Back to Journals » Patient Preference and Adherence » Volume 12
Lack of coordination between partners: investigation of Physician-Preferred and Patient-Preferred (4P) basal insulin titration algorithms in the real world
Authors Zhang T, Zhao Y , Du T, Zhang X , Li X, Liu R, Wang Y, Chen B, He L, Li W
Received 22 March 2018
Accepted for publication 13 May 2018
Published 18 July 2018 Volume 2018:12 Pages 1253—1259
DOI https://doi.org/10.2147/PPA.S169000
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Tong Zhang,1 Yunjuan Zhao,2 Tao Du,2 Xiaodan Zhang,2 Xiaowei Li,2 Ruike Liu,3 Yunlin Wang,4 Bo Chen,5 Ling He,6 Wangen Li2
1Department of Endocrinology, The Third Affiliated Hospital, Southern Medical University, Guangzhou 510630, People’s Republic of China; 2Department of Endocrinology, The Second Affiliated Hospital, Guangzhou Medical University, Guangzhou 510260, People’s Republic of China; 3Department of Endocrinology, The Third People’s Hospital of Dongguan, Dongguan 523326, People’s Republic of China; 4Department of Endocrinology, Foshan Hospital, Southern Medical University, Foshan 528000, People’s Republic of China; 5Department of Endocrinology, Guangdong Second Provincial General Hospital, Guangzhou 510317, People’s Republic of China; 6Department of Endocrinology, Guangzhou First People’s Hospital, Guangzhou 510180, People’s Republic of China
Background: Patient-centered care is respectful to a patient’s preference. All prior clinical trials on patient self-titration algorithms for basal insulin were decided by physicians. We hypothesized that patients and physicians have different preferences.
Patients and methods: Physicians and diabetes patients were asked to choose their preferred insulin glargine self-titration algorithm among 5 algorithms. Algorithm 1, 1 U increase once daily; algorithm 2, 2 U increase every 3 days; algorithm 3, 3 U increase every 3 days; algorithm 4, titration every 3 days according to fasting blood glucose, and algorithm 5, weekly titration 2–8 U based on 3-day mean fasting blood glucose levels.
Results: Eleven (5.2%) out of 210 physicians and 180 (90.9%) out of 198 patients preferred algorithm 1 (χ2=300.4, p=0.000). In contrast, 195 (92.9%) physicians and 18 (9.1%) patients preferred algorithm 2 (χ2=286.6, p=0.000). In addition, 4 (1.9%) physicians but no patients preferred algorithm 3 (χ2=2.099, p=0.124). Neither physicians nor patients chose algorithms 4 or 5. Most physicians preferred algorithm 2 since it is recommended by guidelines, but most patients preferred algorithm 1 for its simplicity.
Conclusion: Patients had different preferences compared with physicians. Attention should be given to patients’ preferences to increase adherence and improve glycemic control.
Keywords: type 2 diabetes, titration algorithm, insulin glargine, basal insulin, self-adjustment, shared decision-making, adherence
Introduction
The initiation of basal insulin, as add-on therapy in patients with type 2 diabetes who fail to reach their glycated hemoglobin (HbA1c) target using oral antidiabetic drugs (OADs), is recommended by current guidelines.1,2 Adequate titration of insulin doses is required in order to achieve optimal glycemic control.3 However, many physicians and patients hesitate to titrate insulin dose in the real world. The First Basal Insulin Evaluation Asia study showed that the prescribed mean daily insulin dose increased marginally from 0.20 U/kg/d at initiation to 0.22–0.24 U/kg/d at 6 months.4 The recently published ORBIT study investigating real-life use of basal insulin in patients with uncontrolled type 2 diabetes with OADs showed that the initial dose was 0.18 U/kg and was followed by a mean increase of daily dose of only 0.03 U/kg after 6 months.5 Additionally, only 56.6% of insulin users reported insulin titration at 6 months.5
To ensure adequate titration of insulin doses, Yki-Järvinen et al6 recommended self-adjustment of insulin dose based on home glucose monitoring in 1997. Thereafter, numerous randomized controlled trials using a basal insulin titration algorithm showed that patients with type 2 diabetes can be effectively and safely involved in insulin titration.7–11
However, prior patient self-titration algorithms for basal insulin used in clinical trials were decided by physicians,7–11 which may lead to poor adherence due to neglecting patient preferences. According to the position of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) on patient-centered approach, physicians and patients act as partners, mutually exchanging information and deliberating on options in order to reach a consensus on the therapeutic course of action.12 Importantly, engaging patients in medical decisions may enhance adherence to therapy.12
Numerous basal insulin titration algorithms have been demonstrated to be effective and safe in randomized clinical trials, which can be chosen by patients and physicians.1,2,7–10 We hypothesized that patients have different preferences than physicians for basal insulin titration algorithms. Thus, the aim of this study was to investigate the differences between physicians’ and patients’ preferences for basal insulin titration algorithms and to assess adherence, efficacy, and safety of patient-preferred algorithms.
