Back to Journals » Cancer Management and Research » Volume 10
Ki-67 index and percentage of sarcomatoid differentiation were two independent prognostic predictors in sarcomatoid renal cell carcinoma
Authors Wang Z, Zeng X, Chen R, Chen Z
Received 4 June 2018
Accepted for publication 7 September 2018
Published 5 November 2018 Volume 2018:10 Pages 5339—5347
DOI https://doi.org/10.2147/CMAR.S176242
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Antonella D'Anneo
Zhixian Wang,1 Xiaoyong Zeng,1,2 Ruibao Chen,1 Zhiqiang Chen1,2
1Department of Urology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei 430030, China; 2Hubei Institute of Urology, Wuhan, China
Purpose: To identify whether and which of pathological features of sarcomatoid differentiation (SD) in renal cell carcinoma (RCC) can be used as independent predictors associated with overall survival (OS).
Materials and methods: After institutional review board approval, patients with a diagnosis of sarcomatoid RCC (sRCC), spindled RCC, or RCC with the presence of spindle cells between 2003 and 2017 were further selected and re-examined. The primary pathological features including histological subtypes, tumor necrosis, Ki-67 index of SD, and the percent of SD (%SD) were included into analysis. Histological subtypes were categorized into clear-cell RCC and nonclear-cell RCC. Ki-67 index of SD was confirmed by immunohistochemical staining. %SD was estimated through reviewing all of the tumor sections microscopically and then giving an approximate %SD within the entire tumor. The clinical relevant prognostic predictor’s association with OS was analyzed within Cox proportional hazards regression models. Survival curves were generated using the Kaplan–Meier method, and OS differences were compared using the log-rank test.
Results: A total of 2,089 consecutive patients of RCC were referred to our department, of whom 62 (3.0%) patients were identified with histological element of SD after re-examining the available slides of suspicious cases. Finally, 53 patients were included into survival analysis after excluding 9 patients without adequate information. Thirty-eight (71.7%) patients died at last follow-up. The median OS for all patients was 11.0 months from the date of surgery. In patients with clinical distant metastasis (cM1), the median OS was only 3 compared with 21 months for patients with no clinical distant metastasis (cM0). Tumor stage, status of clinical distant metastasis, Ki-67 index, and %SD were independent predictors of multivariate analysis in overall 53 patients. However, in the cohort of cM0 patients, we found that only %SD and Ki-67 index were two independent predictors of OS in multivariate analysis.
Conclusion: Patients with sRCC are associated with very poor prognosis. Ki-67 index of SD and %SD were identified as the two most important independent predictors particularly for nonmetastatic patients. The limitations of our study were also observed, and further studies are needed.
Keywords: sarcomatoid renal cell carcinoma, nephrectomy, Ki-67, percentage, survival
Introduction
Sarcomatoid differentiation (SD) in renal cell carcinoma (RCC) is an indicator of poor prognosis1,2 and is more likely to present with advanced disease at first presentation.1,3–7 Sarcomatoid RCC (sRCC) was not considered a separate RCC type currently, since it can be observed across all histological types in either clear-cell RCC (ccRCC) or nonclear-cell RCC (ncRCC).8–11 Transition from epithelial to mesenchymal cells has been proposed as a potential mechanism for the development of SD in RCC.1,9,12 Histologically, it presents features of sarcoma, with atypical spindle-like cells and/or malignant-appearing giant cells interposed with RCC components.9 Although sRCC is a rare morphotype with a low incidence rate of 1%–8% of all RCCs,3 but it has extensive associations with poor clinical outcomes with a low median survival of <1 year.3,9,13 Despite good effects of surgical treatments for patients with localized RCC14 and new drugs for systemic therapies including targeted therapies against vascular endothelial growth factor (VEGF) and mammalian target of rapamycin pathways for advanced patients who demonstrate better survival,13,15,16 but only few patients with sRCC benefit from systemic therapies.8,13,17–19
Several clinicopathological characteristics were reported to be associated with the poor prognosis, and more recent studies have focused on molecular and genomic characteristics of sRCC1,2,5–7,9; however, some risk features were not observed because histological criteria were changed, and a larger proportion of patients with clinical distant metastasis (cM1) were in prior studies, most of which included patients from a period of at least a decade earlier. Nowadays, because of wide use of regular physical examination by abdominal imaging technologies, this may contribute to increase in the diagnosis of patients with no clinical distant metastasis (cM0), and there exists no commonly accepted prognostic nomogram for clinicians in this new period. So a further investigation for predicting prognostic factors of sRCC is still warranted. We aimed to identify predictors of risk stratification in patients with sRCC treated with surgery to better counsel patients and provide more information regarding clinical trial design.
