Back to Journals » Clinical and Experimental Gastroenterology » Volume 10
Laparoscopic esophageal myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized controlled trials
Authors Baniya R, Upadhaya S, Khan J, Subedi SK, Shaik Mohammed T, Ganatra BK, Bachuwa G
Received 16 December 2016
Accepted for publication 3 July 2017
Published 26 September 2017 Volume 2017:10 Pages 241—248
DOI https://doi.org/10.2147/CEG.S130449
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Andreas M. Kaiser
Ramkaji Baniya, Sunil Upadhaya, Jahangir Khan, Suresh Kumar Subedi, Tabrez Shaik Mohammed, Balvant K Ganatra, Ghassan Bachuwa
Department of Internal Medicine, Hurley Medical Center, Michigan State University, Flint, MI, USA
Background: Achalasia is a primary esophageal motility disorder of unknown etiology associated with abnormalities in peristalsis and lower esophageal sphincter relaxation. The disease is incurable; however, definitive treatment procedures like pneumatic dilation (PD)/balloon dilation and laparoscopic esophageal myotomy (LEM) are performed to relieve dysphagia and related symptoms. Currently, there is paucity of data comparing the outcomes of these procedures. The aim of this meta-analysis is to compare the short- and long-term success rates of PD and LEM.
Methods: A thorough systematic search of PubMed, Scopus, clinicaltrials.gov, and Cochrane library was conducted for randomized controlled trials (RCTs) comparing the outcomes of PD versus LEM in the treatment of achalasia. The Mantel-Haenszel method and random effect model were used to analyze the data. RCTs with outcome data at 3-month, 1-year, and 5-year intervals were analyzed.
Results: A total of 437,378 and 254 patients at 3-month, 1-year, and 5-year intervals were analyzed for outcome data. At 3 months and 1 year, PD was not as effective as LEM (odds ratio [OR]: 0.50; confidence interval [CI] 0.31–0.82; P = 0.009 and OR: 0.47; CI 0.22–0.99; P = 0.21) but at 5 years, one procedure was non-inferior to the other (OR: 0.62; 0.33–1.19; P = 0.34).
Conclusion: PD was as effective as LEM in relieving symptoms of achalasia in the long-term.
Keywords: achalasia, balloon dilation, pneumatic dilation, laparoscopic myotomy, Heller’s myotomy
Introduction
Achalasia is an incurable primary progressive motility disorder of the esophagus where inhibitory ganglionic cells in the myenteric plexus of the lower esophageal sphincter (LES) are irreversibly lost. This leads to impaired relaxation of the LES after swallowing, causing functional obstruction.1–6 The most common symptoms of achalasia are dysphagia, heartburn, regurgitation, aspiration, and weight loss leading to impaired quality of life.7–9 This clinical diagnosis is enhanced by barium swallow studies and endoscopy, and confirmed by manometry.10 Although there is no curative treatment of achalasia, various therapies have been tried in the past without much success.10–15 New options for achalasia peroral endoscopic myotomy (POEM), self-expanding metal stents, endoscopic sclerotherapy have shown promising results but there are only a few prospective observational studies to support their efficacy.15–23 Current standard of care for achalasia includes forceful pneumatic dilation/balloon dilatation (PD/BD) and laparoscopic (Heller’s) esophageal myotomy (LEM) with or without an anti-reflux procedure.15 There are some randomized controlled trials (RCTs) comparing the success rate (improvement of dysphagia) of these procedures at short-term follow-up,8,24–26 but there are only 3 RCTs comparing the long-term outcomes at 5 years published till date.27–29 Although there are systematic reviews and meta-analyses on prospective studies and non-RCTs,30 there is only one meta-analysis of RCTs comparing the outcomes of these two procedures in the short-term.31 Herein, we analyzed the published RCTs to study the short- and long-term success rates of these procedures in order to shed light on this controversial issue.