Back to Journals » International Journal of General Medicine » Volume 15
Intrapleural Instillation of Sodium Bicarbonate versus Urokinase in Management of Complicated Pleural Effusion: A Comparative Cohort Study
Authors Zayed NE , El Fakharany K, Mehriz Naguib Abozaid M
Received 5 September 2022
Accepted for publication 5 December 2022
Published 21 December 2022 Volume 2022:15 Pages 8705—8713
DOI https://doi.org/10.2147/IJGM.S388488
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Niveen E Zayed,1 Karim El Fakharany,2 Mohammed Mehriz Naguib Abozaid1
1Department of Chest Disease, Faculty of Medicine, Zagazig University, Zagazig City, Egypt; 2Department of Cardiothoracic Surgery, Faculty of Medicine, Zagazig University, Zagazig City, Egypt
Correspondence: Niveen E Zayed, Chest Department, Zagazig University, Faculty of Medicine, Sharkia Government, Zagazig City, 44519, Egypt, Tel +201024831444, Email [email protected]; [email protected]
Aim: The main target is evacuation; however, with evidence about the value of intrapleural instillation of different fibrinolytic agents still under evaluation, our aim was comparing the effectiveness and safety of intrapleural instillation of sodium bicarbonate (NaHCO3) in comparison with urokinase in patients with infected pleural effusion.
Methods: Our prospective cohort study included 40 patients with complicated empyema; the diagnosis was based on analysis of aspirated fluid in association with radiological and bacteriological culture. The patients were subjected to instillation of two different fibrinolytic agents; the first one was NaHCO3, the second was urokinase.
Results: The commonest underlying chest infection that was visualized by CT was pneumonia 70%. Nearly half of cases had community-acquired infection (45%), and more than half of them (55%) had anaerobic infection, and only five cases had TB pleural effusion based on ADA-positive, tuberculin skin test in addition to Abram’s needles closed biopsy. The rate of repeated therapeutic thoracentesis success in each group was 85%; 80% in NaHCO3 group, and 90% in urokinase group, both of them was significantly equal, P=0.37. Moreover, the frequency of complications in all patients was less than 13%, hence hemothorax and iatrogenic pneumothorax was 12.5%, and only 10% of cases were admitted in ICU after the maneuver, with insignificant difference in between the groups. However, looking at the smaller rate of RTT failure of NaHCO3 or urokinase, the logistic regression model showed that RTT–NaHCO3 was insignificantly related to failure in both unadjusted and adjusted models, P=0.37 and 0.32, respectively, and only smoking habits increase the likelihood of failure 9-fold (OR=8.9, P=0.04) with respect to age, sex, and treatment methods.
Conclusion: The efficacy of repeated therapeutic thoracentesis (RTT) with intrapleural instillation of NaHCO3 was effective and safe, the same as urokinase, with consideration that NaHCO3 was much more available and affordable than urokinase.
Keywords: pleural infection, fibrinolytic agents, NaHCO3, urokinase
Introduction
Infected pleural effusion is a collection of pus in the pleural space, and is considered as a severe form of infection with mortality rate about 20%.1 Commonly it happens as a consequence of pulmonary infection such as pneumonia and lung abscess, then a simple para-pneumonic fluid collection is formed,2,3 and by the effect of both bacteria and white cell metabolism, the fluid is rapidly turned to purulent empyema, which is characterized by low pH and higher LDH enzyme level.4 The pathophysiological degree of empyema is classified into three stages; the first is simple exudative fluid collection, the second is fibrinopurulent transformation, and the third is aggressive organization phase.5,6 The important point of pathophysiological classification of empyema is to guide the process of treatment intervention, hence, the gold standard treatment strategy of infected pleural effusion is evacuation beside the good coverage of antibiotics; however, with formation of fibrinopurulent stage, the theory of using intrapleural fibrinolytic agents is introduced as an add-on therapy to minimize the need for surgical consequences if the classical treatment fails.7–9 Several clinical trials and observational studies were conducted and introduced a different fibrinolytic therapy such as streptokinase, tPA, and DNase as a treatment option for complicated effusion.10,11 Streptokinase and other fibrinolytic substances had the ability to destruct the fibrin threads, which subsequently leads to opening of the loculi, and eventually enhancing the fluid evacuation and healing.12–14 However, this area of research is still growing, putting into consideration the safety and efficacy issues.
