Back to Journals » Medical Devices: Evidence and Research » Volume 7
Laser speckle contrast imaging for intraoperative assessment of liver microcirculation: a clinical pilot study
Authors Eriksson S, Nilsson J, Lindell G, Sturesson C
Received 3 March 2014
Accepted for publication 31 March 2014
Published 25 July 2014 Volume 2014:7 Pages 257—261
DOI https://doi.org/10.2147/MDER.S63393
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Sam Eriksson,1,2,* Jan Nilsson,1,2,* Gert Lindell,1,2 Christian Sturesson1,2
1Department of Surgery, Clinical Sciences Lund, Lund University, 2Skåne University Hospital, Lund, Sweden
*These authors contributed equally to the study
Background: Liver microcirculation can be affected by a wide variety of causes relevant to liver transplantation and resectional surgery. Intraoperative assessment of the microcirculation could possibly predict postoperative outcome. The present pilot study introduces laser speckle contrast imaging (LSCI) as a new clinical method for assessing liver microcirculation.
Methods: LSCI measurements of liver microcirculation were performed on ten patients undergoing liver resection. Measurements were made during apnea with and without liver blood inflow occlusion. Hepatic blood flow was assessed by subtracting zero inflow signal from the total signal. Zero inflow signal was obtained after hepatic artery and portal vein occlusion. Perfusion was expressed in laser speckle perfusion units, and intraindividual and interindividual variability in liver perfusion was investigated using the coefficient of variability.
Results: Hepatic microcirculation measurements were successfully made in all patients resulting in analyzable speckle contrast images. Mean hepatic blood flow was 410±36 laser speckle perfusion units. Zero inflow signal amounted to 40%±4% of the total signal. Intraindividual and interindividual coefficients of variability in liver perfusion were 25% and 28%, respectively.
Conclusion: Under the conditions of this pilot study, LSCI allows rapid noncontact measurements of hepatic blood perfusion over wide areas. More studies are needed on methods of handling movement artifacts.
Keywords: liver surgery, blood perfusion
Introduction
Liver microcirculation can be affected by a wide variety of causes of perioperative interest. In liver transplantation, the liver is subjected to ischemia/reperfusion known to influence postoperative graft function predominantly by sinusoidal perfusion failure;1,2 monitoring of hepatic microcirculation may predict postoperative complications.2 In liver resection, parenchymal injuries due to conditions such as nonalcoholic fatty liver disease and preoperative chemotherapy can influence hepatic microcirculation.3 Morbidity after major hepatectomy is increased in patients with liver parenchymal injuries.4,5 Assessment of liver microcirculation could thus be of interest in determining the liver condition, in order to initiate interventions to inhibit development of graft dysfunction and improve liver transplantation outcome, or to assess how much surgery the liver can withstand.
Techniques used for intraoperative liver microcirculation determination in the clinic include laser Doppler flowmetry (LDF) and video-microscopic techniques such as sidestream dark field (SDF) imaging.6–8 One limitation of these techniques is their single point measurements and, in the case of SDF imaging, time consuming offline analysis.
Laser speckle contrast imaging (LSCI) is yet another method to assess microcirculation, which is extensively used in retinal imaging, skin perfusion, and neurophysiology.9 The technique relies on the speckle phenomenon, speckles being the light and dark areas generated on a detector collecting the backscattered light from a tissue surface illuminated by coherent laser light. Moving red blood cells in the tissue will generate fluctuations, that is blurring, in the speckle pattern on the detector. Speckle contrast is a quantification of the degree of blurring that arises when speckles are captured on a detector with finite exposure time, while red blood cells are moving. An advantage of LSCI is real-time non-contact measurements over large surfaces with excellent reproducibility.10 LSCI results are not quantitative but are expressed as a raw flux value in laser speckle perfusion units (LSPU). LSCI has been validated for assessment of liver microcirculation in rats by comparing results using LSCI with the results using SDF,8 but, to our knowledge, no reports have been published on the use of this technique with human liver material.
Here, we report our first experience using LSCI for intraoperative noninvasive monitoring of liver microcirculation. Ten clinical cases were used to address the feasibility of this imaging technique for intraoperative liver microcirculation assessment.
Materials and methods
The study protocol was approved by the Regional Ethical Review Board in Lund, and written informed consent was obtained from patients. The present pilot study comprised ten consecutive patients undergoing liver resection for colorectal liver metastases at Skåne University Hospital, Lund, Sweden.