Patients and methods
Research design and participants
This study comprised of 2 parts – a physician survey and an observational prospective study involving patients.
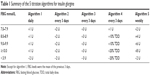
The physician survey was conducted between August 2016 and December 2016, and involved face-to-face interviews. All participating physicians were from 10 secondary and 10 tertiary hospitals, and had >2 years of experience in prescribing basal insulin. All participating physicians were asked to choose among 5 predefined insulin self-titration algorithms and list reasons spontaneously for their choices. The 5 candidate algorithms were: 1) a daily increase of 1 U (INSIGHT study algorithm);9 2) titration with 2 U every 3 days (AT.LANTUS study algorithm, ADA, EASD, American Association of Clinical Endocrinologists [AACE], and American College of Endocrinology [ACE] recommendations);1,2,8 3) titration with 3 U every 3 days (PREDICTIVE 303 study algorithm);10,13 4) increase insulin dose every 3 days based on fasting blood glucose (FBG) as follows: if FBG value is 7.0–7.9 mmol/L, increase insulin dose by 1 U; if FBG value is 8.0–9.9 mmol/L, increase insulin dose by 10% of total daily dose; if FBG values ≥10 mmol/L, increase insulin dose by 20% of total daily dose (AACE and ACE recommendation);2 and 5) a weekly increase of 2–8 U based on the mean of 3 FBG values (Table 1).7,8,14–17
The clinical study involving patients was conducted between January 2016 and February 2017. Type 2 diabetes patients, aged 18–75 years, who failed to reach their HbA1c and FBG targets (<7.0% and 7.0 mmol/L, respectively) using OADs and were recommended to initiate insulin therapy with glargine as add-on to existing OADs were invited to participate and followed up until they reached their FBG target for 3 consecutive days. All patients were asked to visit their treating physicians in the month when their FBG reached the target (second and final study visit). Adherence, efficacy, and safety were recorded during this visit. Exclusion criteria were history of ketoacidosis, noncompliance with daily measurement of FBG, any intention to add additional OADs during study participation, changes in OAD dose at study enrollment, alanine aminotransferase and aspartate aminotransferase >3 times the upper normal limit, serum creatinine ≥120 μmol/L, pregnancy, or use of drugs likely to interfere with glucose control.
The education on insulin administration and FBG monitoring was given according to the local practice of each institution. Patients were provided the insulin titration algorithms presented to physicians, and after detailed explanation of each algorithm, patients were asked to choose a “preferred” insulin titration algorithm to be used during the study and also list reasons spontaneously for their choices. All patients were instructed to start insulin glargine (Lantus®; Aventis Pharma, Strasbourg, France) at an initial dose of 0.2 U/kg and to inject it at the same time each evening (between 21.00 and 22.00 h). Doses were to be self-titrated according to patients’ preferred algorithm and reduced if biochemical or clinical hypoglycemia occurred. During the study, the patients were not allowed to switch from one algorithm to another.
The study was conducted in accordance with the Declaration of Helsinki. Approval was obtained from the institutional ethics committees of the Third Affiliated Hospital of Southern Medical University, the academic ethics review boards of the Second Affiliated Hospital of Guangzhou Medical University, the ethics committees of the Third People’s Hospital of Dongguan, the institutional ethics committees of Foshan Hospital of Southern Medical University, the ethics committees of Guangdong Second Provincial General Hospital, and the ethics committees of Guangzhou First People’s Hospital. All patients provided written informed consent before participation
Preferences, adherence, efficacy, and safety measures
The primary objective of this study was to assess physicians’ and patients’ preferences for the 5 proposed insulin self-titration algorithms.
The secondary objectives included an assessment of adherence, efficacy, and safety of patients’ preferred insulin titration algorithms in reaching FBG levels <7.0 mmol/L. A patient was considered to reach the efficacy target if FBG level was <7 mmol/L on 3 consecutive days, and the first day of the 3 consecutive days was recorded as the date when glucose target was met and the study ended for the patient.
