Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Irrational Responses to Risk Preference Questionnaires by Patients with Diabetes with or without Retinopathy and Comparison with Those without Diabetes
Authors Emoto N , Soga A, Fukuda I, Tanimura-Inagaki K, Harada T, Koyano HM, Goto R, Sugihara H
Received 23 September 2020
Accepted for publication 15 November 2020
Published 14 December 2020 Volume 2020:13 Pages 4961—4971
DOI https://doi.org/10.2147/DMSO.S283591
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Naoya Emoto,1,2 Akimi Soga,1 Izumi Fukuda,1 Kyoko Tanimura-Inagaki,1 Taro Harada,1 Hajime M Koyano,3 Rei Goto,4 Hitoshi Sugihara1
1Department of Endocrinology, Diabetes and Metabolism, Graduate School of Medicine, Nippon Medical School, Tokyo, Japan; 2Diabetes & Thyroid Clinic, Sakura Chuo Hospital, Chiba, Japan; 3Division of Endocrinology and Diabetes, Juntendo University Urayasu Hospital, Chiba, Japan; 4Graduate School of Business Administration, Keio University, Kanagawa, Japan
Correspondence: Naoya Emoto
Diabetes & Thyroid Clinic, Sakura Chuo Hospital, 20-4, Sakaecho, Sakura City, Chiba 285-0014, Japan
Tel +81-43-486-1311
Fax +81-43-486-1314
Email [email protected]
Purpose: The risk preferences of patients with diabetes have profound effects on the progression of complications. The present study aimed to clarify whether the preferences of patients with diabetes and retinopathy are deliberately risk-seeking or irrational and whether this propensity is specific to those with retinopathy or is also found in patients without retinopathy compared with those without diabetes.
Patients and Methods: A total of 394 patients with diabetes (264 without retinopathy and 130 with retinopathy) and 198 patients without diabetes agreed to participate in this survey. The questions were modified versions of those from the Japan Household Survey on Consumer Preferences and Satisfaction, which sought to determine the participants’ personal socioeconomic status and risk preferences. In the questionnaires, responses were analyzed by determining the participants’ willingness to pay for a lottery ticket and for an insurance policy. Irrational responses were defined as violations of two axioms of the Expected Utility Theory: completeness and transitivity.
Results: The incidence of irrational responses increased with age and was associated with educational level. The incidence of irrational responses was significantly higher in patients with retinopathy than in those without retinopathy after adjusting for age and educational level. There was no significant difference in the incidence of irrational responses between patients with diabetes but without retinopathy and those without diabetes.
Conclusion: The risk-seeking behavior of patients with diabetes and retinopathy was not deliberate but was irrational under uncertainty. Medical professionals should be aware of their patients’ propensity to make irrational decisions, which is an important risk factor for the progression of retinopathy in patients with diabetes regardless of age and educational level.
Keywords: behavioral economics, expected utility theory, educational level, cognitive function
Plain Language Summary
Recently, we demonstrated that the risk-seeking behavior of patients with diabetes is an important factor for the progression of diabetic complications. However, there are doubts as to whether patients’ risk-seeking decisions are deliberate. In the present study, we examined the rationality of the patients’ responses to risk preference questionnaires based on the Expected Utility Theory. Irrational responses were defined as violations of two axioms of the Expected Utility Theory: completeness and transitivity. We found that the risk-seeking behavior of patients with diabetes and retinopathy was not deliberate but was irrational under uncertainty. As the practical interpretation, irrationality judged by violations of two axioms (completeness and transitivity) may suggest that the patients' preference is not well-defined and it is hard to forecast their behavior even in the similar situations. Health professionals should be aware of their patients’ propensity to make irrational decisions, which is an important risk factor for the progression of retinopathy in patients with diabetes regardless of age and educational level.
