Back to Journals » Clinical Ophthalmology » Volume 9
Intrapersonal comparison of initial axial length, keratometric readings, and intraocular lens power over a 6-month interval using an IOLMaster device
Authors Khambhiphant B, Varadisai A , Visalvate N
Received 28 September 2014
Accepted for publication 7 November 2014
Published 22 December 2014 Volume 2015:9 Pages 21—24
DOI https://doi.org/10.2147/OPTH.S75075
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Bharkbhum Khambhiphant,1 Adisai Varadisai,2 Nat Visalvate2
1Department of Ophthalmology, King Chulalongkorn Memorial Hospital, Thai Red Cross Society, 2Department of Ophthalmology, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
Purpose: In order to improve current biometry practice, we investigated changes in axial length (AL), keratometry (K), and intraocular lens (IOL) power measured by the IOLMaster in adults within a 6-month period at the outpatient eye clinic, King Chulalongkorn Memorial Hospital, Bangkok, Thailand.
Patients and methods: This was a nonrandomized prospective cohort study. The AL, steepest K, flattest K, and IOL power of nondilated eyes were measured at the initial examination and later at 6 months by the IOLMaster. Changes in AL, K, and IOL power using the SRK (Sanders, Retzlaff, and Kraff)-T formula within 6 months were compared using the paired-sample t-test.
Results: The study comprised 90 eyes from 90 patients. The mean age of the patients was 62.99±13.95 years (range 28–87 years). Mean values and standard deviation for AL, steepest K, flattest K, and IOL power at initial visit and 6 months later were 23.56±1.51 mm and 23.56±1.52 mm (P=1.0; 95% confidence interval [CI] -0.01 to 0), 44.94±1.37 D and 44.98±1.43 D (P=0.96; 95% CI -0.13 to 0.04), 43.85±1.43 D and 43.89±1.36 D (P=0.93; 95% CI -0.02 to 0.07), and 20.27±4.12 D and 20.15±4.51 D (P=0.99; 95% CI -0.05 to 0.29), respectively.
Conclusion: There was no statistically significant difference in AL (P=1.0), both K (P=0.96, P=0.93), or IOL power (P=0.99) within the 6-month period using the IOLMaster. Remeasurement at 6 months may be required in some cases, but should not be routine.
Keywords: cataract, axial length, keratometry, IOLMaster, IOL power
Introduction
Cataract is the most common cause of global blindness, and mostly occurs from aging change.1–3 Most of the cataract population in Thailand range in age from 61 to 80 years.4 The treatment of cataract is surgery to remove the old cloudy natural lens and replacing it with intraocular lens (IOL) implantation. Current optical biometry used in calculating the IOL power for cataract surgery can be divided into a sound-wave principle called A-scan, consisting of an applanation technique and immersion technique, and a light-wave principle: noncontact partial coherence interferometry (IOLMaster device).
The Zeiss IOLMaster is based on noncontact partial coherence interferometry, with an infrared wave (590–880 nm) measuring the corneal convex to the retinal pigment epithelium layer. The measurement results are operator-independent and take less time. Some important features of the IOLMaster are the fact that it is a noncontact measurement device with higher speed and higher accuracy, together with a resolution going up to 0.01 mm.5 The Zeiss IOLMaster is more accurate than ultrasound biometry in IOL-power calculation, resulting in excellent refractive outcomes.6–10
The operational administration of outpatients of the Ophthalmology Department in King Chulalongkorn Memorial Hospital is such that for cataract and cataract surgery with IOL-implantation patients, they are sent for scheduling of the surgery together with IOL-power measurement in preparation for surgery. Due to the large numbers of patients having the surgery in King Chulalongkorn Memorial Hospital, some patients have to wait longer than 6 months for surgery. Normally, patients whose IOL power was measured longer than 6 months previously will be sent for a repeat measurement in order to confirm the IOL power to be used in the surgery.
With the SRK (Sanders, Retzlaff, and Kraff) formula P = AL − (2.5 L) − 0.9 K, where P = lens-implant power for emmetropia (D), AL = axial length (mm), K = average keratometric reading (D), and A = constant specific to the lens implant to be used, we found that the variable factors of IOL power change were AL and K. In the normal population, after 10–15 years there will be no significant increase of AL and no significant change of K within 1 year.11 Based on this, the investigators believe that it is an unnecessary waste of time and expense to send patients for a repeat IOL-power measurement. In this experiment, IOL power was calculated using the SRK/T formula.