Evaluation of safety included assessment of the proportion of patients who experienced hypoglycemic episodes during the study period. Hypoglycemic episodes were defined as symptoms suggestive of hypoglycemia plus a documented blood glucose level <3.9 mmol/L. Severe hypoglycemia was defined as an episode with symptoms consistent with hypoglycemia during which the patient required the assistance of another person.
Statistical analyses
Significance of differences between patients and physicians was analyzed using the Pearson’s χ2 and Fisher’s exact tests or Student’s t-test. Results are expressed as mean ± SD. Statistical analysis was performed using SPSS Statistical Software 19.0 (IBM Corporation, Armonk, NY, USA), and statistical testing was set at a significance level of α=0.05.
Results
Difference between physicians’ and patients’ preferred algorithms
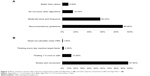
A total of 210 out of 215 screened physicians were willing to receive our survey and 198 out of 230 screened patients were willing to self-titrate their insulin and were included in the analysis of preference of insulin titration algorithms. Eleven (5.2%) out of 210 physicians and 180 (90.9%) out of 198 patients preferred algorithm 1 (χ2=300.4, p=0.000). In contrast, 195 (92.9%) physicians and 18 (9.1%) patients preferred algorithm 2 (χ2=286.6, p=0.000). In addition, 4 (1.9%) physicians but no patients preferred algorithm 3 (χ2=2.099, p=0.124). Neither physicians nor patients chose algorithms 4 or 5 (Figure 1).
The reasons reported by physicians for choosing algorithm 2 included recommendation by several guidelines, moderation in the titration of insulin dose and frequency of insulin titration, lack of knowledge of other algorithms, or higher efficacy of the algorithm in decreasing glucose values (better than others). For patients, reasons for choosing algorithm 1 included its simplicity, the perception that titrating insulin by 1 U is safe, titrating every day may enable them to reach the target faster, and no requirement to calculate mean FBG (Figure 2).
Adherence to the algorithms preferred by patients
Ten out of 180 patients using algorithm 1 and 2 out of 18 patients using algorithm 2 were lost to follow-up, and thus not included in the adherence, efficacy, and safety analyses. The baseline characteristics of the patients in the 2 study groups (algorithms 1 and 2) are listed in Table 2. A total of 165 (97.1%) patients who preferred algorithm 1 and 13 (81.2%) patients who preferred algorithm 2 titrated their insulin glargine dose according to the algorithm (χ2=5.454, p=0.023).
Efficacy and safety analyses of the algorithms preferred by patients
FBG reduced from 9.8±1.2 to 6.2±0.5 mmol/L (t=30.793, p=0.000) for algorithm 1 and from 10.1±1.5 to 6.1±0.8 mmol/L for algorithm 2 (t=11.346, p=0.000), respectively. Hypoglycemia was reported in only 1 patient who used algorithm 2, and this patient reported titrating insulin dose with 2 U daily instead of every 3 days.
FBG target was reached in 8.0±4.3 days in patients using algorithm 1 and in 10.8±5.5 days in those using algorithm 2. Mean insulin glargine dose when FBG target was reached was 20.4±4.4 U (0.35±0.09 U/kg) in those using algorithm 1 and 21.7±4.2 U (0.33±0.06 U/kg) in those using algorithm 2.
Discussion
The most frequently used self-titration algorithm for insulin glargine in clinical trials was increasing the does by 2 U every 3 days, until FBG reached the desired target. This was used for the first time in the AT.LANTUS study, and was incorporated in ADA, EASD, and AACE guidelines.1,7,18 In line with these guidelines, the physicians in this study also preferred the AT.LANTUS algorithm (algorithm 2). However, patients preferred the self-titration algorithm for insulin glargine employing 1 U daily increase (algorithm 1), and which was used for the first time in the INSIGHT study.8 Algorithms 4 and 5, which were recommended by AACE and ACE,2 and used in many clinical trials,7,8,14–17 were neither preferred by our physicians nor patients.