Materials and methods
The research complied with the Declaration of Helsinki rules, and this retrospective study was approved by the Ethics Committee of Tongji Hospital, Huazhong University of Science and Technology. The need for informed consent from all patients was waived because this was a retrospective study. All data had no personal identifiers and were kept confidential. All patients diagnosed with RCC confirmed pathologically were reviewed at Tongji Hospital, Huazhong University of Science and Technology between January 2003 and September 2017.
Clinicopathological characteristics
The clinical variables included gender, age at surgery, body mass index, symptoms at first presentation, comorbidities and Charlson Comorbidity Index, American Society of Anesthesiologists (ASA) score, TNM stage, and lymph nodes (LNs) status determined by imaging. The TNM stage classification was re-evaluated by two clinicians based on the American Joint Cancer Committee (AJCC), 8th edition (2016).20 Tumor size was defined as the longest dimension of the tumor via preoperative computed tomography (CT)/MRI; tumor stage was confirmed by pathological tumor (pT) stage; status of regional LNs was based on the pathologist’s assessment; and all patients underwent evaluation of clinical distant metastasis before surgery, including chest radiography/chest CT and abdominal and pelvic CT/MRI. Bone scan and brain CT/MRI were also offered as clinically indicated. All patients with sRCC underwent radical nephrectomy or cytoreductive nephrectomy, which included removal of the affected kidney together with the perirenal fat; LNs and adrenal dissection were routinely performed when the metastasis was indicated by preoperative imaging and intraoperative suspect. Metastasectomy was not recommended for this group of patients with cM1 because of multiple or organ-diffused metastases. In consideration of poor prognosis of this disease, we would not recommend to perform surgical treatment for patients with weak performance status, so all patients in our cohort were in a good performance status (The Eastern Co-operative Oncology Group performance status: 0–1 score) and can get a better recovery after surgery. Because most of patients received continued treatment locally postsurgery, we could not assess the postoperative performance status, so we did not include it into analysis.
Patients with a diagnosis of sRCC, spindled RCC, or RCC with the presence of spindle cells were further selected for analysis and were re-examined. The sRCC presents features similar to sarcoma with atypical spindle-like cells and/or malignant-appearing giant cells interposed with RCC epithelial components.9 The primary characteristics including histological subtypes, tumor necrosis, Ki-67 index of SD, and the percent of SD (%SD) were included into analysis with other clinical variables. Histological subtype was categorized into ccRCC and ncRCC based on AJCC, the Union for International Cancer Control, and the Heidelberg classification system.21,22 ncRCC includes papillary, chromophobe, collecting duct, and unclassified RCC subtypes. Ki-67 index of SD was confirmed by immunohistochemical staining, and it was considered as a continuous and categorical variable with cut-off points of 30% and 50% to analyze. %SD was estimated as Kim et al6 reported through reviewing all of the tumor sections microscopically, then giving an approximate percentage of the presence of SD within the entire tumor. In order to keep repeatability, we just use 25% and 50% as cut-off point to re-assess the %SD. Only two patients showed features of microvascular invasion, so we excluded it from the analysis. Because sarcomatoid and rhabdoid differentiations are incorporated into WHO/International Society Of Urological Patheology grade 4,20 we did not include the nuclear grade.
Patient outcome follow-up
The follow-up evaluation for patients with sRCC comprises abdominal ultrasound/CT/MRI performed every 3–6 months for the first 2 years postsurgery, every 6 months from postoperative 3–5 years, and every 12 months thereafter. The electronic medical record system and computer-based patient’s record in our outpatient department were the mainly used methods for follow-up, although other methods were also used such as telephone, letter, or other modes of communication to track the patients’ prognosis and the cause of death. The medical history and death certificate were reviewed by two urologists together to determine the cause of death or must be verified with the patient’s family if a death certificate cannot be obtained. Overall survival (OS) was the primary end point and was assessed from the date of surgery to date of death or last follow-up. OS was our primary end point in our study not the cancer-specific survival. Although most patients died from RCC, we were unable to verify the cause of death in few cases, since a majority of patients continued surveillance or treatment locally after the surgery in our center.