Sodium bicarbonate solution has potential antithrombotic and antimicrobial properties;20,21 it has the ability to chelate calcium ions and thus inhibits the conversion of fibrinogen to fibrin.20 Moreover, the antimicrobial ability of sodium bicarbonate may decrease the formation of bacterial biofilm, especially Gram-positive organisms as staphylococci in addition to decreasing its adherence.22 Furthermore, the ionic abundance of NaHCO3 may alter the membrane permeability of the bacteria, which further leads to modification of their structure to become less viable.23 The present work was designed as an observational prospective cohort study to assess the safety and efficacy of sodium bicarbonate (NaHCO3) as a promising fibrinolytic agent in comparison with urokinase in the treatment of complicated pleural effusion.
Patients and Methods
Patients and Study Design
A prospective cohort study that included 40 patients with infected pleural effusion was carried out through the period from June 2020 to January 2022 at the chest department of Zagazig University Hospital. The study included all patients above 18 years of age, with at least one of the following criteria that denote infected fluid. The first was frank pus aspiration, the second was fluid pH <7.2, the third was positive microbiological culture of the aspirated fluid, and the fourth was intrapleural loculation in the radiological examination. After written consent from all participants for publication of their data, the study has been approved from the ethical committee office of the faculty of medicine, Zagazig University in agreement with the Helsinki Declaration rules.
Data Collection
The data of the selected patients were collected in a spreadsheet and included all demographic characteristics and clinical, laboratory, radiological, and bacteriological findings, in addition to the outcome of cases, which stand for the success rate and the associated complications such as hemothorax, iatrogenic pneumothorax, and need for ICU admission for any reasons during intrapleural instillation procedures.
Fibrinolytic Instillation Protocol
The dose of urokinase was 100,000 UI, then diluted in 50 mL saline solution, while the NaHCO3 ampule contains 50 meq in 50 mL. The fibrinolytic agents were instilled in the pleural space by the effect of gravity using pleural trocar at the end of thoracentesis. The thoracentesis was repeated to get rid of the accumulated fluid till the effusion was significantly decreased. The good outcome was defined as adequate pleural evacuation, improvement of clinical state, and control of systemic infection, in addition to enhancement of radiological picture.
Statistical Analysis
The data were collected and coded in an Excel spreadsheet, and the normality of data was examined using Shapiro–Wilk test using Minitab 17.1.0.0 for Windows (Minitab Inc., 2013, Pennsylvania, USA). Continuous data were represented as mean and standard deviation, and categorical data as number and percentage. The comparison between two means was done using an independent t-test, while the frequency comparison was made using the chi-square test. Logistic regression analysis was performed on the factors associated with RTT failure either with unadjusted or adjusted models. All tests were two-sided, and a P value below 0.05 was considered significant.
Results
General Characteristics of Patients
The study included forty patients with infected pleural effusion that were subjected to repeated therapeutic thoracentesis with instillation of two different materials; the first group (Group-A; n=20) was treated with NaHCO3, while the second group (Group-B; n=20) was treated with urokinase. The mean (SD) age of the patients was 52 (15) years, and more than half of them were male (55%). DM was the most frequent comorbidity followed by HTN and IHD (65%, 32.5%, and 12.5%, respectively). Additionally, nearly half of cases were currently smokers and had underlying chest disease (42.5% and 40%, respectively). However, the studied groups were matched as regarding all basic factors, although the Group-A had significantly higher percentage of cases with underlying chest disease (P=0.05, Table 1).
 |
Table 1 General Characters of Patient’s Groups |
Radiological Findings and Biochemical Analysis
About 95% of cases had infected effusion with moderate to large amount that exceeded 1/2 of the thorax, and 55% of them showed loculation in US assessment, Figure 1.
 |
Figure 1 Thoracic ultrasound: (A) complex pleural effusion with loculation; (B) homogeneous effusion with septation after evacuation trial. |
Additionally, the commonest underlying chest infection that was visualized by CT was pneumonia (70%); consolidation and air bronchogram, Figure 2.