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement for reporting meta-analysis and systemic reviews32 as recommended by the Cochrane Collaboration was used for this meta-analysis (Figure 1). A comprehensive electronic literature search was conducted for all the clinical trials on treatment of esophageal achalasia between the years 2000 and 2016 on PubMed, Embase, Scopus, Cochrane Library, clinicaltrials.gov, Ovid Medline, and Google scholar using the all-field “Achalasia, Esophageal”, all-fields “Balloon dilation” or “Pneumatic dilation, and all-fields “Myotomy” or “ Laparoscopic Heller’s Myotomy” or “Laparoscopic esophageal myotomy”; all three search headings were connected with Boolean operator “AND”. The eligibility criteria for the included studies relied on previously published guidelines for systematic reviews and were based on the PICO framework: P (Population: patients with idiopathic primary achalasia diagnosed with the help of clinical, endoscopic and manometric, and radiographic evidence), I (Intervention: repeated BD/PD), C (Comparative intervention/control group: LEM/Heller’s myotomy), and O (Outcomes: improvement in dysphagia score). Only RCTs published in English were included. Patients were randomly assigned to PD or LEM group. Studies with at-least 3-month follow-up were included. Two reviewers (RB and SU) independently assessed the eligibility and validity of each study. Any disagreements were resolved with discussion with the third and fourth authors (JK and SKS). The fifth, sixth, and seventh authors (TSM, BKG, and GB) evaluated the quality of the studies independently and any disagreement was resolved via discussions among all the reviewers, ultimately reaching to an agreement by consensus. This search parameter yielded 393 articles. Case reports, retrospective studies, letters, comments, and studies without the availability of the data were excluded. Only human studies were included. A total of 5 RCTs met the aforementioned criteria. Quality of the included studies was assessed with the Delphi Consensus criteria for RCTs (Table 1).33
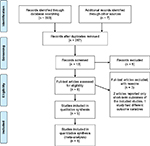  | Figure 1 PRISMA statement of the study. Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analysis. |
  | Table 1 Results of quality assessment by Delphi consensus criteria |
From all the selected studies, we extracted the baseline study details (Table 2): total number of patient enrolled, number of patients in each arm, mean age, sex ratio, inclusion and exclusion criteria, procedure detail (Tables 3 and 4), randomization process, definition of success or failure, adverse events, and quality of life score. Success rate was measured at 3 months, 1 year, and 5 years. The outcomes were calculated with RevMan, version 5.2 for Windows (Cochrane Collaboration, Oxford, UK). Analysis was performed by Mantel-Haenszel test. Odds ratio (OR) was calculated using confidence interval (CI) of 95%. Heterogeneity was calculated using I2. A randomized model was used because of the low heterogeneity from the low number of studies. A P-value of <0.05 was considered significant. The primary analysis focused on symptom resolution as the outcome of interest. This was based on various dysphagia scores in each study. Success rate was evaluated by using improvement validated tools like Watson dysphagia score34 by Persson et al,27 Eckardt score35 by Moonen et al,28 Demeester’s grading of dysphagia5 by Hamdy et al,26 and Vantrappen and Hellemans score36 by Borges et al37 and Novais and Lemme25 (Table 5).
  | Table 3 Pneumatic dilation/balloon dilation procedure of included studies Abbreviations: RCT, randomized controlled trial; PD, pneumatic dilation. |
  | Table 4 Laparoscopic surgical procedure of included studies Abbreviation: RCT, randomized controlled trial. |
  | Table 5 Outcome measure or primary endpoint for included studies Abbreviation: RCT, randomized controlled trial. |
Results
A total of 437 patients at 3-month interval, 378 patients at 1-year interval, and 254 patients at 5-year interval were analyzed for success rate of the procedure, namely the improvement in the dysphagia score. At 3 months, success rate was significantly lower in patients with BD (OR: 0.50; CI 0.31–0.82; P = 0.02). At 1 year, success rate was still significantly lower in BD (OR: 0.47; CI 0.22–0.99; P = 0.99) but nearing non-inferior levels. At 5 years, BD was non-inferior to myotomy (OR: 62; CI 0.33–1.19; P = 0.15) (Figure 2). In an RCT, not included in our study, by Chrystoja et al,29 no significant difference was found in the improvement of achalasia severity questionnaire at 1 year (score difference: 7.3; CI −4.7 to 19.3; P = 0.23 at 1 year) and 5 years (score difference: 0.5; CI −13.5 to 14.4; P = 0.95).