The most important reason for patients’ preference was the simplicity of the INSIGHT titration algorithm. This confirms previous observations that complexity of titration algorithms is one of the main barriers in patients’ acceptance of insulin titration.19,20 A simple titration algorithm can offer several benefits, including fewer clinic visits for insulin dose adjustment, permitting timely increase in insulin dose and patients becoming comfortable in managing their insulin dose.21 This facilitates empowerment of patients in the management of diabetes and a higher flexibility of the therapy.21 All these advantages may provide adherence benefits as compared to more complex algorithms. Indeed, in our study, the adherence to self-titration algorithms was as high as 97.1% in the algorithm 1 group and 81.2% in the algorithm 2 group, and was achieved without increasing the consumption of resources commonly used when initiating insulin in patients with type 2 diabetes. Only standard education on insulin administration and FBG and a short explanation and instructions on the preferred self-titration algorithm were provided.
Not only patients but also physicians preferred the relatively simple algorithm. One study showed that if 40 physicians increased fixed dose of 2 U every 3 days, only 1 physician selected a glucose-based titration algorithm of increasing 4 U every 3 days if glucose value was >10 mmol/L and 2 U if glucose value was ≤10 mmol/L.22
In this study, the patients achieved FBG target and had significant reduction within 8–10 days, according to the algorithm used. The time to achieve FBG targets in our study was similar to Pfutzner et al’s study,22 which used the AT.LANTUS algorithm. In their study, 70% of patients achieved a stable insulin glargine dose and FBG within a preset target after a mean of 5±6 days following study enrollment.22 However, they also had daily physician contact via phone and the dose was based on physician’s decision on insulin dose titration.22 In contrast, the time to achieve similar FBG endpoints in many trials was 12–24 weeks.7–9,11,24 This indicated the adherence of our patients to self-preferred algorithms. Another reason is that most of our patients used sulfonylureas, which shortens the FBG target achievement time.23
Hypoglycemia events rarely occurred in both groups in this study perhaps because our FBG target was 7.0 as compared to 5.1–6.1 mmol/L in previous trials.7–10,14–17,25–28
We chose FBG <7.0 mmol/L as efficacy measurement and treatment target and not HbA1c due to several reasons. First, basal insulin is titrated based on FBG levels.1,2 Additionally, patients understand FBG better than HbA1c. Moreover, the majority of randomized clinical trials with basal insulin did not reach their FBG targets of ≤5,13 ≤5.5,5–7 or ≤6.1 mmol/L,10,11,13 and an increased incidence of severe hypoglycemic events was observed and confirmed at FBG values <5.5 mmol/L.29 One study also showed that aggressive titration did not result in better HbA1c values.30 The ADA/EASD position statement states that a FBG level <7.2 mmol/L is sufficient to reach the recommended HbA1c target of <7%.12
We tested whether a higher target could be achieved in real-life conditions. Observational studies of patients in real-life settings, outside of the highly controlled randomized clinical trials, showed that at 3 months after insulin initiation, mean FBG of 7.3–7.4 mmol/L was reached31 and physicians usually preferred glycemic target of 7.2 rather than 5.5 mmol/L22 in daily practice, which was in line with ADA and EASD position statement (<7.2 mmol/L).1
Interestingly, previous trials with an FBG target of 5.1–6.1 mmol/L7–10,14–17,25–28 attained an endpoint FBG of 6.3–7.6 mmol/L, while we set a higher FBG target of 7.0 mmol/L but attained a lower endpoint FBG of 6.1–6.2 mmol/L. This is in agreement with a global survey which found that physicians would be more aggressive in treating diabetes if there was no concern about hypoglycemia.6
In the present study, a glargine dose of 0.33–0.35 U/kg was required to achieve the FBG target. This dose was lower as compared to that in western populations,7,9,13,24 perhaps due to 2 reasons. First, >80% of our patients also took combined sulfonylureas, which could save insulin glargine dose for enhancing endogenous insulin secretion.32 In the INSIGHT trial, 35.4% of patients used sulfonylureas, combined with 0.41 U/kg and attained an FBG target 6.7 mmol/L. Second, Asian patients with type 2 diabetes may have lower insulin resistance33 and lower insulin needs as compared to non-Asian populations. In contrast, in the Treat-to-Target study of North American patients with type 2 diabetes, the mean FBG was 6.5 mmol/L over 6 months with insulin glargine doses of 0.48 U/kg.7
Limitations
There are several limitations to this study. First, because patients preferring algorithm 1 were more in number compared to those preferring algorithm 2, the power in comparing the efficacy and safety of the 2 patient-preferred algorithms is limited. Second, whether the patient-preferred algorithm is superior to physician-preferred algorithm in clinical practice needs to be further clarified using a randomized trial. Last, our research was a short-term observation based on FBG, so the question of whether patient-preferred algorithm has a long-term advantage based on HbA1c needs further study.