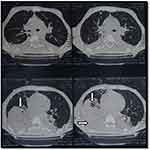 |
Figure 2 Chest computed tomography (CT). The arrows point to consolidation areas with air bronchogram and effusion. |
Furthermore, 8 cases showed cavity with different wall thickness. Irrespectively, both treatment groups were matched regarding all radiological factors, Table 2. All cases showed an exudative pattern regarding Light’s criteria, and nearly half of cases had community-acquired infection (45%), while more than half of cases (55%) showed anaerobic infection. Five cases had TB pleural effusion based on ADA-positive, tuberculin skin test in addition to Abram’s needles closed biopsy.
 |
Table 2 Radiological and Biochemical Analysis of Infected Pleural Effusion |
Consequence of Repeated Thoracentesis Treatment (RTT) and Factors Associated with Failure
As shown in Table 3, the rate of RTT success was 85%; 80% in the NaHCO3 group, and 90% in the urokinase group, both of them significantly equal, P=0.37. However, all cases had developed fever after injection of NaHCO3 and urokinase, and there were insignificant differences between them regarding the duration of fever, P=0.75. Moreover, the frequency of complication in all patients was less than 13%, thus hemothorax and iatrogenic pneumothorax occurred in 12.5%, and only 10% of cases were admitted in ICU after the maneuver, with insignificant difference between the groups. The parametric data are presented as mean and standard deviation (SD), and categorical data as number and percentage (%), Table 3.
 |
Table 3 Treatment Complications and Outcomes |
However, looking at the smaller rate of RTT failure of either NaHCO3 or urokinase, the logistic regression model Table 4 showed that RTT–NaHCO3 was insignificantly related to failure both in unadjusted and adjusted models, P=0.37 and 0.32, respectively, and only smoking habits increase the likelihood of failure 9-fold; OR=8.9, P=0.04 with respect to age, sex, and treatment methods.
 |
Table 4 Factors Associated with RTT Failure |
Discussion
The risk of mortality among patients with pleural infection is higher, and it needs a strict and time-related treatment protocol to avoid the undesired surgery and complications.7 The standard protocol for managing empyema is still undiscovered. The present study aimed to introduce sodium bicarbonate as an add-on therapy in the treatment of complicated pleural infection, and we compared the performance of sodium bicarbonate with the previously used fibrinolytic agent “urokinase” regarding efficacy and safety. Urokinase as fibrinolytic agent had been used and evaluated in several observational studies as well as interventional trials with acceptable results regarding its efficacy and safety.15–18 It was also associated with lower incidence of bleeding and allergic response in comparison with streptokinase.8,19 However, sodium bicarbonate solution has some potential properties regarding antithrombotic ability in addition to antimicrobial benefits.20,21 The calcium ions are chelated by NaHCO3, which subsequently inhibits the conversion of fibrinogen to fibrin.20 As well, the antimicrobial ability of sodium bicarbonate may decrease the formation of bacterial biofilm, especially Gram-positive organisms as staphylococci, in addition to decreasing its adherence.22 Furthermore, the ionic abundance of NaHCO3 may alter the membrane permeability of the bacteria, which further leads to modification of their structure to become less viable.23 The present data showed that the rate of successful thoracentesis in the NaHCO3 group was 80% in comparison with 90% success rate in the urokinase group, with an insignificant difference, P=0.37. Additionally, considering