Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 12
Knowledge, Awareness, and Perceptions of the Diagnosis and Management of Fibromyalgia Among Physical Therapists in Saudi Arabia: A Cross-Sectional Survey
Authors Alodiabi F , Alhowimel A , Alotaibi M , Alamam D , Fritz JM
Received 30 September 2020
Accepted for publication 12 November 2020
Published 30 November 2020 Volume 2020:12 Pages 293—301
DOI https://doi.org/10.2147/OARRR.S284555
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Chuan-Ju Liu
Faris Alodiabi,1 Ahmed Alhowimel,2 Mazyad Alotaibi,2 Dalyah Alamam,1 Julie M Fritz3
1College of Applied Medical Sciences, Health Rehabilitation Sciences, King Saud University, Riyadh, Saudi Arabia; 2Department of Health and Rehabilitation Science, Sattam Bin Abdulaziz University, Al-Kharj, Saudi Arabia; 3Department of Physical Therapy and Athletic Training, University of Utah, Salt Lake City, UT, USA
Correspondence: Faris Alodiabi
College of Applied Medical Sciences, Health Rehabilitation Sciences, King Saud University, 22480, Riyadh 11495, Kingdom of Saudi Arabia
Tel +966 14676176
Fax +966 14676162
Email [email protected]
Aim: To explore awareness of the diagnostic criteria and management of fibromyalgia (FM) among physical therapists practicing in Saudi Arabia.
Methods: A cross-sectional survey was distributed electronically among musculoskeletal physical therapists. It was designed based on the research literature relevant to FM and reviewed by two rheumatologists for accuracy and comprehension. The survey included two sections: participants’ demographic information and questions related to FM. The data were described using absolute and relative frequencies.
Results: A total of 234 physical therapists accepted the invitation to participate in the study, and 52 were excluded for not satisfying the inclusion criteria or not completing the survey. Responses were received from March to May 2020; only 118 (65%) respondents completed the FM section. The average age of the participants was 31.2 (SD=6.9) years, and 36% were females. Eighty percent reported seeing fewer than five patients with FM in the past year; 51% acquired FM-related knowledge through self-learning; half reported having little to no confidence in their FM assessments and management; and less than 20% were familiar with common diagnostic criteria and management guidelines for FM.
Conclusion: Participating physical therapists showed little awareness of or confidence in the assessment and management of patients with FM; moreover, their awareness was not supported by their adherence to recent FM guidelines. Despite the common practice of referring patients with FM for physical therapy, there are many misconceptions about FM. This study highlights the need for educational programs to provide up-to-date evidence in undergraduate and postgraduate education.
Keywords: fibromyalgia, physical therapy, awareness, knowledge, Saudi Arabia
Introduction
Although fibromyalgia (FM) is a common chronic pain condition, awareness about it is poor, even among healthcare providers. The prevalence of FM ranges from 2% to 9% of the population in various countries.1,2 These discrepancies may be the result of differences in the diagnostic criteria. The most common diagnostic criteria of FM were originally published by the American College of Rheumatology (ACR) in 1990, which emphasized the importance of FM’s chronic and widespread pain and the presence of tenderness in response to palpation of 11 or more sites out of 18 specified areas (tender points).3 However, some presentations of FM did not satisfy these criteria because of the low reliability of such tests and failure to consider the importance of some symptoms (eg, fatigue and cognitive symptoms), which led to the 2010 update of the ACR diagnostic criteria.4 This revision eliminated the need to examine patients for tender points and therefore, a physical exam, making it possible to investigate FM using only surveys.4 The newer criteria also measured the severity of the main symptoms, which allow FM to be viewed on a continuum.4,5 Interventions for people with FM include both pharmacologic and non-pharmacological interventions. However, the main components of FM treatment should include education, exercise, and cognitive-behavioral therapy.6 The cornerstone of FM treatment is evidence-based exercise and physical activity, which is led by a physical therapist and should be given more emphasis.6–8
Awareness, perceptions, and attitudes related to the evidence-based assessment and treatment of FM have been examined in studies by rheumatologists, general practitioners, and medical students.9–15 Theses studies have revealed large variations in perceptions and knowledge of diagnosing and treating FM, not only between different specialties but also within the same specialties. These studies generally reported high percentages of the participants with a poor level or lack of knowledge. Some practitioners doubted the existence of FM as a specific medical condition and others believed it was linked primarily to psychological origins.15 Knowledge and attitudes about FM among medical practitioners in Saudi Arabia have recently been investigated, and the findings were not different from other studies that reported insufficient knowledge.16 Healthcare providers’ insufficient knowledge about FM may lead to poor adherence and higher healthcare costs related to unnecessary testing and delays in providing appropriate treatments for patients. Therefore, there is a need to improve the knowledge and training of rheumatologists and medical practitioners to help them acquire an understanding of FM and adhere to the updated guidelines for diagnosing and treating it.