Conclusion
This study showed that even in real-life settings, patients with type 2 diabetes inadequately controlled with OADs, who were recommended insulin initiation, preferred different algorithms as compared to the physicians. Most patients preferred 1 U insulin glargine increase once daily for its simplicity. A simple algorithm had higher adherence, resulted in adequate titration of insulin doses, and was efficient and safe in decreasing FBG. Hence, attention should be given to patients’ preferences in self-titration algorithms.
Data sharing statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
This work was supported by the Health and Family Planning Commission of Guangzhou Municipality (grant number: 20171A011301) and Science and Technology project of Guangzhou (grant numbers: 201707010365 and 201707010045).
Author contributions
Wangen Li contributed to the design of the study, data analysis, and manuscript preparation and overviewing. Other coauthors participated in the patient recruitment, implementation of the study, safety monitoring, and manuscript overviewing. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–149. | ||
Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm – 2016 executive summary. Endocr Pract. 2016;22(1):84–113. | ||
Garber AJ. The importance of titrating starting insulin regimens in patients with type 2 diabetes. Diabetes Obes Metab. 2009;11(Suppl 5):10–13. | ||
Tsai ST, Pathan F, Ji L, et al. First insulinization with basal insulin in patients with type 2 diabetes in a real-world setting in Asia. J Diabetes. 2011;3(3):208–216. | ||
Ji L, Zhang P, Zhu D, et al. Observational Registry of Basal Insulin Treatment (ORBIT) in patients with type 2 diabetes uncontrolled with oral antihyperglycaemic drugs: real-life use of basal insulin in China. Diabetes Obes Metab. 2017;19(6):822–830. | ||
Yki-Järvinen H, Ryysy L, Kauppila M, et al. Effect of obesity on the response to insulin therapy in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab. 1997;82(12):4037–4043. | ||
Riddle MC, Rosenstock J, Gerich J; Insulin Glargine 4002 Study Investigators. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26(11):3080–3086. | ||
Davies M, Storms F, Shutler S, Bianchi-Biscay M, Gomis R; ATLANTUS Study Group. Improvement of glycemic control in subjects with poorly controlled type 2 diabetes: comparison of two treatment algorithms using insulin glargine. Diabetes Care. 2005;28(6):1282–1288. | ||
Gerstein HC, Yale JF, Harris SB, Issa M, Stewart JA, Dempsey E. A randomized trial of adding insulin glargine vs. avoidance of insulin in people with Type 2 diabetes on either no oral glucose-lowering agents or submaximal doses of metformin and/or sulphonylureas. The Canadian INSIGHT (Implementing New Strategies with Insulin Glargine for Hyperglycaemia Treatment) study. Diabet Med. 2006;23(7):736–742. | ||
Meneghini L, Koenen C, Weng W, Selam JL. The usage of a simplified self-titration dosing guideline (303 Algorithm) for insulin detemir in patients with type 2 diabetes – results of the randomized, controlled PREDICTIVE 303 study. Diabetes Obes Metab. 2007;9(6):902–913. | ||
Garg SK, Admane K, Freemantle N, et al. Patient-led versus physician-led titration of insulin glargine in patients with uncontrolled type 2 diabetes: a randomized multinational ATLAS study. Endocr Pract. 2015;21(2):143–157. | ||
Inzucchi SE, Bergenstal RM, Buse JB, et al; American Diabetes Association (ADA); European Association for the Study of Diabetes (EASD). Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364–1379. | ||
Blonde L, Merilainen M, Karwe V, Raskin P; TITRATE Study Group. Patient-directed titration for achieving glycaemic goals using a once-daily basal insulin analogue: an assessment of two different fasting plasma glucose targets – the TITRATE study. Diabetes Obes Metab. 2009;11(6):623–631. | ||
Rosenstock J, Davies M, Home PD, Larsen J, Koenen C, Schernthaner G. A randomised, 52-week, treat-to-target trial comparing insulin detemir with insulin glargine when administered as add-on to glucose-lowering drugs in insulin-naive people with type 2 diabetes. Diabetologia. 2008;51(3):408–416. | ||