Statistical analysis
Continuous and categorical variables were expressed as median (IQR) and frequency counts (percent, %), respectively. The cut-off value of age for the prediction of OS was determined by mean value. Kaplan–Meier survival analysis was used to calculate the probability of OS, and survival differences were compared using the log-rank test. Associations of clinical and pathological characteristics with OS were evaluated using Cox proportional hazards regression models and summarized with HR and 95% CI. Univariate and multivariate Cox models were conducted. All P-values were corrected for multiple hypothesis testing, and false discovery rate (FDR)-corrected P-values (FDR-P) were used. The baseline variables with FDR-P <0.05 in univariable analysis and variables reported clinical relevant in prior studies were included into the multivariate Cox proportional hazards regression model. Pathologic LNs stage and TNM stage were not included in the regression analysis because a majority of patients did not have LNs removed. A P-value <0.05 was considered to represent a statistically significant difference; all reported P-values were two-sided. All analyses were conducted using SPSS 19.0 (SPSS Inc., Chicago, IL, USA). Figures were drawn by GraphPad Prism v.6 (GraphPad Software, Inc., La Jolla, CA, USA).
Results
Baseline clinical and pathological characteristics
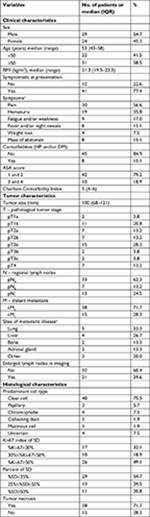
A total of 2,089 patients with RCC underwent surgery between January 2003 and September 2017 at our center. We identified 62 (3.0%) patients with histological element of SD after re-examining the available slides of suspicious cases; 53 patients, finally, were included in our study after we excluded 9 patients without adequate information of important variables and missed follow-up. The clinicopathological characteristics of the 53 patients are reported in Table 1. All patients underwent radical or cytoreductive nephrectomy before pathological diagnosis. The median age (IQR) of the cohort was 53 (43–58) years; male patients were 1.21 fold of female patients in the cohort. A majority of patients had larger tumor size (median [IQR], 100 [68–121] mm), and more than half of the patients suffered symptoms of flank pain (56.6%) and hematuria (35.8%) at first presentation in patients with symptoms; 15.1% (8/53) patients had comorbidities of hypertension and/or diabetes mellitus; and the median Charlson Comorbidity Index was 5 (4–6) score. Approximately half of patients had local progressive disease (49.1% pT3–4), only 20 (37.7%) patients had regional LNs removed, and the rate of positive lymph nodes/negative lymph nodes (pN1/pN0) was 1.86:1 (13:7). 28.3% patients with cM1 were diagnosed. Lung and liver were the most common sites of metastasis. ccRCC accounted for 75.5% histological subtype, 71.7%, 68.0%, and 45.3% tumors showed necrosis, Ki-67 index of SD ≥30%, and %SD ≥25%, respectively.
Survival outcomes and stratification analysis
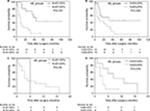
The median OS for all patients was 11 months from the date of surgery (Figure 1A). In cM0 patients, the median OS was 21 months compared with only 3 months for cM1 patients (Figure 1B). Thirty-eight (71.7%) patients died at last follow-up, 33 of them died of cancer confirmed by death certificate, and the causes of another five patients were not verified and just knew the time of death from his or her families. Median length of follow-up for 15 survivals was 23.5 months (IQR: 13.5–62.25). Nine of thirty patients with negative or not assessed lymph-node (pN0/X) and cM0 presented metastasis-free survival, and the median duration of the follow-up was 65 months (IQR: 20.5–97) for this group. At least 13 of 38 cM0 patients observed local and/or distant recurrence with median of 5 months (IQR: 2.5–9). The most common site of postoperative metastases for patients with cM0 were lung (N=5), bone (N=3), intra-abdominal (N=3) and ipsilateral local (N=4). There were only three patients with cM1 treated with targeted therapy (sorafenib or sunitinib) after surgery; two of them refused the therapy contining because of adverse effects of the drugs, and another one died 4 months after surgery. Others did not receive systemic therapy in consideration of effects of drugs and financial burden, so just cytoreductive nephrectomy was performed for them for relief of symptoms. However, we were unable to confirm accurately the types of postoperative systemic therapy because a majority of patients who experienced disease advanced or tumor recurrence were managed in their local cancer center.
