Back to Journals » Journal of Multidisciplinary Healthcare » Volume 12
Is aerobic exercise training during hemodialysis a reliable intervention for autonomic dysfunction in individuals with chronic kidney disease? A prospective longitudinal clinical trial
Authors Morais MJD , de Abreu LC , Santana de Oliveira F , Pinheiro Bezerra IM , Raimundo RD , Paulo Martins Silva R , Valenti VE , Pérez-Riera AR
Received 25 January 2019
Accepted for publication 19 June 2019
Published 27 August 2019 Volume 2019:12 Pages 711—718
DOI https://doi.org/10.2147/JMDH.S202889
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mauro José de Deus Morais,1–3 Luiz Carlos de Abreu,2–4 Fabiano Santana de Oliveira,1–3 Italla Maria Pinheiro Bezerra,2,3,5 Rodrigo Daminello Raimundo,3 Romeu Paulo Martins Silva,1 Vitor Engracia Valenti,6 Andrés Ricardo Pérez-Riera2,3
1Centro de Saúde e Desporto, Universidade Federal do Acre, Rio Branco, Acre, Brazil; 2Laboratório de Delineamento em Pesquisas e Escrita Científica, Centro Universitário Saúde ABC Santo André, São Paulo, Brazil; 3Laboratório de Delineamento em Pesquisas e Escrita Científica, Escola Superior de Ciências da Santa Casa de Misericórdia de Vitória, Vitória, Espirito Santo, Brazil; 4Graduate Entry Medical School, University of Limerick, Limerick V94 T9PX, Ireland; 5Escola Superior de Ciências da Santa Casa de Misericórdia, EMESCAM, Vitória, Brazil; 6Centro de Estudos do Sistema Nervoso Autônomo, State University of São Paulo, Marília, São Paulo, Brazil
Correspondence: Mauro José de Deus Morais
Centro de Saúde e Desporto, Universidade Federal do Acre, Rua Gumercindo, nº 292, Bairro: Universitário, Rio Branco 69.917.698, Acre, Brazil
Tel +55 6 899 971 6122
Email [email protected]
Italla Maria Pinheiro Bezerra
Escola Superior de Ciências da Santa Casa de Misericórdia, EMESCAM, Bolsista Capes Brasil, Vitória, Rio Branco 69.915-900, Brazil
Tel +55 2 799 253 4941
Email [email protected]
Introduction: Physical exercises help in the rehabilitation and recovery of various diseases. Cardiovascular and hypertension problems are the main causes of people being affected by kidney problems, which as a consequence, affects the heart rate variability (HRV) of the individual. Physical activity developed in a well-planned and thorough way can be a component in the treatment of this problem.
Objective: We aimed to evaluate the effects of aerobic exercise intervention during hemodialysis on autonomic heart rate regulation in individuals with chronic kidney disease (CKD).
Methods: This was a longitudinal trial conducted in 19 CKD patients. The patients underwent three weekly sessions of aerobic exercise during hemodialysis for 30 mins for 12 weeks (three months).
Results: HRV was analyzed before and after the protocol training. Linear indices of HRV were not different between before and after the protocol training. Nonlinear HRV analysis indicated reduced values of determinism (p=0008, Cohen’s d=0.82) and entropy (p=003, Cohen’s d=0.84) after the training protocol.
Conclusion: In conclusion, aerobic exercise training during hemodialysis did not improve autonomic control of heart rate in CKD patients.