  | Figure 2 Forest plot of response rate at (A) 3 months, (B) I year, and (C) 5 years. Abbreviations: CI, confidence interval; M-H, Mantel-Haenszel. |
Discussion
Achalasia is a primary motor disorder of the esophagus that is chronic and incurable. Although LEM and PD are the mainstays of treatment, the best modality remains controversial.4 Both treatment approaches carry a variable risk of recurrence of symptoms, perforation, and gastrointestinal reflux.38 Therefore, it is imperative to identify the best method for the short- and long-term symptom relief with due consideration of complications. Our study compared the short- and long-term outcomes of the two procedures based on symptom relief at 3 different intervals. Our analysis shows that LEM is better at 3 months and at 1 year (with increasing confidence interval), while PD becomes non-inferior to LEM at 5 years. These results indicate that both treatment approaches lead to comparable outcomes in the long run.
In contrast to LEM, one major advantage of PD is that it can be performed safely in the outpatient setting without need for general anesthesia. However, more patients in single PD group require re-intervention compared to those treated with LEM.39 Although the remission rate is higher with graded dilation approach,40–43 it is associated with higher rates of perforation and complex surgery44 LEM, on the other hand, has the major risk of mucosal tear, and leads to abdominal wall trauma requiring longer recovery time.
In a meta-analysis by Yaghoobi et al,31 LEM provided greater relief of symptoms compared to graded dilation. The main limitation of the study was the lack of long-term follow-up and a small number of included studies. The network meta-analysis by Schoenberg et al45 corroborated these findings. The study did not include long-term follow-up and included indirect comparison. In another meta-analysis by Campos et al,30 LEM was found to be more effective and long lasting compared to BD or botulin toxin injection. However, the complication rate was higher in the surgical group due to the invasiveness of the procedure. In this regard, PD was deemed more suited for frail patients who are poor surgical candidates, or for those patients who fail surgery. However, the results of these studies have to be interpreted with caution as these studies often use variable and subjective definitions of success rate. Furthermore, some of the studies included in the analysis used data from single dilations, while it is well known that it is a multistage procedure with graded dilation.46 In lieu of the largest RCT, the European Achalasia Trial,28 the present meta-analysis is the only one of its kind to include this in the analysis.
The other consideration for this study is the evolving technique of the procedure. The technique of dilation has evolved from rigid dilators to hydrostatic balloon. This allows achievement of maximum controlled volume with low pressure, which improves efficacy and prevents perforation.47 The hypothesis that BD causes the disruption of muscular layer has been challenged by the study by Borhan-Manesh et al.48 The finding shows that PD works by circumferential stretching of the LES. This has resulted in modification of the current method of dilation by slowing the rate of inflation, leading to increased remission rate of BD. POEM is a newer technique that is being used to perform myotomy of the LES. Long-term data from RCTs comparing POEM with conventional treatment methods are lacking. This procedure is still evolving and its role in management of achalasia is not clearly outlined.49 Further studies comparing conventional treatment with POEM with a longer follow-up will be needed for change in practice. Thus, PD or LEM continues to remain the standard of care for achalasia with comparable outcome in the long-term.
Conclusion
Taken together, the data presented here provide evidence that both treatments have similar success rate at 5 years. So, eligible patients should be given the option of PD or LEM at this time.
Disclosure
The authors report no conflicts of interest in this work.