Education, exercise, and physical activity are integral components of FM management, and there is evidence supporting the need to refer patients with FM for treatment with physical therapy.7,19,20 However, physical therapists’ knowledge, attitudes, and perceptions related to FM diagnoses and management have not been examined. Therefore, our aim was to explore their awareness of the diagnosis and management of FM in Saudi Arabia. Doing this can promote the development of continuing education programs and training sessions designed for physical therapists to improve their effectiveness in treating patients with FM.
Methods
A cross-sectional survey was conducted to address the primary objective of this research: to examine the knowledge of FM diagnoses and management amongst physical therapists in Saudi Arabia.
The survey included three sections: first section contains study overview (targeted participants, purpose, who is conducting the study and assurance of anonymous indemnification) and consent check box so that all participants provided informed consent within the survey. The second section includes questions pertaining to participants’ demographics and to FM. The questions about FM that were developed were based on the literature pertaining to its diagnostic criteria3–6 and FM-related studies.9–16 We sent the survey to two rheumatologists practicing in Saudi Arabia who assessed its accuracy, comprehensiveness, and readability. The FM-related questions included: items that assessed the respondent’s educational background and sources of information about FM, their level of confidence in assessing FM (5-point Likert scale), confidence in managing FM (5-point Likert scale), knowledge and awareness of common FM diagnostic criteria and management guidelines (1990 ACR,3 2010 ACR,4,5 2012 Canadian Guidelines),7 perceptions of different healthcare professions and their roles in managing FM cases (primary role, secondary role, no role), knowledge and awareness of FM risk factors, the degree to which they agreed with common recommendations for FM interventions (4-point Likert scale), and a quiz on general knowledge of FM (true/false items).
We sought a convenience sample, so we distributed the questionnaires and received responses electronically. An electronic invitation was sent to eligible participants (through social media and direct invitation applications). To be eligible in the study, participants had to be a physical therapist practicing in Saudi Arabia who managed and treated patients with musculoskeletal/orthopedic conditions. Data from students and internship physical therapist will be excluded. The Institutional Review Board at King Fahd Medical City (H-01-R-012) reviewed and approved the study.
Statistical Analysis
All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) (IBM Corp, version 26). Information on participants’ demographics, knowledge, and perceptions was described using absolute and relative frequencies. The Chi-square test was used to examine the associations between categorical variables. The significance level was set at 0.05.
Results
A total of 234 physical therapists accepted the invitation to participate in the study; however, 32 who did not complete the survey and 20 who did not satisfy the inclusion criteria (manage and treat musculoskeletal/orthopedic conditions) were excluded. Responses were received between March and May 2020.
Of the 182 included participants, 66 (36%) were females; the mean age was 31.2 (SD=6.9) years; 168 (92%) were from Saudi Arabia; 110 (60%) held a bachelor’s degree as their highest degree of education; 135 (74%) received their highest degree in Saudi Arabia; and most of the participants (143, 79%) received their highest degree after 2010. The practice regions and practice experience (in years) of the participants were diverse; however, 75 (41%) of the sample practiced in Riyadh and 97 (53%) had less than 6 years of clinical experience. The participants’ demographic data are presented in Table 1.
 |
Table 1 Participants’ Characteristics |
A total of 118 respondents (65%) completed the questions in the FM section. Based on the Chi-square test, no significant differences (p>0.05) were found between those who completed the entire survey and those who did not, in terms of age, gender, and educational level.
Estimated Number of Patients with FM Seen per Year
During the past year, 42 (36%) of the participants received no FM referrals and 53 (45%) reported seeing 1 to 5 FM cases per year. The other 23 (19%) reported seeing more than 5 FM cases per year.
Sources of Knowledge About FM
Approximately 40 (22%) reported learning about FM during their undergraduate education and 29% during their postgraduate education. Additionally, 60 (33%) acquired FM-related knowledge through self-learning activities, 14 (8%) claimed they did not have knowledge about FM, and 2 (1%) reported gaining knowledge through contact with a family member or a patient with FM.