Keywords: autonomic nervous system, cardiovascular system, exercise, kidney diseases, renal dialysis
Introduction
Chronic noncommunicable diseases (NCDs) are a global health problem and a threat to health and human development. Among them, we have as main diseases Diabetes, Hypertension, Cardiorespiratory Diseases and Chronic Kidney Disease. The burden of these diseases falls particularly on low- and middle-income groups.1,2
Chronic diseases have motivated the scientific community to develop studies that verify the impact of these diseases on the Quality of Life (QoL) of the population. Among these diseases is Chronic Kidney Disease (CKD), currently known as Chronic Renal Insufficiency (CRF), which is characterized by the progressive, almost always irreversible, loss of kidney function.3 CKD is a disease that compromises a high percentage of the population and is considered a great public health problem because of its high mortality rates. Its chronicity causes organic alterations, psychic and social dysfunctions, significantly interfering in the QoL of the carriers. In view of the diagnosis, there are three therapeutic modalities to be adopted, respectively: hemodialysis, peritoneal dialysis and renal.4,5
There are several factors associated with the renal population, such as: low functional capacity; low cardiopulmonary capacity; high rates of mortality and morbidity, associated diseases of hypertension, diabetes, cardiorespiratory, etc.6,7
Mortality is high in patients in chronic hemodialysis with cardiovascular disease, and many die suddenly. Moreover, there is a very close relationship between CKD and systemic hypertension, where this may affect the cardiovascular system, and consequently cardiac autonomic modulation dysfunction, with a predominance of sympathetic autonomic modulation.8 Unregulated ANS is present in hemodialysis patients because it directly targets several vital organs, and can even lead to death in cardiac complications.8,9
In this sense, cardiac autonomic regulation may be evaluated through heart rate (HR) variability (HRV), which is a conventionally accepted term to describe the fluctuations regarding intervals between consecutive heart beats (RR intervals), that are related to influences by the ANS on the sinus node. This is a noninvasive technique, the analysis of which could be made using linear methods, on the time and frequency domain; and non-linear, in the chaos domain.10,11
Reduced HRV is an increased risk of death in several populations, but its prognostic value in patients with hemodialysis remains uncertain.9 Literature has investigated the existing relationship between HRV in patients carriers of CKD who undergo hemodialysis, and observed that high mortality is related to an erroneous functioning of cardiac autonomic regulation.12
The significant reduction of functional capacity in patients carriers of CKD in hemodialysis has been partially reversed with the regular practice of aerobic physical exercises.13 Well-developed physical activity can bring many benefits, both for healthy individuals, and in the process of prevention or rehabilitation of diseases, strengthening the musculoskeletal system, cardiorespiratory system, as well as improving the quality of life, including those with chronic kidney disease, according to the NKF.14,15
The risks for cardiovascular, cardiorespiratory, musculoskeletal problems, as well as the increase in functional capacities and improvement in the social and psychological aspects improve with the accomplishment of physical training carried out correctly in healthy people.15,16 There are several reports that despite the development of physical exercises in renal patients, they nonetheless present a compromised side due to the consequences that the disease brings to this population. But similar benefits have already been identified, taking into account the particularities of each individual, as well as the time of treatment.17,18
There are already many studies on the fight and control of renal disease, that attempt to identify pre-existing problems and others that may appear in the future. New research must continue to be carried out so that the solution to the disease is discovered, trying to avoid its worsening.3
Therefore, this study is aimed at evaluating the effects of aerobic exercise intervention during hemodialysis in the autonomic control of heart rate in individuals with chronic kidney disease: a prospective longitudinal clinical trial.
Methods
Study design
This is a descriptive, prospective and longitudinal trial, performed in 40 CKD patients in treatment at the Hospital das Clinicas of the Municipality of Rio Branco, State of Acre who were in hemodialysis treatment.
This study was approved by Resolution n° 466/12 by the National Council of Health. We obtained the approval by the Committee on Ethics on Research of the Faculdade de Juazeiro do Norte, (n° 1,962,092). All patients that agreed to participate in the research signed the informed consent. This trial is registered in the Registro Brasileiro de Ensaios Clínicos (Brazilian registry of clinical Trials; http://www.ensaiosclinicos.gov.br/rg/RBR-7354r6/, number RBR-7354r6, UTN Number: U1111-1216-8272). The resolution, as well as the registration of the clinical trial, follow the guidelines of the Declaration of Helsinki.