Introduction
Diabetes is a chronic disease whose prevalence is continuously increasing worldwide.1 The standard treatments for diabetes are dietary therapy and appropriate exercise, followed by the sequential addition of antihyperglycemic agents.2,3 Despite the availability of scientifically established medical treatments, a significant number of patients with diabetes do not attain glycemic control and subsequently experience diabetic complications primarily due to the failure in self-manage4 as well as due to the medication nonadherence.5
The failure in self-management and the medication nonadherence seem to be irrational behaviors to conventional theories of economics in case patients know about benefits of the treatment for the future health. The theory of behavioral economics has emerged as a new concept to clarify irrational human behavior.6 We recently reported the first application of this theory to patients in a clinical setting,7 in which we indicated that patients’ risk preferences play important roles in the progression of diabetic complications. For example, patients who seek risk in judging hypothetical lotteries were prone to develop complications. The findings are consistent with those reported by Simon-Tuval et al indicating using hypothetical lotteries that risk-seeking preferences are significantly associated with failure in self-management and the medication nonadherence.8,9 However, because we used an open pricing method in the questionnaires, there were varied responses. Some patients indicated that they would pay more for a lottery ticket than they could win, which seemed irrational. Therefore, it was questionable whether patients with risk-seeking preferences deliberately made their choices. Rationality of responses to risk preference is an important factor for patients’ education. Baker et al suggested that patient education will change health and lifestyle behavior only when traditional rationality in economics is in operation.10 To analyze the risk-seeking behavior of patients with diabetes and retinopathy, we conducted a behavioral economics survey using new questionnaires whose design was modified to detect irrational choices. Our intention was to clarify two questions: (1) whether the risk preferences of patients with diabetes with retinopathy are deliberate or irrational and (2) whether the irrationality is specific to patients with diabetes and retinopathy or is also present in patients without retinopathy compared with those without diabetes. Given that educational levels can play important roles in risk preferences and the development of retinopathy,11 we also analyzed the results in association with educational level.
Patients and Methods
This study initially included a total of 4409 patients (2126 with diabetes and 2283 with nondiabetic endocrine or metabolic diseases) who were treated by six endocrinologists between 2017 and 2020 at three outpatient clinics of the Department of Endocrinology, Diabetes, and Metabolism in medical schools located in Tokyo and Chiba, Japan. The clinics provide care to patients with difficult-to-control diabetes or other endocrine or metabolic diseases who have been referred by general practitioners. The exclusion criteria were unstable endocrine disease, psychiatric disorder, mental retardation, personality disorder, dementia, malignant disease, inability to understand the Japanese language. The patients younger than 30 years old were also excluded because their educational levels including postgraduate schools may not be accomplished and therefore socioeconomic status may not be settled yet. All eligible patients were individually recruited to participate in the survey by their doctors at a routine clinic visit. Patients who declined the recruitment request were excluded. Those who agreed to participate (the survey participants) were given book coupons worth 500 yen (equivalent to $5) as token remuneration in addition to take-home surveys, explanation sheets, and consent forms. The participants were expected to examine the explanation sheets and consent forms at home and complete the survey forms and return them along with the signed informed consent form by mail. Even at this stage of the survey, the participants were free to not return the forms if they did not agree to answer the questions. A total of 473 patients with diabetes (264 without retinopathy, 130 with retinopathy, and 79 with unknown retinopathy) and 198 patients without diabetes completed the survey (Figure 1). Patients with diabetes with unknown retinopathy were excluded from the present analysis. Table 1 shows the patient characteristics; more detailed characteristics are shown in Supplemental Table S1. The questions were modified versions of those from our previous reports7,11 and from the Japan Household Survey on Consumer Preferences and Satisfaction (https://www.iser.osaka-u.ac.jp/survey_data/top_eng.html). The questionnaire sought to determine the participants’ personal socioeconomic status and risk preferences (Supplemental Table S2). The reliability and validity have been established with the general population12 including those with obesity13 and smoking.14 Retinopathy was evaluated and categorized by ophthalmologists via fundoscopy after pupillary dilatation according to the Davis classification as follows: no diabetic retinopathy, simple diabetic retinopathy, preproliferative diabetic retinopathy, and proliferative diabetic retinopathy, including panretinal photocoagulation. Statistical analyses were performed using the JMP® 13 software (SAS Institute Inc., Cary, NC, USA). Stepwise logistic regression methods as the exploratory data analysis were used to identify the survey items associated with retinopathy. Regarding all 17 questions, except question 9 (Q9) (average spending on medical care), sex, age, duration of diabetes, and body mass index were entered as independent variables in the stepwise regression model. Items were eliminated by the model in a backward stepwise manner using the minimum Akaike’s information criterion to choose the best model. Likelihood ratio tests and Pearson’s tests were used to compare the incidence of rational and irrational responses. Cochran–Mantel–Haenszel tests were used for stratified analysis by age group and educational level. p < 0.05 was considered to be significant. This study was conducted in accordance with the Declaration of Helsinki. The study protocol, including the consent form with a confidentiality clause, was approved by the Internal Review Board of the Ethics Committee of Nippon Medical School and Juntendo University Urayasu Hospital.
