Health 20 (2017) A399–A811: https://www.valueinhealthjournal.com/article/S1098-3015(17)31460-2/abstract.
- Endoprothetikkongress Berlin, 22–24.02.2018, as a poster presentation with interim findings.
References
1. Porter M, Borroff M, Gregg P, Macgregor A, Tucker K National Joint Registry for England, Wales and Northern Ireland - 10th Annual Report 2013. 2013: 10.
2. Parvizi J, Mortazavi SM, Devulapalli C, Hozack WJ, Sharkey PF, Rothman RH. Secondary resurfacing of the patella after primary total knee arthroplasty does the anterior knee pain resolve? J Arthroplasty. 2012;27(1):21–26. doi:10.1016/j.arth.2011.04.027
3. Beverland D. Patient satisfaction following TKA: bless them all! Orthopedics. 2010;33(9):657.
4. Fisher D, Pakrin D. Improving the value of primary total knee arthroplasty: the ATTUNE® knee system. Attune Knee Syst- Johnson Johnson. 2017.
5. Wiering B, de Boer D, Delnoij D. Meeting patient expectations: patient expectations and recovery after hip or knee surgery. Musculoskelet Surg. 2018;102(3):231–240. doi:10.1007/s12306-017-0523-7
6. Amis AA, Senavongse W, Bull AM. Patellofemoral kinematics during knee flexion-extension: an in vitro study. J Orthop Res. 2006;24(12):2201–2211. doi:10.1002/jor.20268
7. Clary CW, Fitzpatrick CK, Maletsky LP, Rullkoetter PJ) Improving dynamic mid-stance stability: an experimental and finite element study.
8. Hamilton W, Brenkel I, Clatworthy M, Early patient reported outcomes with new primary vs. contemporary total knee arthroplasty: a comparison of two worldwide, multi-center prospective studies. Boston: International Society for Technology in Arthroplasty (ISTA); 2016.
9. National Clinical Guideline Centre (UK). Osteoarthritis: Care and Management in Adults. London: Center NNCG, ed; 2014.
10. Weißer M, Rosery H, Schönfelder T. Gesundheitsökonomische Aspekte. In: Bleß -H-H, Kip M, editors. Weißbuch Gelenkersatz. Berlin: Springer; 2017:111–126.
11. Malzahn J. [Conservative and operative treatment of working age patients with gonarthritis. Economic considerations]. Orthopade. 2014;43(6):
12. Anonymus. Die 20 häufigsten operationen - vollstationär behandelte patientinnen und patienten in Krankenhäuser 2015. Krankenhäuser. 2017. Availble from: https://www.destatis.de/DE/ZahlenFakten/GesellschaftStaat/Gesundheit/Krankenhaeuser/Tabellen/DRGOperationen.html. Accessed April 16, 2017.
13. Inacio MCS, Graves SE, Pratt NL, Roughead EE, Nemes S. Increase in total joint arthroplasty projected from 2014 to 2046 in Australia: a conservative local model with international implications. Clin Orthop Relat Res. 2017;475(8):8. doi:10.1007/s11999-017-5377-7
14. Molloy IB, Martin BI, Moschetti WE, Jevsevar DS. Effects of the length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. J Bone Joint Surg Am. 2017;99(5):402–407. doi:10.2106/JBJS.16.00019
15. Schelhase T. Statistische Krankenhausdaten: diagnosedaten der Krankenhäuser 2013. In: Klauber J, Geraedts M, Friedrich J, Wasem J, editors. Krankenhausreport 2016: Schwerpunkt: Ambulant Im Krankenhaus. Stuttgart: Schattauer; 2016:343–372.
16. Mantel J, Corso K, Wei D, et al. Economic Effectiveness of the ATTUNE® knee system - analysis of real world hospital length of stay and incidence of early complications. Value in Health. 2017;20(9):A579. doi:10.1016/j.jval.2017.08.1023
17. Jonas SC, Smith HK, Blair PS, Dacombe P, Weale AE. Factors influencing length of stay following primary total knee replacement in a UK specialist orthopaedic centre. Knee. 2013;20(5):310–315. doi:10.1016/j.knee.2012.07.010
18. Schelhase T. Statistische Krankenhausdaten: diagnosedaten der Krankenhäuser 2011. In: Klauber J, Geraedts M, Friedrich J, Wasem J, editors. Krankenhaus-Report 2014: Patientensicherheit. Stuttgart: Schattauer; 2014:329–356.