Inclusion criteria
Ambulatory patients of both sexes, who were literate, were included, with a minimum age of 18 years and a maximum of 65 years. Adult patients of both sexes who have not been physically active for at least six months were included. Patients who had been on treatment for at least six months and were clinically licensed by the physician responsible for the sector, as well as patients who were taking coincidental medications.
Exclusion criteria
We excluded patients whose RR interval recordings presented more than 5% of artifacts and those who, for any reason, could not participate in all the protocol stages within the agreed terms (Figure 1). Patients with diabetes mellitus, unstable angina, uncontrolled hypertension (systolic blood pressure, SBP: 200 mmHg and/or diastolic blood pressure, DBP: 100 mmHg), use of antiarrhythmic drugs, severe lung diseases, acute systemic infection, osteodystrophy renal impairment, disabling neurological and musculoskeletal disorders.
 |
Figure 1 Flow chart of sample loss in the study. Of the total of 248 patients, there were 208 patients included. |
Experimental protocol
Initially, the sample consisted of 40 adult patients, but we ended up with 19 patients (Figure 1), who had CKD and were under hemodialysis treatment. Patients underwent three weekly sessions of aerobic exercise performed during hemodialysis sessions in the first two hours lasting 30 mins for 12 weeks (three months).19
Forty volunteers were selected. Over the course of the development of aerobic activities, we had three deaths. There were then 37 volunteers, but a further three volunteers underwent kidney transplantation (exclusion criterion). Four volunteers gave up performing the exercises. The volunteer patients were selected only within the first two hours of the hemodialysis session, which corresponded from 5:00 a.m. to 9:30 a.m. (first hour), and from 10 a.m. to 2.30 p.m. (second hour); thus, we had 3 patients who transferred their sessions of hemodialysis to the third shift, which corresponded to the time from 3:00 p.m. to 7:30 p.m. And to conclude, we had eight volunteers excluded at the end of the survey because the artifacts were above 5%, thus presenting an exclusion factor.19
After the enrollment of patients, according to the previously established specific criteria, all underwent HR monitoring by a portable device (Polar RS 800 CX) that allowed storing these data for the subsequent analysis of HRV.19
Initially, the short version of the IPAQ questionnaire was applied, to identify the level of physical activity that the patients practiced at the time.20
Simultaneously, we applied an adapted quality of life QV questionnaire.21 The latter was constituted by 14 multiple-choice questions (5 options), where the first six questions dealt with the quality of life QV of patients before starting the bicycle ergometer program. The other questions identified subjectively, the improvements the patients had reached after the intervention. In the case of this questionnaire, they were applied to 26 patients that were part of the investigation, since specifically in this case, we were evaluating the subjective response of the benefits of aerobic physical exercise in bicycle ergometer. Soon after this phase, the patients were analyzed in the components of Heart Rate Variability, where we had another eight patients excluded from the research because they had artifacts above 5%, falling within the exclusion criteria of the research. Thus, we took advantage of the responses of the 26 patients who answered the subjective questionnaire on the benefits of aerobic exercise, and we ended up with an HRV analysis with 19 patients.
The HRV evaluation was made within the two initial hours of hemodialysis, with a total duration of one hour. A bicycle ergometer was used (Mini Bike Compact – E14) to perform the aerobic exercise, measuring 49×41.5×34.5 m (height x length x width).19
The resting phase had a 10 min duration. In this stage, the patient was guided to remain as relaxed as possible in the stretcher. The intervention stage elapsed over a 30 min period. The patients performed the aerobic exercises with cycling movements of the lower limbs with 45–60% of estimated maximum HR (%HR, 208–0.7 x age).22 They were asked to remain with their arms stretched usually at the length of the hips, at the sides of the body, arranged the best way possible. They started with the tolerated time and were stimulated to increase the intensity so that it would reach the established area, and it was even possible for them to exceed the upper limit until reaching the intervention time. The load was prescribed, taking into consideration the Karvonen formula, a recovery phase, that lasted for 20 mins, during which the patients were instructed to remain as relaxed as possible. These analyses were performed at the beginning of the patient selection and after three months of aerobic exercise.19
In all stages, the supplementary data of patients were collected from their clinical histories, filled in by the medical team of the hospital (body mass index, height, weight, age, gender, blood pressure, and heart rate measurement).