Levels of Confidence in Assessing, Diagnosing, and Managing FM Cases
Approximately 26 (22%) reported they were “not confident at all” in their assessment and diagnosis of patients with FM and 19 (16%) were “not confident at all” in their management of patients with FM. Only 24 (20%) reported being “quite confident” or “extremely confident” in their abilities to assess and diagnose patients with FM. This was little bit higher when it comes to being “quite confident” or “extremely confident” in the abilities to manage patients with FM; 34 (29%). Participants’ levels of confidence in their assessment and management of FM are presented in Figure 1.
 |
Figure 1 Participants’ levels of confidence in assessing, diagnosing, and managing FM cases. |
Knowledge and Awareness of Common FM Diagnostic Criteria and Management Guidelines
We asked the participants about their knowledge and awareness of common guidelines for the diagnostic criteria and management of FM (1990 ACR,3 2010 ACR,4,5 2012 Canadian Guidelines).7 The majority reported they were not aware of these guidelines. Figure 2 presents our findings on the participants’ knowledge and awareness of FM practice guidelines.
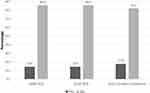 |
Figure 2 Participants’ knowledge and awareness of three common FM practice guidelines. |
Perceptions of Roles of Various Healthcare Professions in the Management of FM Cases
The participants’ perceived roles of different healthcare providers varied. The majority reported that pain management physicians (78, 66%) and physical therapists (80, 68%) have a primary role in managing FM symptoms. Figure 3 presents the percentages of the participants’ perceived roles of each type of healthcare provider in managing FM.
 |
Figure 3 Participants’ perceived roles of each type of healthcare provider in managing FM. |
Participants’ Knowledge and Awareness of FM Risk Factors
The majority of the participants indicated that stress (93, 79%), physical inactivity (74, 63%), gender (73, 62%), genetics (63, 53%), and poor sleep (61, 52%) are risk factors for developing FM. The findings are presented in Figure 4.
 |
Figure 4 Participants’ knowledge and awareness of risk factors for FM. |
Degree of Participants’ Recommendations for Common FM Interventions
Most of the participants highly recommended pain education (86, 73%) and self-management (74, 63%) for the management of FM symptoms. However, other interventions received a mixture (high and low) of recommendations. Passive interventions, including acupuncture, dry needling, and ultrasound and electrotherapy were less likely to be recommended. The findings are presented in Figure 5.
 |
Figure 5 Degree of the participants’ recommendations for common interventions for FM conditions. |
General Knowledge Quiz
The majority of participants agreed that FM is characterized by widespread musculoskeletal pain (104, 88%), is associated with sleep disturbances (94, 80%), fatigue (90, 76%), anxiety and/or depression (80, 68%), waking up unrefreshed (70, 59%), and forgetfulness and concentration difficulties (62, 53%). Similarly, most of them agreed that FM impacts the affected individual’s quality of life (109, 92%).
On the other hand, the majority of participants disagreed that FM treatment depends mainly on medications (98, 83%), that FM is an inflammatory joint disease (87, 74%), that FM is completely psychological (84, 71%), that it causes deformities in joints (78, 66%), and that it is seen equally in females and males (67, 57%). See Table S1 for the results of the knowledge quiz.
Discussion
This study’s aim was to examine the awareness of diagnosis and management of FM among physical therapists practicing in Saudi Arabia. This study highlights several drawbacks in their current knowledge. There was a lack of awareness of the diagnostic criteria and guidelines for FM management among the physical therapists, and almost 80% were unaware of the three most commonly used diagnostic criteria. Lack of awareness and experience of FM may also explain why many respondents did not answer questions about treatment of the condition. Therefore, it was not surprising that physical therapists have little confidence in their abilities to assess, diagnose, and treat patients with FM.
It was found that more than half of the responders had less than 6 years clinical experience. This could be because Saudi Arabia has increased further education in physical therapy in recent years. Alghadir et al21 found that between 2005 and 2015, the number of universities in Saudi Arabia offering a bachelor’s degree course in physical therapy increased from 6 to 16. High participation of young and less experienced therapists may be also the data collection electronic method. Yetter and Capaccioni22 found that younger respondents were more likely to answer surveys distributed online and older respondents prefer paper ones. This may limit the generalizability of the findings since it may yield different results if the average age and experience was higher. Younger and newly graduate are expected to have higher and updated level of knowledge since they just learned new evidence related to FM. Nonetheless, our findings showed limited knowledge and confidence which reflect the need to have more emphasis regarding rheumatology and FM in the physical therapy curriculum.
While the prevalence of FM has been reported to be 2–9% of the general population,1,2 more than 50% of the physical therapists in this study stated that the number of patients treated for FM per year is less than five patients. The awareness of FM’s diagnostic criteria in Saudi Arabia was found in another study to be inadequate.16 This finding also raises doubts that physical therapy is considered a preferred service for patients with FM, which might reflect referring physicians’ inadequate knowledge of the physical therapist’s role.