References
Gockel I, Müller M, Schumacher J. Achalasia--a disease of unknown cause that is often diagnosed too late. Dtsch Arztebl Int. 2012;109(12):209–214. | ||
Roll GR, Rabl C, Ciovica R, Peeva S, Campos GM. A controversy that has been tough to swallow: is the treatment of achalasia now digested? J Gastrointest Surg. 2010;14 (Suppl 1):S33–S45. | ||
Chuah SK, Hsu PI, Wu KL, Wu DC, Tai WC, Changchien CS. 2011 update on esophageal achalasia. World J Gastroenterol. 2012;18(14):1573–1578. | ||
Richter JE. Achalasia – an update. J Neurogastroenterol Motil. 2010;16(3):232–242. | ||
Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol. 2013;108(8):1238–1249; quiz 1250. | ||
Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005;100(6):1404–1414. | ||
Chan SM, Chiu PW, Wu JC, et al. Laparoscopic Heller’s cardiomyotomy achieved lesser recurrent dysphagia with better quality of life when compared with endoscopic balloon dilatation for treatment of achalasia. Dis Esophagus. 2013;26(3):231–236. | ||
Kostic S, Kjellin A, Ruth M, et al. Pneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia. Results of a randomized controlled trial. World J Surg. 2007;31(3):470–478. | ||
Marlais M, Fishman J, Fell J, Rawat D, Haddad M. Reduced health-related quality of life in children with achalasia. Arch Dis Child. 2010;95 (Suppl 1):A53. | ||
Moonen AJ, Boeckxstaens GE. Management of achalasia. Gastroenterol Clin North Am. 2013;42(1):45–55. | ||
Mikaeli J, Fazel A, Montazeri G, Yaghoobi M, Malekzadeh R. Randomized controlled trial comparing botulinum toxin injection to pneumatic dilatation for the treatment of achalasia. Aliment Pharmacol Ther. 2001;15(9):1389–1396. | ||
Bansal R, Nostrant TT, Scheiman JM, et al. Intrasphincteric botulinum toxin versus pneumatic balloon dilation for treatment of primary achalasia. J Clin Gastroenterol. 2003;36(3):209–214. | ||
Zaninotto G, Annese V, Costantini M, et al. Randomized controlled trial of botulinum toxin versus laparoscopic Heller myotomy for esophageal achalasia. Ann Surg. 2004;239(3):364–370. | ||
Beck WC, Sharp KW. Achalasia. Surg Clin North Am. 2011;91(5):1031–1037. | ||
Krill JT, Naik RD, Vaezi MF. Clinical management of achalasia: current state of the art. Clin Exp Gastroenterol. 2016;9:71–82. | ||
Zhao JG, Li YD, Cheng YS, et al. Long-term safety and outcome of a temporary self-expanding metallic stent for achalasia: a prospective study with a 13-year single-center experience. Eur Radiol. 2009;19(8):1973–1980. | ||
Cheng YS, Ma F, Li YD, et al. Temporary self-expanding metallic stents for achalasia: a prospective study with a long-term follow-up. World J Gastroenterol. 2010;16(40):5111–5117. | ||
Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42(4):265–271. | ||
von Renteln D, Inoue H, Minami H, et al. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol. 2012;107(3):411–417. | ||
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg. 2014;259(6):1098–1103. | ||
Li YD, Tang GY, Cheng YS, Chen NW, Chen WX, Zhao JG. 13-Year follow-up of a prospective comparison of the long-term clinical efficacy of temporary self-expanding metallic stents and pneumatic dilatation for the treatment of achalasia in 120 patients. AJR Am J Roentgenol. 2010;195(6):1429–1437. | ||
Moretó M, Ojembarrena E, Barturen A, Casado I. Treatment of achalasia by injection of sclerosant substances: a long-term report. Dig Dis Sci. 2013;58(3):788–796. | ||
Niknam R, Mikaeli J, Fazlollahi N, et al. Ethanolamine oleate as a novel therapy is effective in resistant idiopathic achalasia. Dis Esophagus. 2014;27(7):611–616. | ||
Boeckxstaens GE, Annese V, des Varannes SB, et al; European Achalasia Trial Investigators. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364(19):1807–1816. | ||
Novais PA, Lemme EM. 24-h pH monitoring patterns and clinical response after achalasia treatment with pneumatic dilation or laparoscopic Heller myotomy. Aliment Pharmacol Ther. 2010;32(10):1257–1265 | ||