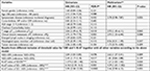
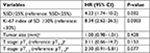
Overall, the 1-, 2-, and 5-year OS for the cohort was 43.5%, 34.2%, and 20.2%, respectively. The 1-, 2-, and 5-year OS for cM0 patients was 59.1%, 44.3%, and 26.1%, respectively, but 1-year OS for cM1 was only 26.7%. Advanced pT stage (pT3 and pT4) had a worse prognosis with median OS of 7 months in comparison with median OS of 27 months for stages pT1 and pT2 (Figure 2A). Ki-67 index and %SD with cut-off point of 30% and 25%, respectively, demonstrated significance in Kaplan–Meier survival analysis (Figure 2B, C). In contrast, the cohort of cM0 patients with Ki-67 index of SD ≥30% and ≥25% SD had significantly worse OS compared with Ki-67 index <30% and<25% SD (Figure 3A, B); however, in the cM1 setting, there was no observed difference (Figure 3C, D).
  | Figure 2 Kaplan–Meier survival curves for overall survival stratified by (A) tumor stage, (B) Ki-67 index of SD, and (C) %SD. Abbreviations: SD, sarcomatoid differentiation; %SD, percent of SD. |
Predictors associated with prognosis
Univariate and multivariate analyses were used to assess which clinicopathological features of 53 patients were associated with OS (Table 2). In univariate analysis, age, gender, comorbidities of hypertension and diabetes mellitus, Charlson Comorbidity Index, ASA stage, and histological type were not associated with OS after P-values were corrected for multiple hypothesis testing with FDR-P. The variables found to be significant in the univariable analysis were further analyzed in the multivariate Cox model. In order not to miss underlying predictors, we also included the features of necrosis, histological types, and %SD in the model, although these variables were not statistically significant after multiple hypothesis testing; however, we found that no evidence of pathological features of tumor necrosis was significantly associated with OS in multivariate analysis. T stage, distant metastatic diseases, %SD, and Ki-67 index of SD were independent prognostic predictors. %SD with either 25% or 50% as a cut-off point did influence OS in univariate analysis. The same thing happened with Ki-67 index with either 30% or 50% as cut-off points, but both Ki-67 and %SD did not observe statistical significance when 50% was considered as a cut-off value in multivariate analysis. In addition, for cM0 patients, %SD and Ki-67 index of SD with 25% and 30% as cut-off points, respectively, were the two most important independent predictors for OS (P=0.0003 and P=0.002 for Ki-67 and %SD respectively, Table 3). Meanwhile, we also found that in the cohort of cM0, symptom diseases were a predictor but tumor size and tumor stage were not associated with OS.
Discussion
Fifty-three patients diagnosed with sRCC were analyzed in detail. Herein we again observed RCC with feature of SD have extremely poor outcomes. In our cohort, we observed only the median 11.0 months OS for all patients with metastases or not at diagnoses, what’s more, only the median 21 months OS for cM0 patients. We observed that some patients benefited from surgery and showed prolonged progression-free survival.1,6 We hypothesized that a lower proliferative rate might contribute to a better prognostic outcome. Our data identified that %SD and Ki-67 index of SD were two independent predictors of OS, which might provide practical and clinical information of prognosis for clinicians to better counsel patients in the period of targeted therapy.