The physical therapists’ lack of knowledge and awareness about FM in the present study is consistent with similar previous studies on other professions.9–15 The main difference is that physical therapy in the Saudi healthcare system is a referral-based service, and patients approach the clinic with a predefined diagnosis. Therefore, lack of knowledge and awareness of the diagnostic criteria is more understandable because of patients’ predefined diagnoses; however, knowledge of treatment recommendations is especially important for physical therapists.
Only one-quarter of the physical therapists in this study’s sample reported having undergraduate education about FM; therefore, their knowledge about the standard diagnostic criteria for FM was poor. More than 30% of this study’s sample believed FM is objectively defined and that lab tests or imaging is needed for a diagnosis. It has been reported23 that physical therapists think FM is caused by psychological factors. Kaki and Hazazi16 reported a similar finding in a mixed group of healthcare professionals in Saudi Arabia, highlighting that only 26% of the participants learned about FM during their undergraduate education, and only 33% reported being familiar with its diagnostic criteria. A qualitative study of medical students reported that the students’ lack of formal education about FM led them to perceive FM as less important than other subjects in the curriculum.17
Lack of confidence in the management of musculoskeletal symptoms has been reported to correlate with performance on tests of general musculoskeletal knowledge.18,24,25 In the present study, 75% of physical therapists were not entirely confident in handling FM symptoms; hence, this deficiency in knowledge is expected. It should be noted that confidence in managing FM has also been positively associated with FM-related experiences (21). In our sample, almost half of the participants had less than 5 years of clinical practice.
The best non-pharmacological interventions for FM, which yield sustained functional improvement, are education, exercise, and cognitive behavioral therapy.6,26 The participants in our study gave various responses regarding treatment recommendations, with passive physical therapy or unproven treatments (eg, needling, trigger point therapy, massage, ultrasound, and electrotherapy) recommended by 32% to 56% of them. However, 49% to 81% recommended active physiotherapy or effective interventions, such as aerobic and strengthening exercises, and 65% recommended cognitive behavioral therapy. Lack of knowledge was apparent in the participants’ selections of treatment options.
The present study highlights the current lack of knowledge amongst essential care providers for patients with FM. Notably, other research studies undertaken in other countries report similar findings. For example, Blotman et al10 found that lack of medical school training and continuing professional education about FM led to lack of understanding amongst medical professionals about the condition.
It is imperative to incorporate evidence-based knowledge about FM in undergraduate education and provide short educational courses to practising physical therapists as part of continued professional development. These educational courses should address the primary symptoms of FM, how to identify the condition, and current physical therapy-based treatment options for the condition.
Furthermore, effective communication is needed between healthcare providers involved in the care of patients with FM. Physical therapists need to work with referring physicians to optimise the care of patients with FM. Although lack of knowledge has been reported amongst different healthcare providers in Saudi Arabia, there is also a need to listen to the experiences of patients’ undergoing assessments and management by healthcare providers, and how these skills can be improved.
Limitation
The current study has limitations. First, this study used a cross-sectional design with self-report questions, which might have promoted selection bias. Second, the sample size and the selection process of the study might limit the generalisability of the findings, although the participants were from different educational backgrounds. Another limitation with the study was that more than half of the participants were younger physical therapists with less than 6 years’ experience. This may limit the generalizability of the findings as stated before. Future research may utilize both electronic and paper forms of the questionnaire to reach wider and variant population.
Conclusion
The current study intended to explore the awareness and knowledge of physical therapists practicing in Saudi Arabia about FM diagnostic criteria, assessment, and management. The findings showed limited knowledge and lack of confidence in assessing and managing FM cases. Updated and evidence-based knowledge about FM should be incorporated in the undergraduate physical therapy education.