The criteria for interrupting the aerobic exercise included intense physical tiredness, chest pain, dizziness, pallor, fainting, tachycardia, hypotension, and lower limb fatigue, interdialytic weight gain greater than 5 kg, difficulty of vascular access and any significant complaint (pain, dyspnea, etc.), before or during training. In these cases, they were prevented from performing the exercise that day or while such alterations persisted, or according to the medical prescription of the sector. Resting HRV was evaluated before and two days after exercise training protocol in a supine position under spontaneous breathing.19
HRV analysis
For the analysis of heart rate variability (HRV), we placed the recording stripes in the chest and the pulse watch of patients. The heart rate receptor (RS800CX, Polar Electro, Finland) was validated to locate the heart beat for the analysis of HRV.19
After the recording, the signal reached was filtered to remove artifacts by the Polar Precision Performance software (version 4.01.029), and only the series with more than 95% of sinus beats were included in the study. At the time, manual filtering was fulfilled, which involved a visual inspection and the bookbinding of the RR intervals.
HRV was analyzed in the time (RMSSD – root-mean-square differences of successive R-R intervals) and frequency (HF – high frequency: 0.15–0.40 Hz) domains. Nonlinear analysis of HRV included the quantitative Poincaré plot (SD1 – standard deviation of the instantaneous variability of the beat-to-beat heart rate), symbolic (0V and 2UV), and recurrence analysis. We did not use analysis low-frequency index since it has been repeatedly demonstrated to be theoretically flawed and empirically unsupported.23–29
The SD1 index, time and frequency domain HRV measurements were estimated using the Kubios HRV software (Biomedical Signal Analysis Group, Department of Applied Physics, University of Kuopio, Finland) (Tarvainen et al, 2014). Symbolic HRV analysis was performed through CardioSeries®v2.4 (Ribeirao Preto, SP, Brazil) and recurrence analysis was performed by using Visual Recurrence Analysis software (Institute for Mathematics and its Applications, Finland)
Statistical analysis
The normality of the groups was estimated by the Shapiro-Wilk test. When the sets of data were normally distributed, we used the paired Students’ t-test. For non-parametric distributions, we applied the Wilcoxon test.
To compared HRV before and three months after exercise protocol training, the paired Students’ t-test was applied for parametric distributions and the Wilcoxon test for non-parametric distributions. Statistical significance was considered a level of p<0.05 (or 5%).
We calculated the effect size for significant differences; we considered a large effect size for Cohen’s d >0.8 and medium effect size for values between 0.8 and 0.5.
Results
We finished the investigation with 19 patients, mean and standard deviation of diastolic (DBP) and systolic blood pressure (SBP), weight, height, age, and body mass index (BMI) of patients are presented in Table 1.
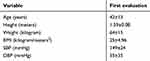 |
Table 1 Diastolic blood pressure (DBP) and systolic blood pressure (SBP), weight, height, age and body mass index (BMI) of patients |
About the results of the short version of the International Physical Activity Questionnaire (IPAQ), we had the following results: patients considered active (n-8 42.1%), irregularly active patients (n-5, 26.3%) and sedentary patients (n-6, 31.6%). Considering that irregularly active and sedentary are considered a very low classification according to the evaluation criteria of the questionnaire, we had 57.9% of patients with a classification below the expectations.
About the adapted quality of life QV questionnaire, all the interviewed patients, 100%, replied that they improved their health in some aspect after the intervention, as they increased their day-to-day disposition. They reported their musculoskeletal pain decreasing, such as headaches/sore eyes, their back, arms/legs, fists/hands. We noticed that 88% also reported improvements in their humor, and increase in appetite.