undesired complications, bleeding during procedures had been recorded in only one case in the NaHCO3 group, in contrast to 3 cases in the urokinase group. Moreover, iatrogenic pneumothorax was also recorded in 5 cases; 2 in the NaHCO3 group and 3 in the urokinase group. The need for ICU admission was also recorded, with one case admitted in ICU in the NaHCO3 group in contrast to 3 cases in the urokinase group. However, the differences between the two groups were insignificant, which means the capability of sodium bicarbonate in managing complicated pleural effusion was equal to the urokinase. The results regarding the efficacy of urokinase were supported by several studies,15–19 but no previous study had used NaHCO3 instillation with repeated thoracentesis as the present study. In spite of that, an Egyptian study suggested that the use of sodium bicarbonate lavage during medical thoracoscopy (MT) in treatment of complicated para-pneumonic effusion was beneficial, and the improvement rate reached 88%.24 However, one of the strength points of our study was the use of sodium bicarbonate without invasive thoracoscopy, and even with frequent irrigation and thoracentesis, the overall outcome was acceptable. Another consideration that should be kept in mind, which made the sodium bicarbonate a potential alternative fibrinolytic agent, was its availability and affordability; additionally, its presence in different concentrations may open the window for future researchers to reach the optimal outcome. The current study had some limitation: the first was being a single-center study, which made some difference with other reports; the second was its small sample size, which made the generalization of the results much more restricted; however, more research using observational studies with larger cohorts was mandatory, in addition to designing a randomized control trial with a large scale of patients.
Conclusion
Sodium bicarbonate was a promising, affordable, and efficient fibrinolytic agent; it showed equal effectiveness and safety as urokinase in managing complicated pleural effusion.
Abbreviations
RTT, repeated therapeutic thoracentesis; SD, standard deviation; LDH, lactate dehydrogenase; tPA, tissue plasminogen activator.
Data Sharing Statement
The data sets utilized in this study are available upon reasonable request to the corresponding author.
Acknowledgment
The authors would like to thank all who supported the work at the Faculty of Medicine, Zagazig University.
Disclosure
The authors declare no competing interests in this work.
References
1. Karpathiou G, Péoc’h M, Sundaralingam A, Rahman N, Froudarakis ME. Inflammation of the pleural cavity: a review on pathogenesis, diagnosis and implications in tumor pathophysiology. Cancers. 2022;14(6):1415. doi:10.3390/cancers14061415
2. Krutikov M, Rahman A, Tiberi S. Necrotizing pneumonia (aetiology, clinical features and management). Curr Opin Pulm Med. 2019;25(3):225–232. doi:10.1097/MCP.0000000000000571
3. Heffner JE, Klein J. Parapneumonic effusions and empyema. In Seminars in respiratory and critical care medicine 2001 (Vol. 22, No. 06, pp. 591–606). Copyright© 2001 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA. Semin Respir Crit Care Med. 2001;22(6):591–606. doi:10.1055/s-2001-18795
4. Rahman NM, Chapman SJ, Davies RJ. The approach to the patient with a parapneumonic effusion. Semin Respir Crit Care Med. 2010;31(6):706–715. doi:10.1055/s-0030-1269830
5. Hassan M, Patel S, Sadaka AS, Bedawi EO, Corcoran JP, Porcel JM. Recent insights into the management of pleural infection. Int J Gen Med. 2021;14:3415–3429. PMCID: PMC8286963, PMID: 34290522. doi:10.2147/IJGM.S292705