Kennedy L, Herman WH, Strange P, Harris A; GOAL AIC Team. Impact of active versus usual algorithmic titration of basal insulin and point-of-care versus laboratory measurement of HbA1c on glycemic control in patients with type 2 diabetes: the Glycemic Optimization with Algorithms and Labs at Point of Care (GOAL A1C) trial. Diabetes Care. 2006;29(1):1–8. | ||
Fritsche A, Schweitzer MA, Haring HU; 4001 Study Group. Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes. A randomized, controlled trial. Ann Intern Med. 2003;138(12):952–959. | ||
Raskin P, Allen E, Hollander P, et al; INITIATE Study Group. Initiating insulin therapy in type 2 diabetes: a comparison of biphasic and basal insulin analogs. Diabetes Care. 2005;28(2):260–265. | ||
Vaag A, Lund SS. Insulin initiation in patients with type 2 diabetes mellitus: treatment guidelines, clinical evidence and patterns of use of basal vs premixed insulin analogues. Eur J Endocrinol. 2012;166(2):159–170. | ||
Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger PM. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med. 2012;29(5):682–689. | ||
Dailey G, Aurand L, Stewart J, Ameer B, Zhou R. Comparison of three algorithms for initiation and titration of insulin glargine in insulin-naive patients with type 2 diabetes mellitus. J Diabetes. 2014;6(2):176–183. | ||
Khunti K, Davies MJ, Kalra S. Self-titration of insulin in the management of people with type 2 diabetes: a practical solution to improve management in primary care. Diabetes Obes Metab. 2013;15(8):690–700. | ||
Pfutzner A, Stratmann B, Funke K, et al. Real-world data collection regarding titration algorithms for insulin glargine in patients with type 2 diabetes mellitus. J Diabetes Sci Technol. 2016;10(5):1122–1129. | ||
Yki-Jarvinen H. Combination therapies with insulin in type 2 diabetes. Diabetes Care. 2001;24(4):758–767. | ||
Yki-Jarvinen H, Kauppinen-Makelin R, Tiikkainen M, et al. Insulin glargine or NPH combined with metformin in type 2 diabetes: the LANMET study. Diabetologia. 2006;49(3):442–451. | ||
Yki-Jarvinen H, Juurinen L, Alvarsson M, et al. Initiate Insulin by Aggressive Titration and Education (INITIATE): a randomized study to compare initiation of insulin combination therapy in type 2 diabetic patients individually and in groups. Diabetes Care. 2007;30(6):1364–1369. | ||
Heine RJ, Van Gaal LF, Johns D, Mihm MJ, Widel MH, Brodows RG. Exenatide versus insulin glargine in patients with suboptimally controlled type 2 diabetes: a randomized trial. Ann Intern Med. 2005;143(8):559–569. | ||
Janka HU, Plewe G, Riddle MC, Kliebe-Frisch C, Schweitzer MA, Yki-Jarvinen H. Comparison of basal insulin added to oral agents versus twice-daily premixed insulin as initial insulin therapy for type 2 diabetes. Diabetes Care. 2005;28(2):254–259. | ||
Eliaschewitz FG, Calvo C, Valbuena H, et al; HOE 901/4013 LA Study Group. Therapy in type 2 diabetes: insulin glargine vs NPH insulin both in combination with glimepiride. Arch Med Res. 2006;37(4):495–501. | ||
Strange P. Treat-to-target insulin titration algorithms when initiating long or intermediate acting insulin in type 2 diabetes. J Diabetes Sci Technol. 2007;1(4):540–548. | ||
Zinman B, Fulcher G, Rao PV, et al. Insulin degludec, an ultra-long-acting basal insulin, once a day or three times a week versus insulin glargine once a day in patients with type 2 diabetes: a 16-week, randomised, open-label, phase 2 trial. Lancet. 2011;377(9769):924–931. | ||
Schreiber SA, Haak T. Insulin glargine benefits patients with type 2 diabetes inadequately controlled on oral antidiabetic treatment: an observational study of everyday practice in 12,216 patients. Diabetes Obes Metab. 2007;9(1):31–38. | ||
Yki-Jarvinen H, Ryysy L, Nikkila K, Tulokas T, Vanamo R, Heikkila M. Comparison of bedtime insulin regimens in patients with type 2 diabetes mellitus. A randomized, controlled trial. Ann Intern Med. 1999;130(5):389–396. | ||
Kodama K, Tojjar D, Yamada S, Toda K, Patel CJ, Butte AJ. Ethnic differences in the relationship between insulin sensitivity and insulin response: a systematic review and meta-analysis. Diabetes Care. 2013;36(6):1789–1796. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.