 |
Table 1 Patients’ Characteristics |
 |
Figure 1 Recruitment process. |
Results
Logistic Regression Analysis of Questionnaires Associated with Retinopathy
Logistic regression analyses of questionnaires associated with retinopathy were performed for the confirmation of reproducibility of our previous report in patients in the present study. The analysis included 394 patients with diabetes with and without retinopathy. Logistic regression analysis with backward stepwise parameter selection (it begins with a model containing all questionnaires and parameters used in the previous reports) is the best tool for the exploratory data analysis. Although the selection process is purely mathematical without any clinical meanings, we can avoid overlooking unexpected parameters associated with retinopathy. As shown in Table 2, risk aversion, as estimated by the maximum price, the participant was willing to pay for an insurance policy (Q13), was significantly associated with retinopathy, along with other factors such as diabetes duration, spare time, procrastination during childhood, and savings. The maximum price for the lottery ticket (Q12) was eliminated during the stepwise search for the best regression model because of its positive correlation with the maximum acceptable price for the insurance policy (Q13) (p < 0.0001). Although it appears contradictory that risk-seeking (Q12 lottery) positively correlates with risk aversion (Q13 insurance), it is necessary to determine whether their responses were deliberate or irrational. Educational level, which has been found to be a risk factor of retinopathy in patients with diabetes younger than 65 years in our previous study, was also eliminated because of its correlations with savings (Q16) (p < 0.0001). This correlation indicates a close relationship between educational level and financial status in patients with diabetes. The results are consistent with those of our previous reports7,11 and confirm the reproducibility of the studies. Given that our previous report has suggested that some of the answers from patients with diabetes seemed unreasonable with respect to the pricing of lottery tickets and insurance policies, we examined whether the responses were rational or irrational using the Expected Utility Theory.
 |
Table 2 Logistic Regression Analysis of Factors Associated with Retinopathy in Patients with Diabetes |
Examination of Rationality in the Risk Preference Choices of Patients with Diabetes Using the Expected Utility Theory
Figure 2A shows the format of Q12 (lottery) and Q13 (insurance), and Figure 2B shows examples of the rational and irrational responses given in the survey. The criteria for the rational choices according to the axioms of the Expected Utility Theory are as follows:
 |
Figure 2 (Continued). |
Axiom 1, completeness: all prices should be chosen as either “Purchase” or “Do not purchase.”
Axiom 2, transitivity: the choices for prices lower than the maximum “Purchase” price should be “Purchase.”
Rational choices must meet both axiom 1 and axiom 2. Violations of the two axioms are judged as irrational.
The incidence of irrational responses to Q13 (insurance) increased with age (30–49-year age group, 6.6%; 50–64-year age group, 10.3%; 65–70-year age group, 27.3%; ≥71-year age group, 46.0%; likelihood ratio test, chi-squared value (χ2), 95.7; p < 0.001) and was significantly associated with educational level (9–12 years of education, 33.6%; 13–15 years, 18.4%; ≥16 years, 12.9%; likelihood ratio test, χ2, 33.6; p < 0.001). There was no difference in sex with respect to the incidence of irrational responses (male 23.4%, female 23.1%). Tables 3–5 shows the incidence of irrational responses to Q13 by the patients with diabetes with and without retinopathy. Patients with retinopathy showed a significantly higher incidence of irrational responses to Q13. Among the patients with retinopathy, 38.5% of the responses were considered irrational, whereas 21.5% of the responses from patients without retinopathy and 14.1% of those from patients without diabetes were considered irrational. The incidence of irrational responses was associated with age and educational level, and these parameters differed between patients with and without diabetes. Therefore, we performed the Cochran–Mantel–Haenszel test to adjust for age and educational level. Tables 3–5 shows the results of the detailed statistical analysis, which confirmed the higher incidence of irrational responses in patients with retinopathy (p < 0.01). The relative risk of irrational responses to Q13 for patients with diabetes and retinopathy was 1.78 (95% CI 1.30–2.44) compared with that for those without retinopathy. Results from logistic regression model for irrational responses to Q13 containing age, presence or absence of retinopathy, and educational level are shown in Supplemental Table S3. The incidence of irrational responses to Q12 (lottery) were similar to those for Q13 (Tables 6–8). The relative risk of irrational responses to Q12 for patients with diabetes with retinopathy was 1.81 (95% CI 1.26–2.60) compared with that for those without retinopathy. Results from logistic regression model for irrational responses to Q12 containing age, presence or absence of retinopathy, and educational level are shown in Supplemental Table S4. There was no significant difference in the incidence of irrational responses to Q13 (insurance) between patients with diabetes without retinopathy and those without diabetes in the analysis stratified by age group (Table 9). Results from logistic regression model for irrational responses to Q12 and Q13 containing age, patients without diabetes or with diabetes without retinopathy, and educational level are shown in Supplemental Tables S5 and S6.