6. Higuchi M, Suzuki H. Current status and prospect of medical and surgical management for thoracic empyema. Curr Chall Thorac Surg. 2020;2:39. doi:10.21037/ccts.2020.02.09
7. Kanai E, Matsutani N. Management of empyema: a comprehensive review. Curr Chall Thorac Surg. 2020;2:38. doi:10.21037/ccts.2020.03.02
8. Altmann ES, Crossingham I, Wilson S, Davies HR. Intra‐pleural fibrinolytic therapy versus placebo, or a different fibrinolytic agent, in the treatment of adult parapneumonic effusions and empyema. Cochrane Database Syst Rev. 2019;2019(10):CD002312. doi:10.1002/14651858.CD002312.pub4
9. Maskell NA, Davies CW, Nunn AJ, et al. UK controlled trial of intrapleural streptokinase for pleural infection. N Engl J Med. 2005;352(9):865–874. doi:10.1056/NEJMoa042473
10. Bouros D, Antoniou KM, Light RW. Intrapleural streptokinase for pleural infection. BMJ. 2006;332(7534):133–134. doi:10.1136/bmj.332.7534.133
11. Rahman NM, Maskell NA, West A, et al. Intrapleural use of tissue plasminogen activator and DNase in pleural infection. N Engl J Med. 2011;365(6):518–526. doi:10.1056/NEJMoa1012740
12. Krishnamurthy A, Belur PD, Subramanya SB. Methods available to assess therapeutic potential of fibrinolytic enzymes of microbial origin: a review. J Anal Sci Technol. 2018;9(1):1. doi:10.1186/s40543-018-0143-3
13. Varjú I, Kolev K. Networks that stop the flow: a fresh look at fibrin and neutrophil extracellular traps. Thromb Res. 2019;182:1–11. doi:10.1016/j.thromres.2019.08.003
14. Pechlaner C. Plasminogen activators in inflammation and sepsis. Acta Med Austriaca. 2002;29(3):80–88. doi:10.1046/j.1563-2571.2002.02011
15. Bédat B, Plojoux J, Noel J, et al. Comparison of intrapleural use of urokinase and tissue plasminogen activator/DNAse in pleural infection. ERJ Open Res. 2019;5(3). doi:10.1183/23120541.00084-2019
16. Paz LD, Bayeh B, Chauvin P, et al. Intrapleural use of urokinase and DNase in pleural infections managed with repeated thoracentesis: a comparative cohort study. PLoS One. 2021;16(9):e0257339. doi:10.1371/journal.pone.0257339
17. Beckert L, Brockway B, Simpson G, et al. Phase I trial of the single-chain urokinase intrapleural LTI-01 in complicated parapneumonic effusions or empyema. JCI Insight. 2019;5(10):e127470. doi:10.1172/jci.insight.127470
18. Lee S, Lee H, Lee DH, et al. Fibrinolysis with lower dose urokinase in patients with complicated parapneumonic effusion. Tuberc Respir Dis. 2021;84(2):134. doi:10.4046/trd.2020.0018
19. Alemán C, Porcel JM, Alegre J, et al. Intrapleural fibrinolysis with urokinase versus alteplase in complicated parapneumonic pleural effusions and empyema: a prospective randomized study. Lung. 2015;193(6):993–1000. doi:10.1007/s00408-015-9807-6
20. Wong DW, Mishkin FS, Tanaka TT. The effects of bicarbonate on blood coagulation. JAMA. 1980;244(1):61–62. doi:10.1001/jama.1980.03310010047028
21. Wong DW. Effect of sodium bicarbonate on in vitro conversion of fibrinogen to fibrin. J Pharm Sci. 1980;69(8):978–980. doi:10.1002/jps.2600690832
22. Nostro A, Cellini L, Di Giulio M, et al. Effect of alkaline pH on staphylococcal biofilm formation. APMIS. 2012;120(9):733–742. doi:10.1111/j.1600-0463.2012.02900.x
23. Farha MA, French S, Stokes JM, Brown ED. Bicarbonate alters bacterial susceptibility to antibiotics by targeting the proton motive force. ACS infectious diseases. 2017 Dec 21; 4(3): 382–90. ACS Infect Dis. 2018;4(3):382–390. doi:10.1021/acsinfecdis.7b00194
24. Goldberg K, Sarig H, Zaknoon F, Epand RF, Epand RM, Mor A. Sensitization of gram-negative bacteria by targeting the membrane potential. FASEB J. 2013;27(9):3818–3826. PMID: 2373374. doi:10.1096/fj.13-227942
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