We performed linear analysis of HRV and also evaluated possible differences between before and after training exercise regarding RR interval and HR. According to Figure 2, we observe no significant difference between before and after the exercise training protocol regarding resting RR interval, HR, RMSSD, and HF.
Figure 3 displays data concerning the nonlinear analysis of HRV based on the Poincaré plot, symbolic and recurrence analysis. We observed that Determinism and Entropy values were significantly increased after exercise protocol training with large effect size.
 |
Figure 3 Mean values and respective standard deviations of nonlinear analysis of HRV. Abbreviation: SD1, standard deviation of the instantaneous variability of the beat-to-beat heart rate. |
Discussion
This study was undertaken to analyze the effects of aerobic exercise training during hemodialysis on the autonomic modulation of heart rate in patients with CKD. As the main finding, we did not notice the significant influence of exercise on linear analysis of HRV. On the other hand, although we evidenced the positive influence of exercise training on pain, the non-linear analysis showed that exercise training did not prevent HRV worsening in three months.
The risks for cardiovascular, cardiorespiratory and musculoskeletal problems, as well as, the increase of the functional capacities and improvement in the social and psychological aspects improve with the accomplishment of physical training carried out correctly in healthy individuals.30,31 There are several reports that despite the development of physical exercises, renal patients present a compromised side due to the consequences that the disease brings to this population. Nevertheless, similar benefits have already been identified, taking into account the particularities of each individual, as well as the time of treatment.30
Unregulated ANS is present in hemodialysis patients because it directly targets several vital organs, and can even lead to death in cardiac compromise.8,9 One of the main causes of ANS imbalance in renal patients is related to cardiovascular problems.8,9,12 HRV is greatly impaired in its normal functioning when it is related to cardiac arrhythmias associated with these patients.8,9,12 In this case, the organism is directly affected in all its systems: nervous, cardiovascular, respiratory, musculoskeletal, immunological and endocrine/metabolic.8,9,12
Our investigation focused on exercise as a complementary therapy for CKD treatment. Patients with CKD have several compromised functions, as well as restrictions on both the food portion and the physical part, compared with healthy people. Thus, the development of physical exercise programs generates a greater difficulty to be performed, mainly by the patient.18 Even so, the positive effects that the physical exercises can generate in the treatment of this population are already demonstrated, working both in the prevention and in the fight against the disease in the most advanced phase.32
In this context, we noted no significant positive influence of exercise during hemodialysis on linear analysis of HRV. An investigation conducted during twelve weeks with supervised aerobic training during hemodialysis sessions in CKD patients verified that there were no modifications on HRV and there was no promotion of significant improvement on left ventricular function, although there were good results on the wellbeing of patients.17
A previous review4 reported that exercise protocol improves functional capacity, providing cardiorespiratory and muscle benefits in CKD patients. They also showed that exercise improves aerobic capacity and physical conditioning, decrease of fatigue and anxiety, improvement of muscle capillarization, and blood pressure at rest, increase in time of duration of exercise and improvement on urea purification.
Chigira et al, (2017) performed an intervention study with exercise during hemodialysis in elderly patients for three months. On the other hand, there was a significant difference in the WHO-QOL26 score.14 Corroborating the results aforementioned, Picariello et al, (2017) investigated the social and psychological interventions on the effectiveness of fatigue reduction in CKD. A significant improvement was identified on fatigue after psychological and social interventions.14,33
Corroborating the results quoted above, a study30 pointed out significant improvements in muscle function and physical performance measures, after the result of physical resistance training and a low rate of work in patients with CKD.