Hamdy E, El Nakeeb A, El Hanfy E, et al. Comparative study between laparoscopic Heller myotomy versus pneumatic dilatation for treatment of early achalasia: a prospective randomized study. J Laparoendosc Adv Surg Tech A. 2015;25(6):460–464. | ||
Persson J, Johnsson E, Kostic S, Lundell L, Smedh U. Treatment of achalasia with laparoscopic myotomy or pneumatic dilatation: long-term results of a prospective, randomized study. World J Surg. 2015;39(3):713–720. | ||
Moonen A, Annese V, Belmans A, et al. Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut. 2016;65(5):732–739. | ||
Chrystoja CC, Darling GE, Diamant NE, et al. Achalasia-specific quality of life after pneumatic dilation or laparoscopic Heller myotomy with partial fundoplication: a multicenter, randomized clinical trial. Am J Gastroenterol. 2016;111(11):1536–1545. | ||
Campos GM, Vittinghoff E, Rabl C, et al. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg. 2009;249(1):45–57. | ||
Yaghoobi M, Mayrand S, Martel M, Roshan-Afshar I, Bijarchi R, Barkun A. Laparoscopic Heller’s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc. 2013;78(3):468–475. | ||
Beller EM, Glasziou PP, Altman DG, et al; PRISMA for Abstracts Group. PRISMA for Abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med. 2013;10(4):e1001419. | ||
Verhagen AP, de Vet HC, de Bie RA, et al. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51(12):1235–1241. | ||
Clark AG, Rogers KM. Dependence upon bile volume of the biliary excretion of bromocresol green and amaranth in the anaesthetized rat. Aust J Biol Sci. 1975;28(4):339–351. | ||
Eckardt VF, Stauf B, Bernhard G. Chest pain in achalasia: patient characteristics and clinical course. Gastroenterology. 1999;116(6):1300–1304. | ||
Vantrappen G, Hellemans J. Treatment of achalasia and related motor disorders. Gastroenterology. 1980;79(1):144–154. | ||
Borges AA, Lemme EM, Abrahao LJ Jr, et al. Pneumatic dilation versus laparoscopic Heller myotomy for the treatment of achalasia: variables related to a good response. Dis Esophagus. 2014;27(1):18–23. | ||
Lake JM, Wong RK. Review article: the management of achalasia – a comparison of different treatment modalities. Aliment Pharmacol Ther. 2006;24(6):909–918. | ||
Lopushinsky SR, Urbach DR. Pneumatic dilatation and surgical myotomy for achalasia. JAMA. 2006;296(18):2227–2233. | ||
West RL, Hirsch DP, Bartelsman JF, et al. Long term results of pneumatic dilation in achalasia followed for more than 5 years. Am J Gastroenterol. 2002;97(6):1346–1351. | ||
Zerbib F, Thétiot V, Richy F, Benajah DA, Message L, Lamouliatte H. Repeated pneumatic dilations as long-term maintenance therapy for esophageal achalasia. Am J Gastroenterol. 2006;101(4):692–697. | ||
Bravi I, Nicita MT, Duca P, et al. A pneumatic dilation strategy in achalasia: prospective outcome and effects on oesophageal motor function in the long term. Aliment Pharmacol Ther. 2010;31(6):658–665. | ||
Hulselmans M, Vanuytsel T, Degreef T, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Clin Gastroenterol Hepatol. 2010;8(1):30–35. | ||
Morino M, Rebecchi F, Festa V, Garrone C. Preoperative pneumatic dilatation represents a risk factor for laparoscopic Heller myotomy. Surg Endosc. 1997;11(4):359–361. | ||
Schoenberg MB, Marx S, Kersten JF, et al. Laparoscopic Heller myotomy versus endoscopic balloon dilatation for the treatment of achalasia: a network meta-analysis. Ann Surg. 2013;258(6):943–952. | ||
Moonen A, Boeckxstaens G. Finding the right treatment for achalasia treatment: risks, efficacy, complications. Curr Treat Options Gastroenterol. 2016;14(4):420–428. | ||
Jacobs J, Richter JE. Opening the bird’s beak: tips and tricks for effective pneumatic dilation for achalasia. Am J Gastroenterol. 2016;111(2):157–158. | ||
Borhan-Manesh F, Kaviani MJ, Taghavi AR. The efficacy of balloon dilation in achalasia is the result of stretching of the lower esophageal sphincter, not muscular disruption. Dis Esophagus. 2016;29(3):262–266. | ||
Youn YH, Minami H, Chiu PW, Park H. Peroral endoscopic myotomy for treating achalasia and esophageal motility disorders. J Neurogastroenterol Motil. 2016;22(1):14–24. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