Hepatic microcirculation measurements were incorporated in the standard liver resection surgery procedure. A right-sided subcostal incision with an upward midline extension was used to access the liver. Measurements were made after mobilization of the liver from its diaphragmatic attachments but before liver resection. A sling was placed around the hepatoduodenal ligament allowing the blood inflow vessels, consisting of the portal vein and hepatic artery, to be occluded by temporarily tightening the sling, thereby inducing ischemia to the entire liver. Apnea was accomplished by temporarily stopping the respirator ventilation of the patient. Microcirculation measurements were made during 10 seconds with and without apnea, first without blood inflow occlusion and subsequently after 3 minutes of blood inflow occlusion.
A commercially available LSCI instrument (MoorFLPI Speckle Contrast Imager, Moor Instruments Ltd, Axminster, UK) was used to obtain hepatic blood flow data. The instrument was mounted on an adjustable stand and coated with a sterile drape (3M™ Steri-Drape™; 3M Health Care, St Paul, MN, USA), allowing the instrument to be placed steadily over the operation area at a distance of 20 cm above the exposed liver surface, capturing an area of approximately 12×16 cm. With this setting, 785 nm laser light from the instrument could illuminate a large area of the hepatic surface. The camera of the instrument captured the generated speckle contrast representing hepatic circulation. Surface reflections interfering with the blood flow signal were filtered through a polarization filter. Instrument settings were set to 4 ms exposure time, 25 Hz display rate, and a 0.3 second time constant, enabling a high speed capturing of a video sequence with a resolution of 152×113 pixels for further blood flow analysis.
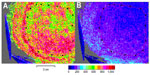
Blood flow analysis was conducted using computer software (moorFLPI Review V3.0, Moor Instruments Ltd) installed on a standard laptop computer. Accompanying the speckle contrast images was a normal video sequence, allowing the investigator to define a region of interest (ROI) representing the part of the liver surface visible to the laser speckle instrument. The most horizontal part of the visible liver was chosen as the ROI in order to reduce geometrical artifacts. In practice, this meant that a peripheral 2 cm rim was excluded from analysis, as shown in Figure 1. Perfusion is presented in LSPU.
Total hepatic signal (THS) was calculated as a mean flux of the chosen ROI during 10 seconds under apnea. Measurements during vascular occlusion and apnea constituted the zero inflow signal (ZIS). By subtracting ZIS from THS, hepatic blood flow (HBF) was obtained. The variability in HBF was investigated using the coefficient of variability (CV) of all the measurements within the ROI at a single mid interval frame. CV is defined as the ratio of the standard deviation to the mean of the perfusion in the defined ROI.
All data are expressed as mean ± standard error of the mean unless stated otherwise. Correlations were made using linear regression analysis and computing a Pearson’s correlation coefficient (r). A P-value of <0.05 was considered statistically significant. Statistical analyses were made using IBM SPSS Statistics software, version 21 (IBM Corporation, Armonk, NY, USA).
Results
Eight men and two women with a median age of 68 years (range 52–77 years) and a body mass index of 27.5±1.2 kg/m2 were included in the study. All patients had normal preoperative hepatic function as assessed by indocyanine green clearance.11 Hepatic microcirculation measurements were successfully made in all patients, resulting in analyzable speckle contrast images. A typical example of a LSCI measurement with and without blood inflow occlusion is shown in Figure 1. Figure 2 demonstrates raw flux signal for the chosen ROI for one typical patient in four different stages. THS and CV for all patients are presented in Table 1. Mean intraindividual CV was 25%. The total duration of the measuring procedure as well as the time needed for subsequent analysis was about 5 minutes per patient. Mean HBF in the study group was 410±36 LSPU, resulting in an interindividual CV of 28%. HBF for each of the ten patients can be seen in Figure 3. The THS (682±37 LSPU) was composed of the sum of ZIS (272±25 LSPU) and HBF. ZIS constituted 40%±4% of THS. The correlation between ZIS and body mass index was almost significant (r=−0.58, P=0.081).
