Back to Journals » Clinical Ophthalmology » Volume 8
Isolated posterior capsular rupture following blunt head trauma
Authors Mansour A , Jaroudi M, Hamam R, Maalouf F
Received 9 September 2014
Accepted for publication 23 September 2014
Published 28 November 2014 Volume 2014:8 Pages 2403—2407
DOI https://doi.org/10.2147/OPTH.S73990
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Ahmad M Mansour, Mahmoud O Jaroudi, Rola N Hamam, Fadi C Maalouf
Department of Ophthalmology, American University of Beirut, Beirut, Lebanon
Abstract: Closed-globe traumatic cataract is not uncommon in males in the pediatric age group. However, there is a relative paucity of literature on isolated posterior lens capsule rupture associated with closed-globe traumatic cataract. We report a case of a 6-year-old boy who presented with white cataract 1 day after blunt trauma to the forehead associated with posterior capsular rupture that was detected by B-scan ultrasonography preoperatively. No stigmata of trauma outside the posterior capsule could be detected by slit-lamp exam, funduscopy, and optical coherence tomography. Phacoemulsification with posterior chamber intraocular lens implant was performed 24 hours after trauma, with the patient achieving 6/6 visual acuity 1 week and 6 months after surgery. Our case is unique, being the youngest (amblyogenic age) to be reported, with prompt surgical intervention, and with no signs of trauma outside the posterior capsule.
Keywords: posterior capsule rupture, forehead trauma, traumatic cataract, pediatric cataract
Introduction
Blunt ocular trauma frequently leads to damage of the cornea, lens, and retina. However, there is scarce literature1–15 on isolated posterior lens capsule rupture (PCR) following blunt ocular trauma. We present the case of a child who developed an isolated oval defect in the posterior lens capsule after blunt trauma with rapid cataract formation.
Case report
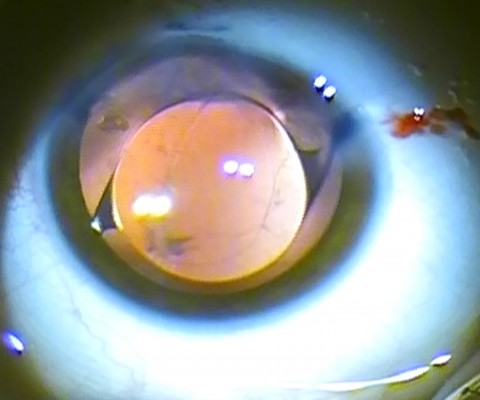
Our case is a 6-year-old boy who sustained direct minor trauma to the left forehead. He was playing at home with his sister and swirling in a circular fashion when he slipped and hit his forehead against the ground. The following day, he reported blurring of vision in the left eye and his parents noticed a white left pupil. Twenty-four hours following the incident, examination of the right eye was normal and the left eye had hand motion vision. Intumescent cataract was evident by slit-lamp examination (Figure 1). The cornea was clear, the anterior chamber was deep and quiet, the pupil was round and reactive, and the anterior lens capsule was intact. Intraocular pressure measured 14 mmHg in the right eye and 16 mmHg in the left eye. Gonioscopy revealed a normal angle without angle recession. The media opacity precluded exam of the posterior segment. B-scan revealed a flat retina, quiet vitreous, and a breached posterior capsule centrally (Figure 2). Computerized tomography scan of brain was negative for skull fracture or intracranial bleed. Since the patient was in the amblyogenic age, cataract surgery was performed within hours of presentation.
  | Figure 1 Mature white cataract of the left eye 1 day after blunt trauma to the forehead. |
  | Figure 2 Posterior capsular defect (arrow) is evident by B-scan of the left eye. |
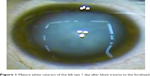
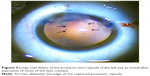
Surgery was started with trypan blue staining of anterior capsule, anterior circular capsulorhexis, and avoiding hydrodissection to prevent expansion of PCR. Slow aspiration of lens matter with the phacoemulsification probe was performed under low settings of bottle height, irrigation, and aspiration. After aspiration of two-thirds of the lens content, a very large, oval-shaped central posterior capsular rent was exposed (Figure 3). Anterior vitrectomy was performed, followed by cortex aspiration with the vitrector. Although one-piece foldable intraocular lens implantation in the capsular bag was initially thought feasible, the intraocular lens had a tendency to dislodge into the vitreous cavity, necessitating subsequent fixation in the sulcus without further optic capture (Figure 4). Intracameral carbachol was applied at the end of the surgery. One week postoperatively, uncorrected visual acuity was 6/6 (20/20). The patient had normal funduscopy and spectral-domain optical coherence tomography of the posterior pole. Visual acuity stabilized at 6/6 (20/20) over 14 months of follow-up with well-centered intraocular implant.
  | Figure 3 Large oval defect of the posterior lens capsule of the left eye as noted after aspiration of most of the lens content. |
  | Figure 4 Well-centered acrylic intraocular lens placed in the sulcus at the end of surgery. |
Discussion
Isolated PCR in the event of blunt trauma appears rarely (Table 1).1–15 Our patient presented unique features that differ from those reported in the literature (Table 1) in several respects: he is the youngest patient in the literature (6 years) with PCR; his visual loss was rapid in onset and very severe to the level of hand motion (unlike a gradual decrease in other cases); he underwent “immediate” (24 hours after trauma) surgery to prevent amblyopia (unlike the several days to weeks in other cases); and his ocular findings were uniquely restricted to PCR with absence of iritis, hyphema, Vossius ring, iris sphincter tear, angle recession, or posterior pole trauma (funduscopic and tomographic).
