Back to Journals » Journal of Pain Research » Volume 8
Landmark-based versus ultrasound-guided ilioinguinal/iliohypogastric nerve blocks in the treatment of chronic postherniorrhaphy groin pain: a retrospective study
Authors Trainor D, Moeschler S , Pingree M , Hoelzer B, Wang Z , Mauck W, Qu W
Received 17 April 2015
Accepted for publication 26 June 2015
Published 23 October 2015 Volume 2015:8 Pages 767—770
DOI https://doi.org/10.2147/JPR.S86777
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Michael Schatman
Drew Trainor,1 Susan Moeschler,2 Matthew Pingree,1,2 Brian Hoelzer,2 Zhen Wang,2 William Mauck,2 Wenchun Qu1,2
1Department of Physical Medicine and Rehabilitation, 2Department of Anesthesiology, Division of Pain Medicine, Mayo Clinic, Rochester, MN, USA
Background: Chronic postherniorrhaphy groin pain (CPGP) is a debilitating condition, which is often refractory to conservative medical management. To our knowledge, there have been no studies directly comparing landmarked-based and ultrasound-guided approaches in this population.
Objective: To compare the effectiveness of landmark-based and ultrasound-guided ilioinguinal/iliohypogastric nerve blocks in the treatment of CPGP.
Study design: This is a retrospective chart review of patients who presented to our tertiary care pain medicine clinic with a diagnosis of CPGP. Inclusion criteria were the following: age >18 years, diagnosis of groin pain, and prior history of herniorrhaphy. Exclusion criteria included those who were seen for initial consultation but were lost to follow-up. Primary outcomes were 50% or greater reduction in pain on visual analog scale (VAS). Secondary outcomes were 30% or greater reduction in VAS pain score, changes in VAS pain scores, and reported complications.
Results: A total of 36 patients were included in the study. Of them, 20 patients underwent the landmark-based and 16 underwent the ultrasound-guided techniques. There was no significant difference in baseline demographics. The average VAS score preinjection was 7.08 in the landmark-based and 7.0 in the ultrasound-guided groups (P=0.65). A total of 14 patients (70%) in the landmark-based and eleven patients (79%) in the ultrasound-guided groups experienced at least a 50% reduction in VAS scores. There was no statistically significant difference between the two groups (P=1.0), and no complications were noted. We also did not find a significant difference in terms of number of patients with 30% or greater reduction (P=0.71) and changes in VAS pain scores (P=0.64). No complications were reported in either group.
Conclusion: In our study, there was no statistically significant difference between the landmark-based and ultrasound-guided groups in terms of a reduction in VAS pain scores, and no complications were noted in either group.
Keywords: abdominal wall, intramuscular injections, ultrasound, anatomic landmarks
Introduction
Chronic postherniorrhaphy groin pain (CPGP) is a common and debilitating condition that occurs with a prevalence of 15%–53%.1 While no specific guidelines exist in the treatment of CPGP, according to the European Federation of Neurological Societies (EFNS), the treatment of “traumatic and postsurgical neuropathic pain” includes medical management and the use of neuropathic pain medications such as gabapentin and tricyclic antidepressants.2 When these medications do not provide adequate reduction in pain, other more invasive therapeutic interventions may be indicated. Ilioinguinal/iliohypogastric nerve blocks (IINBs) with local anesthetic and corticosteroid can be effective in treating CPGP refractory to medical management.3 The two most common approaches for performing IINBs are the landmark-based and ultrasound-guided techniques. In the acute setting, studies have shown that using ultrasound provides more effective analgesia and higher satisfaction of analgesia compared to the landmark-based technique,4 but to our knowledge, there have been no studies directly comparing landmark-based versus ultrasound-guided nerve blocks in the chronic groin pain population.
Study design
After obtaining approval from the Mayo Clinic Institutional Review Board (IRB), we performed a retrospective chart review to identify patients who presented to our tertiary care outpatient pain medicine clinic from November 2001 to November 2011 with a diagnosis of postherniorrhaphy groin pain. Obtaining written informed consent for this study was unnecessary, as the study involved the retrospective review of patients’ data. Using the Mayo Clinic Life Sciences System Data Discovery and Query Builder, we searched for the text phrases “inguinal pain”, “groin pain”, and “postherniorrhaphy pain” mentioned in the outpatient pain medicine clinic notes within the electronic medical record during that time period. Our initial search returned 1,090 unique medical record numbers that met our inclusion criteria of age >18 years, diagnosis of groin pain, and prior history of herniorrhaphy. We then performed a second data query to exclude those patients who were seen for initial consultation but were lost to follow-up, which reduced the number of unique medical record numbers to 428. Following the second data query, we executed a manual chart review to identify the patients who failed standard medical therapy and eventually underwent either landmark-based or ultrasound-guided IINBs as definitive therapy. Using the Microsoft Access database management system, we recorded patient demographics, pre- and postinjection visual analog scale (VAS) pain scores, and use of surgical mesh.