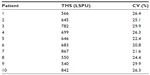  | Table 1 Variability of laser speckle measurements |
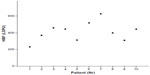  | Figure 3 HBF for each patient. |
Discussion
In this pilot clinical study, we have for the first time assessed hepatic microcirculation using intraoperative LSCI allowing rapid noncontact measurements over wide areas. The method has been validated previously for measurement of liver microcirculation in rats.8 Previous methods for clinical hepatic microcirculation measurements have relied on point surface measurements using either LDF or video-microscopic techniques.2,12 LSCI and LDF have similarities in that both methods measure backscattered light from moving red blood cells13 and former studies using the two methods have shown good correlation when measuring skin perfusion.10,14 In contrast to LSCI, LDF with its single point measurement suffers from both intersite and interindividual variability.15 In this study, we found an intraindividual CV of 25% for THS, suggesting a relatively large intraindividual heterogeneity for hepatic blood flow. These results are similar to what has been shown by Wheatley et al in the rat using LDF with several measuring points.15 Thus, when measuring at single points on the liver, as with LDF, blood perfusion is site dependent. This advocates the use of LDF as a method to measure relative blood perfusion at a single point. LSCI, on the other hand, which uses a larger measuring area, could potentially permit measurements of microcirculation. These could be compared between subjects, although this would give a raw flux value in LSPU rather than a quantitative value.
Since LSCI measurement is even more superficial (less than 1 mm depth) than LDF,13 it is only subsurface microcirculation that is measured. However, we assume surface measurements to be representative also of the more deep-located liver parenchyma.15,16 The noncontact feasibility of LSCI allows measurements without interfering with microcirculation due to pressure influences, which ought to be the case in LDF and SDF imaging.
As shown in Figure 3, there were considerable differences in HBF between patients, resulting in an interindividual CV of 28%, which may seem high because no patient showed any derangement of preoperative liver function tests and all patients had a normal liver on intraoperative visual inspection. Concerning interindividual variability in liver microcirculation measurements on humans, studies using LDF12 and orthogonal polarization spectroscopy2 have also resulted in high values. In addition, a high interindividual CV of 23% to 25% has also been found using other methods for estimating global liver blood perfusion in the clinic, such as magnetic resonance imaging and intraoperative measurement of hepatic blood inflow.17,18 Thus, it appears that the high intersubject variability found in the present study is not only method-related but reflects the apparent differences between individuals with respect to hepatic microcirculation.
Hepatic blood flow as calculated by subtracting the values obtained during blood inflow occlusion and apnea from THS constituted the larger part of the total signal. With inflow occlusion and apnea, we assumed that there was zero perfusion in the liver, as has been shown for experimental animals,8 creating a ZIS. The ZIS signal in the present study was larger than observed on human forearm skin19 and also significantly larger than observed on rat liver.8 In rat experiments where the liver was totally static, ZIS reached a mere 10% of the total perfusion signal. The higher ZIS obtained in the present study most probably emanated from motion artifacts due to heart-beating movements propagated to the liver through the diaphragm. These movements were also visible to the eye. Differences in ZIS between patients could possibly be explained by differences in body constitution. Intuitively, patients with higher body mass index should be able to dampen some of the motion artifacts. However, the correlation between ZIS and body mass index failed to reach statistical significance in this small pilot study.
Sensitivity to movement artifacts appears to be an inherent drawback of the LSCI method because all movements are registered as microcirculation, regardless of whether the movement comes from moving red blood cells or movement of the organ under study. In this study, we simply subtracted the ZIS from the THS to get the HBF. The additive contribution of movement artifacts to the microcirculation LSCI signal has been shown previously by Mahe et al.20 In order to take into account irregular and random movement artifacts, tests have been made using LSCI on skin using an opaque reference area attached to the skin for point-by-point subtraction of artifact signals.20,21 Similar methods could probably be applicable to the liver as well. Breathing artifacts, which are also significant, as shown in Figure 2, are easily compensated for by stopping respirator ventilation during measurement.
In this feasibility study, we present preliminary data of LSCI measurements in ten patients and elucidate some technical challenges with this new method. The small number of patients, and the fact that we did not compare our results with results gained from other methods to measure microcirculation, limit the findings of the study. A future study including a larger number of patients and methods of handling movement artifacts is the next step for investigation of LSCI in clinical use.
In conclusion, we have, for the first time, performed intraoperative hepatic LSCI measurements on human subjects, which were carried out contactless in real time over large areas. The technique holds promise for clinical liver microcirculation assessment. Movement artifacts even during apnea were found to be considerable, amounting to 40% of the total hepatic signal.