A study that evaluated the correlation of HRV during ergometer test to an aerobic deficit in patients in hemodialysis found a strong correlation between aerobic deficit with HRV (SDNN) during exercise. This association was independent from age, gender, body mass index, smoking, diabetes, and use of beta blockers or clonidine, but not from hemoglobin levels.12
Our data was also based on nonlinear HRV analysis. This is because HRV presents a complex and variable behavior over time, and it is advisable to make the identification of behavior patterns by proper methods. One of the indicators that we made had as a basis the use of the so-called Recurrence Plot. This technique is extensively used nowadays, on the analysis of complex signals, which can be analyzed by the introduction of the so-called quantifiers, which enable the quantification of the analyzed signal behavior.34
Recurrence plot is used in the study of time-dependence of a series, a probability of a state occurring in phase space; i.e., in the study of their stationaries signals.35 In the analysis of experimental time series of heart rate, for time series of healthy individuals, Recurrence plot has a diagonal line and less apparent squares, indicating a higher HRV. In a series of individuals that present a pathology, Recurrence plot shows more squares in the graph indicating inherent periodicity and a low HRV.34,35
In this regard, according to our results, the analysis of HRV recurrence showed that resting HRV decreased after 12 weeks of exercise training. This indicates that the ANS is in worst conditions compared to before the training protocol. Conversely, aerobic exercise in bicycle ergometer provides not only an improvement in cardiopulmonary capacity and resistance but also corroborates the decrease in fatigue, as well as an increase in muscle strength.30 Aerobic exercise provides an improvement in aerobic function and other beneficial effects such as an increase in motor unit recruitment, favoring the development of muscle fibers.34
Several studies have demonstrated positive results when work was done relating the implementation of physical activity programs in renal patients, demonstrated a safe resource, as well as, assisting in the physiological and subjective responses of this population, improving their life.30,36,37
All scientific research that applies some protocol must follow clear and defined standards, following rules and guidelines of reliable concepts, to achieve a correct and real result.38 The study, when applying the instrument for analysis of HRV, obtained interesting results with renal patients, as it promoted favorable physiological adaptations, leading to a better quality of life. In this way, a protocol of physical exercise well prepared and safe can contribute to an improvement of this population in its physical, nutritional, social, and affective aspects. Nevertheless, in this specific population of CKD patients, our results showed that aerobic physical training was not able to improve autonomic function.
Conclusion
In conclusion, aerobic exercise training during hemodialysis did not improve autonomic control of heart rate in CKD patients. Complex behavior of HR dynamics worsened three months after aerobic exercise training.
Data availability
The authors intend to share data from identified individual participants. If necessary, the data will be available from the corresponding authors, however always respecting the resolution focused on research with human beings. The data will be available for a period of 5 years from the publication of the manuscript via contact with the corresponding authors.
Acknowledgment
We thank the Faculty of Medicine of the ABC of Santo André for having allowed us to develop research that we believe will be of great relevance in the scientific field.
Disclosure
The authors declare no conflicts of interest associated with the collection, dissemination, or interpretation of this research. The study is presented clearly, honestly, and without fabrication, falsification, or data manipulation.
References
1. World Health Organization. Preventing chronic diseases: a vital investment: WHO global report; 2005. ISBN 92 4 156300 1.
2. Heiwe S, Clyne N, Dahlgren MA. Living with chronic renal failure: patients’ experiences of their physical and functional capacity. Physiother Res Int. 2003;8(4):167–177.
3. Bastos MG, Kirsztajn GM. Chronic kidney disease: importance of early diagnosis, immediate referral and structured interdisciplinary approach to improve outcomes in patients not yet on dialysis. J Bras Nefrol. 2011;33(1):93–108.
4. Bohm J, Monteiro MB, Thome FS. [Effects of aerobic exercise during haemodialysis in patients with chronic renal disease: a literature review]. J Bras Nefrol. 2012;34(2):189–194.
5. Seidl EM, Zannon CM. [Quality of life and health: conceptual and methodological issues]. Cad Saude Publica. 2004;20(2):580–588.