The primary outcome of interest was the number of patients with 50% or greater reduction in VAS pain score. The secondary outcomes were 30% or greater reduction in VAS pain score, changes in VAS pain scores, and reported complications (colonic/small bowel puncture, damage to vascular structures, or femoral nerve block). Due to the small number of patients included in this study, we conducted univariate analyses by comparing patient demographics and outcomes between two interventions. Nonparametric Mann–Whitney U tests were used for continuous variables and chi-square tests, and Fisher’s exact tests (n≤5) for dichotomized variables. All statistical analyses were conducted using STATA version 13.1 (StataCorp, College Station, TX, USA).
Results
A total of 36 patients were included in the study. Of them, 20 patients underwent landmark-based injections, and 16 patients were treated with ultrasound-guided injections. There was no significant difference between the two groups in age, sex, obesity, opioid use, number of surgeries, and use of surgical mesh (Table 1). The initial VAS pain scores were 7.08 for the landmark-based injection group and 7.00 for the ultrasound-guided injections group (P=0.65).
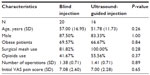  | Table 1 Patient baseline characteristics by group |
A total of 14 patients (70%) in the blind injections group experienced at least 50% reduction in pain, compared to eleven patients (79%) in the ultrasound-guided injections group (Table 2). There was no statistically significant difference between the two groups (P=1.00). We also did not find significant difference in terms of number of patients with 30% or greater reduction (P=0.71) and changes in VAS pain scores (P=0.64). No complications were reported in either group.
  | Table 2 Comparisons of VAS pain scores by group |
Discussion
The ilioinguinal and iliohypogastric nerves are the implicated structures in CPGP. Both arise from the anterior division of the first lumbar vertebrae; course anterior to the psoas, quadratus lumborum, and iliacus; and pierce the transversus abdominis near the anterior portion of the iliac crest. The ilioinguinal nerve then pierces the internal oblique muscle and accompanies the spermatic cord through the superficial inguinal ring, while the anterior division of the iliohypogastric nerve pierces the obliquus internus and externus above the superficial inguinal ring and provides sensation to the skin of the pubic region. The proximity of these structures to the inguinal region makes them susceptible to injury during herniorrhaphy repair and can lead to chronic pain in a significant percentage of this population.1 While the mechanism of postherniorrhaphy neuropathic groin pain has not been defined, several theories exist and include direct intraoperative nerve injury, tension on the ilioinguinal and iliohypogastric nerves created by postsurgical changes, and an inflammatory reaction to implanted mesh.5 Moreover, the independent risk factors for the development of CPGP included younger age (<40 years), body mass index greater than 25 kg/m2, and the use of a surgical propylene radomesh.6 In patients affected by this debilitating condition, IINBs are a reasonable option for treatment in those who have failed conservative medical management.3
Landmark-based IINBs have reported failure rates of 10%–25% in the literature.7 According to Golfeld et al,8 this may be due to anatomic variations in the ilioinguinal and iliohypogastric nerves, with only 41.8% of patients having nerves that course in the manner described in anatomy texts. In the landmark-based technique, the needle is inserted 2 cm medial and 2 cm superior to the anterior superior iliac spine. An initial pop sensation is felt as the needle penetrates the external oblique aponeurosis, and approximately one half of the local anesthetic and corticosteroid is injected at this location. The needle is then advanced deeper where a second pop is felt when the aponeurosis of the internal oblique is punctured and the bevel of the needle lies in the fascial plane between the internal oblique and transversus abdominis. This is commonly referred to as the transversus abdominis plane (TAP) and is the region where the ilioinguinal and iliohypogastric nerves are located. The remainder of the local anesthetic and corticosteroid is injected in this fascial plane. Commonly, a total volume of 10 mL or greater is injected.7 The use of this technique requires an experienced proceduralist with excellent palpatory skills to appreciate the pop as the needle moves through the aponeurosis of the external and internal obliques to ensure that the medication is injected in the proper fascial plane and that the risk of complications is minimized. Multiple complications have been reported using the landmark-based technique. These include colonic or small bowel puncture,9,10 damage to vascular structures resulting in hematoma,11 and inadvertent femoral nerve block. The latter can result in lower extremity weakness, and increased fall risk, requiring prolonged recoveries in the postprocedure suite.12