Disclosure
The authors report no conflicts of interest in this work.
References
Lemasters JJ, Thurman RG. Reperfusion injury after liver preservation for transplantation. Annu Rev Pharmacol Toxicol. 1997;37:327–338. | |
Puhl G, Schaser KD, Pust D, et al. Initial hepatic microcirculation correlates with early graft function in human orthotopic liver transplantation. Liver Transpl. 2005;11(5):555–563. | |
Seifalian AM, Piasecki C, Agarwal A, Davidson BR. The effect of graded steatosis on flow in the hepatic parenchymal microcirculation. Transplantation. 1999;68(6):780–784. | |
Brouquet A, Benoist S, Julie C, et al. Risk factors for chemotherapy-associated liver injuries: A multivariate analysis of a group of 146 patients with colorectal metastases. Surgery. 2009;145(4):362–371. | |
Vauthey JN, Pawlik TM, Ribero D, et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol. 2006;24(13):2065–2072. | |
Sturesson C, Ivarsson K, Stenram U, Andersson-Engels S, Tranberg KG. Interstitial laser thermotherapy of a rat liver tumour: effect of hepatic inflow occlusion. Lasers Surg Med. 2011;43(1):29–35. | |
Oberg PA. Laser-Doppler flowmetry. Crit Rev Biomed Eng. 1990;18(2):125–163. | |
Sturesson C, Milstein DM, Post IC, Maas AM, van Gulik TM. Laser speckle contrast imaging for assessment of liver microcirculation. Microvasc Res. 2013;87:34–40. | |
Senarathna J, Rege A, Li N, Thakor NV. Laser Speckle Contrast Imaging: theory, instrumentation and applications. IEEE Rev Biomed Eng. 2013;6:99–110. | |
Roustit M, Millet C, Blaise S, Dufournet B, Cracowski JL. Excellent reproducibility of laser speckle contrast imaging to assess skin microvascular reactivity. Microvasc Res. 2010;80(3):505–511. | |
Wiegand BD, Ketterer SG, Rapaport E. The use of indocyanine green for the evaluation of hepatic function and blood flow in man. Am J Dig Dis. 1960;5:427–436. | |
Seifalian AM, Chidambaram V, Rolles K, Davidson BR. In vivo demonstration of impaired microcirculation in steatotic human liver grafts. Liver Transpl Surg. 1998;4(1):71–77. | |
Briers JD. Laser Doppler, speckle and related techniques for blood perfusion mapping and imaging. Physiol Meas. 2001;22(4):R35–R66. | |
Tew GA, Klonizakis M, Crank H, Briers JD, Hodges GJ. Comparison of laser speckle contrast imaging with laser Doppler for assessing microvascular function. Microvasc Res. 2011;82(3):326–332. | |
Wheatley AM, Almond NE, Stuart ET, Zhao D. Interpretation of the laser Doppler flow signal from the liver of the rat. Microvasc Res. 1993;45(3):290–301. | |
Kotzampassi K, Eleftheriadis E, Aletras H. Experimental and clinical evaluation of capsular and parenchymal total liver perfusion. Liver microcirculation. HPB Surg. 1992;6(2):99–104. | |
Yzet T, Bouzerar R, Baledent O, et al. Dynamic measurements of total hepatic blood flow with Phase Contrast MRI. Eur J Radiol. 2010;73(1):119–124. | |
Schenk WG Jr, McDonald DJ, McDonald DK, Drapanas T. Direct measurement of hepatic blood flow in surgical patients: with related observations on hepatic flow dynamics in experimental animals. Ann Surg. 1962;156:463–471. | |
Millet C, Roustit M, Blaise S, Cracowski JL. Comparison between laser speckle contrast imaging and laser Doppler imaging to assess skin blood flow in humans. Microvasc Res. 2011;82(2):147–151. | |
Mahe G, Abraham P, Le Faucheur A, Bruneau A, Humeau-Heurtier A, Durand S. Cutaneous microvascular functional assessment during exercise: a novel approach using laser speckle contrast imaging. Pflugers Arch. 2013;465(4):451–458. | |
Mahé G, Rousseau P, Durand S, Bricq S, Leftheriotis G, Abraham P. Laser speckle contrast imaging accurately measures blood flow over moving skin surfaces. Microvasc Res. 2011;81(2):183–188. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.