A majority of previous studies have attempted to risk stratify patients diagnosed with sRCC based on pathological features.1,2,4–6 Similarly, a prior study that was reported by Kim et al6 also found this results, in cM0 setting, the tumors harboring much more %SD were more likely to suffer progression of disease and assert greater influence on OS. In their study, 50% as a cut-off point for %SD was not continue to analyzed when just found that 25% of SD can observed different influence on OS, in addition, Ki-67 index was not included in their study. Recently, Wang et al23 have shown the poor prognostic value of high Ki-67 index in RCC by meta-analysis. In the present study, we identified that the discrimination capability of either %SD or Ki-67 index was decreased when the cut-off point increased to 50%, which informed us that there might be another better cut-off point for a better discrimination of prognostic outcomes in the interval of 25%–50% for %SD and 30%–50% for Ki-67 index. Another study by Zhang et al1 increased the cut-off point of %SD to 30%, and indicated patients with tumors presenting ≥30% of SD were 52% more likely to die from sRCC than those with tumors with element of SD <30%, but they did not stratify patients based on the distant metastatic diseases (cM1 and cM0). We found that neither %SD nor Ki-67 index was associated with OS for patients without distant metastatic diseases but not for the cM1 cohort, which was consistent with Kim et al.6 In addition, some studies found that the amount of SD impacts response to therapy. It has been reported that RCCs with <20% SD have partial response to targeted therapy, and those with higher amounts of SD are more likely to respond to cytotoxic chemotherapy consisting of doxorubicin and gemcitabine.17,24
In our study, we also want to investigate whether there exists different influence between histological types on OS. But, in the present study, we did not find that histological types of RCC could reach statistical significance. To our knowledge, the utility of histological types as a predictor remains controversial. The histological features of SD can be observed in all types of RCC25; ccRCC is the most common histological subtype, which accounts for about 65%–79% of all histological subtype with sarcomatoid differentiation.1,2,5–8,18 Nguyen et al2 showed that histological subtype was associated with cancer-specific survival (P=0.001) but not associated with distant metastasis (P=0.8) in patients with sRCC and found that patients with ncRCCs were more likely to die from sRCC (HR: 2.3: 95% CI: 1.38–3.82) than ccRCC. In the targeted therapy period, Golshayan et al17 found that patients with metastatic sRCC with underlying histological subtype of ccRCC were more likely to respond to VEGF-targeted therapy. Conversely, Cheville et al26 showed that ccRCC and chromophobe RCC were more likely to have tumors with SD (5.2% and 8.7%, respectively), but the underlying histological subtype of sRCC was not a prognostic predictor.
There are some limitations to our study. First, the retrospective design and small sample size in this single center study were unable to further stratify prognostic predictors (eg, tumor stage, histological subtypes, etc). Although the long follow-up time was accrued over 15 years, 89% patients with sRCC were referred to our center after 2010 and the similar technique of radical nephrectomy was performed for all patients. In addition, regional retroperitoneal LN dissection was not routinely performed and was determined by the operating surgeon at nephrectomy; however, a standard of the extent of LN dissection was still not identified, and most of prior studies were also not well evaluated. The findings should be validated in a larger cohort and should identify a better cut-off point.
Conclusion
SD is associated with a very poor prognosis for patients with RCC regardless of metastasis, as reported in this single institution analysis of 52 cases. Although underlying subtype of ccRCC and ncRCC and necrosis features did not reach statistical significance, the tumor features with higher proliferation rate including Ki-67 index of SD ≥30% and %SD ≥25% were associated with higher risk of death from sRCC and identified two most important independent predictors. The limitations of our study were also observed, and further studies are needed.
Acknowledgments
The authors thank Chunxiang Feng, Chang Liu, Shiliang Liu, and Kai Yu for data collection. Prof Tao Wang, Xiaolin Guo, Zhiquan Hu, Qianyuan Zhuang, Shaogang Wang, Jihong Liu, and Zhangqun Ye provided detailed patients’ information and gave significant suggestion for original manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Zhang BY, Thompson RH, Lohse CM, et al. A novel prognostic model for patients with sarcomatoid renal cell carcinoma. BJU Int. 2015;115(3):405–411. | ||