PCR can be diagnosed preoperatively by B-scan ultrasonography.6 Echography with a 20 MHz probe was found to be an accurate and sensitive imaging modality for detection of PCR in a large series of traumatic cataracts (41 open-globe injuries and two closed-ocular injuries).13 Other diagnostic modalities, such as Scheimpflug imaging, can be especially helpful in delineating the extent of PCR, amount of residual nucleus and cortex, and presence or absence of vitreous prolapse in the anterior chamber.8
When PCR occurs, management depends on several parameters, such as the extent and location of the tear, the amount of residual nucleus and cortex, and the presence of vitreous in the anterior chamber. Traditionally, pars plana lensectomy was the preferred approach for managing such cases.1–3 More recently, surgeons have adopted a method involving a clear corneal incision, phacoemulsification, and intraocular lens implantation in the capsular bag, with excellent visual outcome.7,9,11 Pars plana vitrectomy with lensectomy is reserved for cases of extensive posterior capsular rupture, marked vitreous prolapse, or significant zonular instability.
The mechanism of blunt trauma-induced blowout PCR in children can be explained by a combination of forces (Table 2; Figure 5):10,16 1) equatorial elongation of the globe following blunt trauma leads to stretch of zonules and posterior capsule; 2) anteroposterior vector force to the posterior capsule from direct trauma; 3) preferential rupture of elastic posterior capsule because the zonules are strong in children.7 We postulate that the anatomy of the bony orbit around the globe might play a pivotal protective role in cases of head trauma. Our patient had a shallow orbital rim, making the globe more vulnerable to injury upon direct forehead trauma.
  | Table 2 Proposed mechanisms for isolated posterior capsular rupture following forehead trauma |
This case of isolated PCR and 17 cases in the literature establish PCR as a distinct clinical entity with diagnostic echographic findings, special surgical management strategy, and good visual outcome.1–11,14,15
Acknowledgments
Written informed consent was obtained from the patient’s family for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
Author contributions
AMM made substantial contributions to conception and design; MOJ made substantial contributions to acquisition, analysis, and interpretation of data; RNH and FCM was involved in initial conception and data collection. All authors were involved in drafting the manuscript and revising it critically for important intellectual content, and all authors gave final approval of the version to be published.
Disclosure
The authors report no conflicts of interest in this work.
References
Yasukawa T, Kita M, Honda Y. Traumatic cataract with a ruptured posterior capsule from a nonpenetrating ocular injury. J Cataract Refract Surg. 1998;24:868–869. | ||
Rao SK, Parikh S, Padhmanabhan P. Isolated posterior capsule rupture in blunt trauma: pathogenesis and management. Ophthalmic Surg Lasers. 1998;29:338–342. | ||
Thomas R. Posterior capsule rupture after blunt trauma. J Cataract Refract Surg. 1998;24:283–284. | ||
Rosen WJ, Campbell DG. Posterior capsule rupture after a paint-pellet injury. J Cataract Refract Surg. 2000;26:1422–1423. | ||
Lee SI, Song HC. A case of isolated posterior capsule rupture and traumatic cataract caused by blunt ocular trauma. Korean J Ophthalmol. 2001;15:140–144. | ||
Li KK, Groenewald C, Wong D. Management of traumatic posterior capsular rupture: corneal approach with high speed vitrector. J Cataract Refract Surg. 2005;31:1666–1668. | ||
Por YM, Chee SP. Implantation of foldable intraocular lens with anterior optic capture in isolated posterior capsule rupture. J Cataract Refract Surg. 2006;32:707–708. | ||
Grewal DS, Jain R, Brar GS, Grewal SP. Scheimpflug imaging of pediatric posterior capsule rupture. Indian J Ophthalmol. 2009;57:236–238. | ||
Pavlovic S. Epilenticular intraocular lens implantation in traumatic cataract with a ruptured posterior capsule. Am J Ophthalmol. 2000;130:352–353. | ||
Campanella PC, Aminlari A, DeMaio R. Traumatic cataract and Wieger’s ligament. Ophthalmic Surg Lasers. 1997;28:422–423. | ||
Pushker N, Sony P, Khokhar S, Vardhan P. Implantation of foldable intraocular lens with anterior optic capture in isolated posterior capsule rupture. J Cataract Refract Surg. 2005;31:1457–1458. | ||
Angra SK, Vajpayee RB, Titiyal JS, Sharma YR, Sandramouli S, Kishore K. Types of posterior capsular breaks and their surgical implications. Ophthalmic Surg. 1991;22:388–391. | ||
Tabatabaei A, Kiarudi MY, Ghassemi F, et al. Evaluation of posterior lens capsule by 20 MHz ultrasound probe in traumatic cataract. Am J Ophthalmol. 2012;153:51–54. | ||
Saika S, Kin K, Ohmi S, Ohnishi Y. Posterior capsule rupture by blunt ocular trauma. J Cataract Refract Surg. 1997;23:139–140. | ||
El-Gendy A, Rahman I, Mahmood U, Nylander A. Traumatic rupture of the posterior capsule resulting in complete posterior prolapse of the lens with subsequent resolution of high myopia. J Cataract Refract Surg. 2006;32:893–894. | ||
Wolter JR. Coup-contrecoup mechanism of ocular injuries. Am J Ophthalmol. 1963;56:785–796. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.