19. Anonymus. Fallpauschalen-Katalog 2008–2016. Siegburg, Germany: InEK GmbH – Institut für das Entgeltsystem im Krankenhaus; 2008–2016.
20. Pennington M, Grieve R, Black N, van der Meulen JH, Green C. van der Meulen JH. Cost-effectiveness of five commonly used prosthesis brands for total knee replacement in the UK: a study using the NJR dataset. PLoS One. 2016;11(3):e0150074. doi:10.1371/journal.pone.0150074
21. Indelli PF, Pipino G, Johnson P, Graceffa A, Marcucci M. Posterior-stabilized total knee arthroplasty: a matched pair analysis of a classic and its evolutional design. Arthroplast Today. 2016;2(4):193–198. doi:10.1016/j.artd.2016.05.002
22. Martin JR, Jennings JM, Watters TS, Levy DL, McNabb DC, Dennis DA. Femoral implant design modification decreases the incidence of patellar crepitus in total knee arthroplasty. J Arthroplasty. 2017;32(4):1310–1313. doi:10.1016/j.arth.2016.11.025
23. Ranawat CS, White PB, West S, Ranawat AS. Clinical and radiographic results of attune and PFC sigma knee designs at 2-year follow-up: a prospective matched-pair analysis. J Arthroplasty. 2017;32(2):431–436. doi:10.1016/j.arth.2016.07.021
24. Etter K, Lerner J, Kalsekar I, de Moor C, Yoo A, Swank M. Comparative analysis of hospital length of stay and discharge status of two contemporary primary total knee systems. J Knee Surg. 2018;31(6):541–550. doi:10.1055/s-0037-1604442
25. Clement N, Brenkel I, Walmsley P. Improved Early Functional Outcome with the Attune Total Knee Replacment: A Propensity Score Matched Trial. In: British Association for Surgery of the Knee 2017. UK: Southport; 2017.
26. Pipino G, Paragò V, Corso KA, Wigham R, Holy CE, Do Rego B. Economic outcomes of the Attune® knee system: analysis of real world length of stay in an Italian hospital. Value Health. 2017;20(9):A595. doi:10.1016/j.jval.2017.08.1116
27. Huey V, Brenkel I, Chang CB, et al. Learning curve with a new primary TKA implant: a worldwide perspective with more than 2000 patients. Orthop Proc. 2017;99-B(Supp 4):1.
28. Gaughan J, Mason A, Street A, Ward P. English Hospitals Can Improve Their Use of Resources: An Analysis of Costs and Length of Stay for Ten Treatments. York, UK : University of York, UK; 2012.
29. Otero JE, Gholson JJ, Pugely AJ, Gao Y, Bedard NA, Callaghan JJ. Length of hospitalization after joint arthroplasty: does early discharge affect complications and readmission rates? J Arthroplasty. 2016;31(12):2714–2725. doi:10.1016/j.arth.2016.07.026
30. Clement N, Brenkel I, Walmsley P. Improved early functional outcome with the attune total knee replacment: a propensity score matched trial; 2017. Availble from: https://risweb.st-andrews.ac.uk/portal/en/researchoutput/improved-early-functional-outcome-with-the-attune-total-knee-replacment-a-propensity-score-matched-trial(a96e719b-79f0-46c8-b709-8cca7962e191).html.
31. Bundesausschuss G. Tragende Gründe Des Gemeinsamen Bundesausschusses Über Die Festlegung Der Leistungen Oder Leistungsbereiche Gemäß § 136b Absatz 1 Satz 1 Nummer 4 SGB V Für Qualitätsverträge Nach § 110a SGB V. In: Bundesausschuss G, ed. Berlin: GBA; 2017.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