Nguyen DP, Vilaseca A, Vertosick EA, et al. Histologic subtype impacts cancer-specific survival in patients with sarcomatoid-variant renal cell carcinoma treated surgically. World J Urol. 2016;34(4):539–544. | ||
Thomas AZ, Adibi M, Slack RS, et al. The role of metastasectomy in patients with renal cell carcinoma with sarcomatoid dedifferentiation: a matched controlled analysis. J Urol. 2016;196(3):678–684. | ||
Shuch B, Said J, Larochelle JC, et al. Histologic evaluation of metastases in renal cell carcinoma with sarcomatoid transformation and its implications for systemic therapy. Cancer. 2010;116(3):616–624. | ||
Shuch B, Bratslavsky G, Shih J, et al. Impact of pathological tumour characteristics in patients with sarcomatoid renal cell carcinoma. BJU Int. 2012;109(11):1600–1606. | ||
Kim T, Zargar-Shoshtari K, Dhillon J, et al. Using percentage of sarcomatoid differentiation as a prognostic factor in renal cell carcinoma. Clin Genitourin Cancer. 2015;13(3):225–230. | ||
Adibi M, Thomas AZ, Borregales LD, et al. Percentage of sarcomatoid component as a prognostic indicator for survival in renal cell carcinoma with sarcomatoid dedifferentiation. Urol Oncol. 2015;33(10):427.e17–427.e23. | ||
Molina AM, Tickoo SK, Ishill N, et al. Sarcomatoid-variant renal cell carcinoma: treatment outcome and survival in advanced disease. Am J Clin Oncol. 2011;34(5):454–459. | ||
Wang Z, Kim TB, Peng B, et al. Sarcomatoid renal cell carcinoma has a distinct molecular pathogenesis, driver mutation profile, and transcriptional landscape. Clin Cancer Res. 2017;23(21):6686–6696. | ||
Malouf GG, Ali SM, Wang K, et al. Genomic characterization of renal cell carcinoma with sarcomatoid dedifferentiation pinpoints recurrent genomic alterations. Eur Urol. 2016;70(2):348–357. | ||
Keskin SK, Msaouel P, Hess KR, et al. Outcomes of patients with renal cell carcinoma and sarcomatoid dedifferentiation treated with nephrectomy and systemic therapies: comparison between the cytokine and targeted therapy eras. J Urol. 2017;198(3):530–537. | ||
Conant JL, Peng Z, Evans MF, Naud S, Cooper K. Sarcomatoid renal cell carcinoma is an example of epithelial–mesenchymal transition. J Clin Pathol. 2011;64(12):1088–1092. | ||
Voss MH, Bastos DA, Karlo CA, et al. Treatment outcome with mTOR inhibitors for metastatic renal cell carcinoma with nonclear and sarcomatoid histologies. Ann Oncol. 2014;25(3):663–668. | ||
van Poppel H, Becker F, Cadeddu JA, et al. Treatment of localised renal cell carcinoma. Eur Urol. 2011;60(4):662–672. | ||
Choueiri TK, Motzer RJ. Systemic therapy for metastatic renal-cell carcinoma. N Engl J Med. 2017;376(4):354–366. | ||
Motzer RJ, Hutson TE, Cella D, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369(8):722–731. | ||
Golshayan AR, George S, Heng DY, et al. Metastatic sarcomatoid renal cell carcinoma treated with vascular endothelial growth factor-targeted therapy. J Clin Oncol. 2009;27(2):235–241. | ||
Kunene V, Miscoria M, Pirrie S, Islam MR, Afshar M, Porfiri E. Sarcomatoid renal cell carcinoma: clinical outcome and survival after treatment with sunitinib. Clin Genitourin Cancer. 2014;12(4):251–255. | ||
Korenbaum C, Pierard L, Thiéry A, et al. Treatments, outcomes, and validity of prognostic scores in patients with sarcomatoid renal cell carcinoma: a 20-year single-institution experience. Clin Genitourin Cancer. 2018;16(3):e577–e586. | ||
Paner GP, Stadler WM, Hansel DE, Montironi R, Lin DW, Amin MB. Updates in the eighth edition of the tumor-node-metastasis staging classification for urologic cancers. Eur Urol. 2018;73(4):560–569. | ||
Ljungberg B, Alamdari FI, Stenling R, Roos G. Prognostic significance of the Heidelberg classification of renal cell carcinoma. Eur Urol. 1999;36(6):565–569. | ||
Störkel S, Eble JN, Adlakha K, et al. Classification of renal cell carcinoma: Workgroup No. 1. Union Internationale Contre le Cancer (UICC) and the American Joint Committee on Cancer (AJCC). Cancer. 1997;80(5):987–989. | ||
Wang Z, Xie H, Guo L, et al. Prognostic and clinicopathological value of Ki-67/MIB-1 expression in renal cell carcinoma: a meta-analysis based on 4579 individuals. Cancer Manag Res. 2017;9:679–689. | ||
Haas NB, Lin X, Manola J, et al. A phase II trial of doxorubicin and gemcitabine in renal cell carcinoma with sarcomatoid features: ECOG 8802. Med Oncol. 2012;29(2):761–767. | ||
Lopez-Beltran A, Scarpelli M, Montironi R, Kirkali Z. 2004 WHO classification of the renal tumors of the adults. Eur Urol. 2006;49(5):798–805. | ||
Cheville JC, Lohse CM, Zincke H, et al. Sarcomatoid renal cell carcinoma: an examination of underlying histologic subtype and an analysis of associations with patient outcome. Am J Surg Pathol. 2004;28(4):435–441. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.