 |
Table 3 Overall Analysis of Incidence of Irrational Choices to Q13 (Insurance) in Patients with and without Diabetes and with and without Retinopathy by Likelihood Ratio Test and Pearson Test |
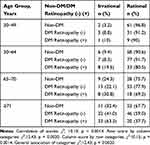 |
Table 4 Cochran–Mantel–Haenszel Tests for Data in Table 3 Stratified by Age Group |
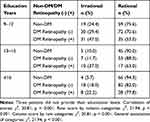 |
Table 5 Cochran–Mantel–Haenszel Tests for Data in Table 3 Stratified by Educational Level |
 |
Table 6 Overall Analysis of Incidence of Irrational Choices to Q12 (Lottery) in Patients with and without Diabetes and with and without Retinopathy by Likelihood Ratio Test and Pearson Test |
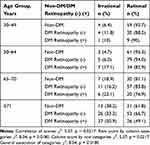 |
Table 7 Cochran–Mantel–Haenszel Tests for Data in Table 6 Stratified by Age Group |
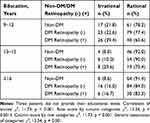 |
Table 8 Cochran–Mantel–Haenszel Tests for Data in Table 6 Stratified by Educational Level |
 |
Table 9 Incidence of Irrational Choices to Q13 (Insurance) in Patients without Diabetes and Patients with Diabetes without Retinopathy |
Discussion
The attitude of patients with diabetes toward risk is a significant factor in glycemic control and the progression of complications. Using lottery choice tasks, Simon-Tuval et al demonstrated that risk-seeking patients with type 2 diabetes adhere less to self-care behavior and medications.8,9 We previously showed that patients with diabetes who were risk-seeking in judging hypothetical lotteries were prone to developing complications.7 Although the method for estimating risk preferences using the maximum price that an individual‘s willing to pay for a lottery ticket has been proved in economics,13–15 the participants of these studies were usually healthy volunteers. Our previous report indicated that we could not differentiate between patients with diabetes who were deliberately risk-seeking and those who made irrational choices.
There are various definitions of economic rationality.10,16 We defined irrationality as the violation of the two basic axioms of the Expected Utility Theory: completeness and transitivity. The axiom of completeness implies that respondents know their preference and the axiom of transitivity assumes that their preferences are monotonic and continuous. Ryan et al suggested that by using quantitative tests, there may be “rational” reasons for why patients’ responses were irrational when they were simply judged based on axioms.17 Campbell et al indicated that poor behavioral choices can be economically rational, especially under highly stressful conditions.16 These reports suggest that irrational responses may be due to study design and open-ended questions may reveal the rationality of “irrational” responses by patients. However, analysis of open-ended questions is difficult to draw any statistically meaningful conclusions. Therefore, it seems appropriate to judge irrationality by the violations of the axioms. The criteria are clear and robust in a large number of variations of the response by patterns.
The incidences of irrational responses to Q12 and Q13 were significantly higher for patients with diabetes and retinopathy than for those without retinopathy. This result suggests that it is not appropriate to judge patients’ preferences as risk-seeking or risk aversion by estimating the maximum prices they are willing to pay for lottery tickets and insurance policies because the maximum price indicates only a fragment of their attitude toward risk. The results also suggest that irrational response could be a specific risk factor for patients with diabetes to progress to diabetic retinopathy. However, it is not clear whether patients’ irrational choices are the cause or the effect of poor glycemic control and subsequent diabetic complications. There is a similar controversy regarding cognitive function and type 2 diabetes mellitus;18,19 cognitive function appears to be an important factor for patients’ irrational responses, as discussed below.