In contrast, with ultrasound training, the proceduralist can guide the needle to the TAP and visualize the flow of medication in real time, theoretically providing more consistent and accurate delivery of the medication, although this did not impact the outcomes of this study. Using this technique, a high-frequency linear probe is placed in an oblique orientation along a line connecting the anterior superior iliac spine and the umbilicus. Then, using sonographic guidance, the needle is advanced into the TAP where the ilioinguinal and iliohypogastric nerves are visualized and the local anesthetic and corticosteroid are subsequently injected (Figure 1). Given more accurate needle placement, smaller volumes of injectate are used in the ultrasound-guided technique (3–4 mL compared to 10 mL or greater with the landmark-based approach).8,13 In some circumstances, it may not be possible to directly visualize the nerves in the TAP. In this situation, Doppler testing can be helpful in identifying the branch of the deep circumflex artery, which lies in the same plane and runs parallel to the ilioinguinal nerve.8
Due to the small number of participants in this study, there were no significant differences in pain reduction when comparing the landmark-based and ultrasound-guided techniques. Nevertheless, direct visualization of the nerves, arteries, and TAP by ultrasound may lead to a more precise injection and may be the reason for improvement in a larger percentage of patients in the ultrasound-guided group. There may be a trend toward significance, but with our small patient numbers, no statically significant difference was appreciated. Similarly, direct visualization of the needle with ultrasound guidance may help to minimize the risk of complications when compared to the landmark-based technique. Yet, this study is too small to make that statement given the lack of complications in both groups. As complications related to this procedure are rare, large numbers of patients would be required to detect a significant difference in complications.
Conclusion
Our study did not show a statistically significant difference in pain reduction when comparing landmark-based and ultrasound-guided IINBs. No complications were noted in either group. However, this was a retrospective study with small patient numbers. Larger prospective studies are needed to investigate whether there is a difference in efficacy and risk between these two methods for the treatment of CPGP.
Disclosure
The authors report no conflicts of interest in this work.
References
Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA. A review of chronic pain after inguinal herniorrhaphy. Clin J Pain. 2003;19:48–54. | |
Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17:1113–e88. | |
Thomassen I, van Suijlekom JA, van de Gaag A, Ponten JE, Nienhuijs SW. Ultrasound-guided ilioinguinal/iliohypogastric nerve blocks for chronic pain after inguinal hernia repair. Hernia. 2013;17:329–332. | |
Demirci A, Efe EM, Turker G, et al. Iliohypogastric/ilioinguinal nerve block in inguinal hernia repair for postoperative pain management: comparison of the anatomical landmark and ultrasound guided techniques. Braz J Anesthesiol. 2014;64:350–356. | |
Song XJ, Vizcarra C, Xu DS, Rupert RL, Wong ZN. Hyperalgesia and neural excitability following injuries to central and peripheral branches of axons and somata of dorsal root ganglion neurons. J Neurophysiol. 2003;89:2185–2193. | |
Massaron S, Bona S, Fumagalli U, Battafarano F, Elmore U, Rosati R. Analysis of postsurgical pain after inguinal hernia repair: a prospective study of 1,440 operations. Hernia. 2007;11:517–525. | |
van Schoor AN, Boon JM, Bosenberg AT, Abrahams PH, Meiring JH. Anatomical considerations of the pediatric ilioinguinal/iliohypogastric nerve block. Paediatr Anaesth. 2005;15:371–377. | |
Gofeld M, Christakis M. Sonographically guided ilioinguinal nerve block. J Ultrasound Med. 2006;25:1571–1575. | |
Johr M, Sossai R. Colonic puncture during ilioinguinal nerve block in a child. Anesth Analg. 1999;88:1051–1152. | |
Amory C, Mariscal A, Guyot E, Chauvet P, Leon A, Poli-Merol ML. Is ilioinguinal/iliohypogastric nerve block always totally safe in children? Paediatr Anaesth. 2003;13:164–166. | |
Vaisman J. Pelvic hematoma after an ilioinguinal nerve block for orchialgia. Anesth Analg. 2001;92:1048–1049. | |
Tsai TY, Huang YS, Tsai YC, Liu YC. Temporary femoral nerve palsy after ilioinguinal nerve blockade combined with splash block for post-inguinal herniorrhaphy analgesia in a pediatric patient. Acta Anaesthesiol Taiwan. 2007;45:237–240. | |
Urigel S, Molter J. Transversus abdominis plane (TAP) blocks. AANA J. 2014;82:73–79. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