6. Knight EL, Ofsthun N, Teng M, Lazarus JM, Curhan GC. The association between mental health, physical function, and hemodialysis mortality. Kidney Int. 2003;63(5):1843–1851. doi:10.1046/j.1523-1755.2003.00931.x
7. Sietsema KE, Amato A, Adler SG, Brass EP. Exercise capacity as a predictor of survival among ambulatory patients with end-stage renal disease. Kidney Int. 2004;65(2):719–724. doi:10.1111/j.1523-1755.2004.00411.x
8. Fukuta H, Hayano J, Ishihara S, et al. Prognostic value of heart rate variability in patients with end-stage renal disease on chronic haemodialysis. Nephrol Dial Transplant. 2003;18(2):318–325. doi:10.1093/ndt/18.2.318
9. Hayano J, Takahashi H, Toriyama T, et al. Prognostic value of heart rate variability during long-term follow-up in chronic haemodialysis patients with end-stage renal disease. Nephrol Dial Transplant. 1999;14(6):1480–1488. doi:10.1093/ndt/14.6.1480
10. Vanderlei LC, Pastre CM, Hoshi RA, Carvalho TD, Godoy MF. Basic notions of heart rate variability and its clinical applicability. Revista Brasileira de Cirurgia Cardiovascular. 2009;24(2):205–217. doi:10.1590/s0102-76382009000200018
11. Giacon TR, Vanderlei FM, Da Silva AKF, Da Silva NT, Valenti VE, Vanderlei LCM. Influence of diabetes on autonomic function in children: analysis through the geometr ic indices. J Hum Growth Dev. 2016;26(1):81–87. doi:10.7322/jhgd.113728
12. Carreira MA, Nogueira AB, Pena FM, et al. Heart rate variability correlates to functional aerobic impairment in hemodialysis patients. Arq Bras Cardiol. 2015;104(6):493–500. doi:10.5935/abc.20150039
13. Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev. 2011;10:Cd003236.
14. Chigira Y, Oda T, Izumi M, Yoshimura T. Effects of exercise therapy during dialysis for elderly patients undergoing maintenance dialysis. J Phys Ther Sci. 2017;29(1):20–23. doi:10.1589/jpts.29.20
15. Ploeger HE, Takken T, de Greef MH, Timmons BW. The effects of acute and chronic exercise on inflammatory markers in children and adults with a chronic inflammatory disease: a systematic review. Exerc Immunol Rev. 2009;15:6–41.
16. Pinto VCM, Dos Santos PGMD, Souza FES, Dos Santos Simões TB, de Carvalho Dantas RPN, Cabral B. Maturational stages: comparison of growth and physical capacity indicators in adolescents. J Hum Growth Dev. 2018;28(1):42–49. doi:10.7322/jhgd.127411
17. Reboredo Mde M, Pinheiro Bdo V, Neder JA, et al. Effects of aerobic training during hemodialysis on heart rate variability and left ventricular function in end-stage renal disease patients. J Bras Nefrol. 2010;32(4):367–373.
18. Barcellos FC, Santos IS, Umpierre D, Bohlke M, Hallal PC. Effects of exercise in the whole spectrum of chronic kidney disease: a systematic review. Clin Kidney J. 2015;8(6):753–765. doi:10.1093/ckj/sfv099
19. Morais MJD, Raimundo RD, Oliveira FS, et al. Evaluation of the effects of aerobic training during hemodialysis on autonomic heart rate modulation in patients with chronic renal disease. Medicine. 2019;98(23):e15976. doi:10.1097/MD.0000000000015976
20. Matsudo S, Araújo T, Matsudo V, et al. International questionnaire of physical activity (ipaq): stupe of validity and reproducibility In Brazil. Braz J Phys Act Health. 2001;6(2):5–18.
21. Vilela Junior G, Leite N. Qualidade de vida e saúde: avaliação pelo QVS-80 [QVS-80 Quality of Life and Health Assessment Questionnaire]. In: IPES Editorial, editors. Qualidade de vida no ambiente corporativo. Edition 1. Barueri: Manole; 2008:71–80. Portuguese.