There are two factors relevant to irrational responses. The first is that the incidence of irrational responses increased with age. In the ≥71-year age group, 49% of patients with diabetes and 32% of patients without diabetes gave irrational responses to Q13, whereas only 10% and 3%, respectively, of the 30–49-year age group gave irrational responses. The age-dependent increase in irrational responses, which was prominent in patients with retinopathy, may be due to deterioration in cognitive function. This result was consistent with the already established fact that mild cognitive impairment is common in patients with diabetes.20–23 Educational level was another relevant factor for irrational responses. The lower the educational level, the higher the incidence of irrational responses. The results suggest that cognitive function plays an important role in irrational responses. However, it should be noted that cognitive function appears not to be the only determinant factor because analysis stratified by age group and educational level still showed a significantly higher incidence of irrational responses in patients with diabetes and retinopathy; there were irrational responses in the most educated patients without diabetes in the younger age group. There may still be an undetermined factor that induces patients’ irrational choices. One of the possible factors could be brain function specific to risk preferences. Irrational decision-making under uncertainty is influenced by the brain dopamine system in rats.24 Insulin resistance in brain alters dopamine turnover and results in behavioral disorders.25 The brain dopamine system might be a pre-existing factor, and brain insulin resistance might affect the system and result in deterioration in glycemic control in some patients with diabetes. To clarify the mechanism of association between irrational preferences and retinopathy, a broad range of experiments will be necessary, including well-designed experiments for risk preferences combined with the estimation of multidomain cognitive function and quantitative measurements of brain insulin resistance in humans.
Sampling bias may be a limitation of this study, particularly in patients without diabetes. We decided that healthy volunteers are not suitable as nondiabetic controls because the psychology of patients with any disease is different from that of normal healthy individuals. However, further studies would be necessary for patients with various diseases other than endocrine and metabolic diseases. Some patients were not enrolled due to the exclusion criteria, and others declined the survey recruitment request. Even after agreeing to participate, one-fifth of the participants did not return the survey sheet probably because they were unwilling to answer the questions concerning their privacy. Although certain types of sampling bias might be inevitable in any survey that depends on patient volunteerism, our data are validated as follows. Age and sex differences were adjusted via stratified analysis. The socioeconomic status indicated by educational level was not significantly different among the three categories. Patients with an educational level above high school in the present study comprised 57.6% of the study population, which is compatible with the proportion of 54.0% in Japan (Japanese Government Statistics 2017). Taken together, it might be reasonable to state that the patients in the present study were representative of the patients in Japan. However, further studies are warranted in other countries and ethnic groups to confirm these results.
Conclusion
We demonstrated that the risk-seeking preferences of patients with diabetes and retinopathy are not deliberate but irrational and that irrational responses to risk preference questionnaires are a risk factor for the progression of retinopathy in patients with diabetes regardless of age and educational level. As the practical interpretation, irrationality judged by violations of two axioms (completeness and transitivity) may suggest that the patients’ preference is not well-defined and it is hard to forecast their behavior even in the similar situations. Different educational and psychological approaches may be necessary for patients with diabetes based on whether their risk-seeking preferences are deliberate or irrational.
Data Sharing Statement
The data that support the findings of this study are stored in the Department of Endocrinology, Diabetes and Metabolism, Graduate School of Medicine, Nippon Medical School, and are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Internal Review Board of the Ethics Committee of Nippon Medical School (#29-07-803) and Juntendo University Urayasu Hospital. The study participants provided written informed consent for the study contents, purposes, protocols, data confidentiality and anonymity procedures, and publication. The freedom to discontinue the study at any stage was explained and agreed upon.
Acknowledgments
The authors would like to thank Enago (www.enago.jp) for the English language review.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, took part in drafting the article or revising it critically for important intellectual content, agreed to submit to the current journal, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Funding
This study was supported by Grants-in-Aid for scientific research from the Japan Society for the Promotion of Science (KAKENHI) for Research Project #17K08936 (FY 2017-2019).
Disclosure
The authors report no conflicts of interest.
References
1. Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;389(10085):2239–2251.
2. American Diabetes Association. 5. Facilitating behavior change and well-being to improve health outcomes: standards of medical care in diabetes-2020. Diab Care. 2020;43(Suppl 1):S48–S65. doi:10.2337/dc20-S005
3. American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2020. Diab Care. 2020;43(Suppl 1):S98–S110. doi:10.2337/dc20-S009
4. Karl FM, Holle R, Schwettmann L, Peters A, Laxy M. Time preference, outcome expectancy, and self-management in patients with type 2 diabetes. Patient Prefer Adherence. 2018;12:1937–1945. doi:10.2147/PPA.S175045
5. Polonsky WH, Henry RR. Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors. Patient Prefer Adherence. 2016;10:1299–1307.