Funding
This project was supported by the Deanship of Scientific Research at Prince Sattam Bin AbdulAziz University under the research project number 2019/01/13,195.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38:19–28. doi:10.1002/art.1780380104
2. Queiroz LP. Worldwide epidemiology of fibromyalgia. Curr Pain Headache Rep. 2013;17:356. doi:10.1007/s11916-013-0356-5
3. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum. 1990;33:160–172. doi:10.1002/art.1780330203
4. Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010;62:600–610. doi:10.1002/acr.20140
5. Wolfe F, Clauw DJ, Fitzcharles MA, et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol. 2011;38:1113–1122. doi:10.3899/jrheum.100594
6. Clauw DJ. Fibromyalgia: a clinical review. JAMA. 2014;311:1547–1555. doi:10.1001/jama.2014.3266
7. Fitzcharles MA, Ste-Marie PA, Goldenberg DL, et al. 2012 Canadian guidelines for the diagnosis and management of fibromyalgia syndrome: executive summary. Pain Res Manag. 2013;18:119–126. doi:10.1155/2013/918216
8. Fink L, Lewis D. Exercise as a treatment for fibromyalgia: a scoping review. J Nurse Pract. 2017;13:546–551. doi:10.1016/j.nurpra.2017.06.018
9. Arshad A, Ooi KK. Awareness and perceptions of fibromyalgia syndrome: a survey of Southeast Asian rheumatologists. J Clin Rheumatol. 2007;13:59–62. doi:10.1097/01.rhu.0000260494.29921.9e
10. Blotman F, Thomas E, Myon E, Andre E, Caubere JP, Taieb C. Awareness and knowledge of fibromyalgia among French rheumatologists and general practitioners. Clin Exp Rheumatol. 2005;23:697.
11. Mu R, Li C, Zhu JX, et al. National survey of knowledge, attitude and practice of fibromyalgia among rheumatologists in China. Int J Rheum Dis. 2013;16:258–263. doi:10.1111/1756-185X.12055
12. Kumbhare D, Ahmed S, Sander T, Grosman-Rimon L, Srbely J. A survey of physicians’ knowledge and adherence to the diagnostic criteria for fibromyalgia. Pain Med. 2017;19:1254–1264. doi:10.1093/pm/pnx271
13. Agarwal A, Oparin Y, Glick L, et al. Attitudes toward and management of fibromyalgia: A national survey of Canadian rheumatologists and critical appraisal of guidelines. J Clin Rheum. 2018;24:243–249. doi:10.1097/RHU.0000000000000679
14. Ortiz FE, de la Cruz VA, Jiménez FE. Knowledge on fibromyalgia among general practitioners, from Chiclayo-Peru, 2016. Rheumatol Clín. 2017;13:326–330. doi:10.1016/j.reumae.2016.08.005
15. Amber KT, Brooks L, Chee J, Ference TS. Assessing the perceptions of fibromyalgia syndrome in United States among academic physicians and medical students: where are we and where are we headed? J Musculoskeletal Pain. 2014;22:13–19. doi:10.3109/10582452.2014.883024
16. Kaki AM, Hazazi AA. Assessment of medical practitioners’ knowledge of fibromyalgia in Saudi Arabia. Saudi J Anaesth. 2018;12:178. doi:10.4103/sja.SJA_458_17
17. Silverwood V, Chew-Graham CA, Raybould I, Thomas B, Peters S. ‘If it’s a medical issue I would have covered it by now’: learning about fibromyalgia through the hidden curriculum: a qualitative study. BMC M Educ. 2017;17. doi:10.1186/s12909-017-0972-6.
18. Amber KT, Brooks L, Ference TS. Does improved confidence in a disease relate to increased knowledge? Our experience with medical students. Pain Med. 2014;15:483–484. doi:10.1111/pme.12315
19. Stucki MOG. Physical therapy in the treatment of fibromyalgia. Scand J Rheumatol. 2000;29:78–85. doi:10.1080/030097400446706
20. Hävermark AM, Langius‐Eklöf A. Long‐term follow up of a physical therapy programme for patients with fibromyalgia syndrome. Scand J Caring Sci. 2006;20:315–322. doi:10.1111/j.1471-6712.2006.00410.x
21. Alghadir A, Zafar H, Iqbal ZA, Anwer S. Physical therapy education in Saudi Arabia. J Phys Ther Sci. 2015;27:1621–1623. doi:10.1589/jpts.27.1621
22. Yetter G, Capaccioli K. Differences in responses to web and paper surveys among school professionals. Behaviour Research Methods. 2010;42:266–272. doi:10.3758/BRM.42.1.266
23. Roitenberg N, Shoshana A. Physiotherapists’ accounts of fibromyalgia: role-uncertainty and professional shortcomings. Disabil Rehabil. 2019;1–8. doi:10.1080/09638288.2019.1632939
24. Freedman KB, Bernstein J. The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am. 1998;80:1421–1427. doi:10.2106/00004623-199810000-00003
25. Ahern MJ, Soden M, Schultz D, Clark M. The musculo‐skeletal examination: a neglected clinical skill. Aust N Z J M. 1991;21:303–306. doi:10.1111/j.1445-5994.1991.tb04694.x
26. Mengshoe AM. Physiotherapy management of fibromyalgia: what do we know and how may this affect clinical practice? Phys Ther Rev. 2000;5:85–91.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