22. Tanaka H, Monahan KD, Seals DR. Age-predicted maximal heart rate revisited. J Am Coll Cardiol. 2001;37(1):153–156. doi:10.1016/s0735-1097(00)01054-8
23. Billman GE. The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Front Physiol. 2013;4:26. doi:10.3389/fphys.2013.00026
24. Houle MS, Billman GE. Low-frequency component of the heart rate variability spectrum: a poor marker of sympathetic activity. Am J Physiol. 1999;276(1 Pt 2):H215–23. doi:10.1152/ajpheart.1999.276.1.H215
25. Goldstein DS, Bentho O, Park MY, Sharabi Y. Low-frequency power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflexes. Exp Physiol. 2011;96(12):1255–1261. doi:10.1113/expphysiol.2010.056259
26. Hopf HB, Skyschally A, Heusch G, Peters J. Low-frequency spectral power of heart rate variability is not a specific marker of cardiac sympathetic modulation. Anesthesiology. 1995;82(3):609–619. doi:10.1097/00000542-199503000-00002
27. Heathers JA. Sympathovagal balance from heart rate variability: an obituary. Exp Physiol. 2012;97(4):556. doi:10.1113/expphysiol.2011.063867
28. Eckberg DL. Sympathovagal balance: a critical appraisal. Circulation. 1997;96(9):3224–3232. doi:10.1161/01.cir.96.9.3224
29. Reyes Del Paso GA, Langewitz W, Mulder LJ, van Roon A, Duschek S. The utility of low frequency heart rate variability as an index of sympathetic cardiac tone: a review with emphasis on a reanalysis of previous studies. Psychophysiology. 2013;50(5):477–487. doi:10.1111/psyp.12027
30. Storer TW, Casaburi R, Sawelson S, Kopple JD. Endurance exercise training during haemodialysis improves strength, power, fatigability and physical performance in maintenance haemodialysis patients. Nephrol Dial Transplant. 2005;20(7):1429–1437. doi:10.1093/ndt/gfh784
31. de Maio Nascimento M, Pereira LGD, Cordeiro PRN, de Araújo LMG. Comparison and agreement of criteria for the BMI classification of physically active elderly women living in the Backlands, semi-arid Region. J Hum Growth Dev. 2017;27(3):342–349. doi:10.7322/jhgd.128227
32. Gould DW, Graham-Brown MP, Watson EL, Viana JL, Smith AC. Physiological benefits of exercise in pre-dialysis chronic kidney disease. Nephrology (Carlton). 2014;19(9):519–527. doi:10.1111/nep.12285
33. Picariello F, Hudson JL, Moss-Morris R, Macdougall IC, Chilcot J. Examining the efficacy of social-psychological interventions for the management of fatigue in end-stage kidney disease (ESKD): a systematic review with meta-analysis. Health Psychol Rev. 2017;11(2):197–216. doi:10.1080/17437199.2017.1298045
34. de Godoy MF, Takakura IT, Correa PR, Machado MN, Miranda RC, Brandi AC. Preoperative nonlinear behavior in heart rate variability predicts morbidity and mortality after coronary artery bypass graft surgery. Med Sci Monit. 2009;15(3):Cr117–22.
35. Stuckey MI, Tulppo MP, Kiviniemi AM, Petrella RJ. Heart rate variability and the metabolic syndrome: a systematic review of the literature. Diabetes Metab Res Rev. 2014;30(8):784–793. doi:10.1002/dmrr.2555
36. Raimundo RD, de Abreu LC, Adami F, et al. Heart rate variability in stroke patients submitted to an acute bout of aerobic exercise. Transl Stroke Res. 2013;4(5):488–499. doi:10.1007/s12975-013-0263-4
37. de Rezende Barbosa M, Vanderlei LCM, Neves LM, et al. Impact of functional training on geometric indices and fractal correlation property of heart rate variability in postmenopausal women. Ann Noninvasive Electrocardiol. 2018;23(1):e12469. doi:10.1111/anec.2018.23.issue-1
38. de Araújo Moraes SDT. Scientific method and research in health: orientation for professional practice. J Hum Growth Dev. 2019;29(1):5–9. doi:10.7322/jhgd.157742
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