6. Kahneman D. Thinking, Fast and Slow. Farrar, Straus and Giroux: New York; 2011.
7. Emoto N, Okajima F, Sugihara H, Goto R. Behavioral economics survey of patients with type 1 and type 2 diabetes. Patient Prefer Adherence. 2015;9:649–658. doi:10.2147/PPA.S82022
8. Simon-Tuval T, Shmueli A, Harman-Boehm I. Adherence to self-care behaviors among patients with type 2 diabetes-the role of risk preferences. Value Health. 2016;19(6):844–851. doi:10.1016/j.jval.2016.04.003
9. Simon-Tuval T, Shmueli A, Harman-Boehm I. Adherence of patients with type 2 diabetes mellitus to medications: the role of risk preferences. Curr Med Res Opin. 2018;34(2):345–351. doi:10.1080/03007995.2017.1397506
10. Baker RM. Economic rationality and health and lifestyle choices for people with diabetes. Social Sci Med. 2006;63(9):2341–2353. doi:10.1016/j.socscimed.2006.06.007
11. Emoto N, Okajima F, Sugihara H, Goto R. A socioeconomic and behavioral survey of patients with difficult-to-control type 2 diabetes mellitus reveals an association between diabetic retinopathy and educational attainment. Patient Prefer Adherence. 2016;10:2151–2162. doi:10.2147/PPA.S116198
12. Watanapongvanich S, Binnagan P, Putthinun P, Khan MSR, Kadoya Y. Financial literacy and gambling behavior: evidence from Japan. J Gambling Studies. 2020. doi:10.1007/s10899-020-09936-3
13. Ikeda S, Kang MI, Ohtake F. Hyperbolic discounting, the sign effect, and the body mass index. J Health Econ. 2010;29(2):268–284. doi:10.1016/j.jhealeco.2010.01.002
14. Kang MI, Ikeda S. Time discounting and smoking behavior: evidence from a panel survey. Health Econ. 2014;23(12):1443–1464. doi:10.1002/hec.2998
15. Donkers B, Melenberg B, Van Soest A. Estimating risk attitudes using lotteries: a large sample approach. J Risk Uncertain. 2001;22(2):165–195. doi:10.1023/A:1011109625844
16. Campbell D. Economic rationality in choosing between short-term bad-health choices and longer-term good-health choices. Int J Environ Res Public Health. 2013;10(11):5971–5988. doi:10.3390/ijerph10115971
17. Ryan M, Watson V, Entwistle V. Rationalising the ‘irrational’: a think aloud study of discrete choice experiment responses. Health Econ. 2009;18(3):321–336. doi:10.1002/hec.1369
18. Ganmore I, Beeri MS. The chicken or the egg? Does glycaemic control predict cognitive function or the other way around? Diabetologia. 2018;61(9):1913–1917. doi:10.1007/s00125-018-4689-9
19. Altschul DM, Starr JM, Deary IJ. Cognitive function in early and later life is associated with blood glucose in older individuals: analysis of the lothian birth cohort of 1936. Diabetologia. 2018;61(9):1946–1955. doi:10.1007/s00125-018-4645-8
20. Cavanaugh K, Huizinga MM, Wallston KA, et al. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737–746. doi:10.7326/0003-4819-148-10-200805200-00006
21. Biessels GJ, Despa F. Cognitive decline and dementia in diabetes mellitus: mechanisms and clinical implications. Nat Rev Endocrinol. 2018;14(10):591–604. doi:10.1038/s41574-018-0048-7
22. Luchsinger JA, Reitz C, Patel B, Tang MX, Manly JJ, Mayeux R. Relation of diabetes to mild cognitive impairment. Arch Neurol. 2007;64(4):570–575. doi:10.1001/archneur.64.4.570
23. Roy S, Kim N, Desai A, et al. Cognitive function and control of type 2 diabetes mellitus in young adults. N Am J Med Sci. 2015;7(5):220–226. doi:10.4103/1947-2714.157627
24. Cocker PJ, Dinelle K, Kornelson R, Sossi V, Winstanley CA. Irrational choice under uncertainty correlates with lower striatal D (2/3) receptor binding in rats. J Neurosci. 2012;32(44):15450–15457. doi:10.1523/JNEUROSCI.0626-12.2012
25. Kleinridders A, Cai W, Cappellucci L, et al. Insulin resistance in brain alters dopamine turnover and causes behavioral disorders. Proc Natl Acad Sci U S A. 2015;112(11):3463–3468. doi:10.1073/pnas.1500877112
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