Patients and methods
This was a prospective cohort study to compare IOL power, AL, and K at 0 and 6 months with an IOLMaster device (version 5; Carl Zeiss, Jena, Germany). This study was conducted under an institutional review board-approved protocol, Faculty of Medicine, Chulalongkorn University. We received financial support from the Ratchadapiseksompotch Fund. This study was done at the outpatient clinic of the Department of Ophthalmology, King Chulalongkorn Memorial Hospital from August 2011 to October 2012. All participating subjects read and signed the informed consent form before enrollment. The participants in this study were aged over 18 years, with no current medical condition (topical or systemic) that affected accommodation. In cataract patients, they needed not to have dense cataracts that prohibited the use of the IOLMaster device. Subjects with a history of extraocular and intraocular surgery were excluded. One who could not fix their eyes at one specific point was excluded. The subjects’ AL and K (both steepest and flattest) were measured with the IOLMaster device. The SRK/T formula was used for IOL-power calculation in this study. All subjects were assigned to have IOLMaster measurements once in the same eye at the first visit and then 6 months later without pupil dilation.
Patient age, sex, measured eye, IOL power, AL, and K (both steepest K and flattest K) were included in data collection. The main outcomes were IOL power using the SRK/T formula (aiming at the nearest to emmetropia), AL, and K (steepest K and flattest K) at 0 months and 6 months. The two groups of data were recorded on a standardized data-collection sheet that was used for data entry into a structured database program for analysis (SPSS for Mac version 20).
Statistical analysis
Patient demographic data were recorded as the means ± standard deviation. For the main outcomes (IOL power, AL, and K), univariate analysis using two-tailed paired-sample t-tests assuming equal variance were used to compare means between the two groups. Statistical significance was set at 0.05 using SPSS software for Mac version 20.
Results
Subject
Ninety patients with cataract were included in the study. The mean age of the study population was 62.99±13.95 years (range 28–87). The demographic data of the patients is shown in Table 1.
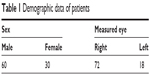  | Table 1 Demographic data of patients |
Outcomes
The main outcomes, IOL power, AL, and K (steepest K and flattest K) at 0 and 6 months, are presented in Table 2.
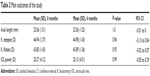  | Table 2 Main outcomes of the study |
Discussion
As already mentioned, in the normal population, after 10–15 years there will be no significant increase of AL and no significant change of K within 1 year.11 Most patients who receive cataract surgery and IOL implantation in King Chulalongkorn Memorial Hospital are elderly, in whom AL and K values should not change. In this circumstance, the investigators recognized that though 6 months’ time had passed, IOL power should not have changed.
From the study outcome, there was no statistical significant difference between AL and K (steepest K and flattest K) at 0 and 6 months. We used IOLMaster, as it is more precise, reliable, and repeatable in long and short eyes, especially with cataract.12,13 Lopez de la Fuente et al14 found that the IOLMaster had very good repeatability in healthy young persons.
For IOL power, which was the main variable of interest, the investigators needed to study its differentiation. By specifying the acceptable difference of measurement for both time periods at not over ±0.5 D, we found that there was no statistical significant difference, corresponding with the hypothesis of the investigators.
A limitation of this study was that the investigators chose to use only the SRK-T formula in calculating IOL power, without grouping assortments of the patients’ AL in order to get the most accurate IOL power.15 For the duration of the comparison, the main outcome proved that the length of duration may have been insufficient to find a statistically significant difference.
Due to the fact that there has been no study done on IOL-power measurement to see the difference in the duration of each measurement that may affect the IOL power, this will be assessed in future work.
In conclusion, there were no statistically significant differences in AL, K (steepest K and flattest K), or IOL power within the 6-month period using the IOLMaster. In order for improvements in the operational administration of outpatients of the Ophthalmology Department in King Chulalongkorn Memorial Hospital and the reduction of unnecessary expense, it is not necessary to send patients for remeasurement. Remeasurement at 6 months may be required in some cases, but should not be routine.
Acknowledgment
Financial support was received from the Ratchadapiseksompotch Research Fund, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.
Disclosure
The authors report no conflicts of interest in this work.
References
Resnikoff S, Pascolini D, Etya’ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82(11):844–851. | ||
Pistolla G, Tsilimparis MK, Prastacos P, Sifaki-Pistolla D, Philalithis A, Pallikaris IG. Ophthalmological disorders in rural areas of Crete: a geospatial analysis. Rural Remote Health. 2013;13(1):2020. | ||
Chiang PP, Zheng Y, Wong TY, Lamoureux EL. Vision impairment and major causes of vision loss impacts on vision-specific functioning independent of socioeconomic factors. Ophthalmology. 2013;120(2):415–422. | ||
Yospaiboon Y, Yospaiboon K, Ratanapakorn T, Sinawat S, Sanguansak T, Bhoomibunchoo C. Management of cataract in the Thai population. J Med Assoc Thai. 2012;95 Suppl 7:S177–S181. | ||
Hussin HM, Spry PG, Majid MA, Gouws P. Reliability and validity of the partial coherence interferometry for measurement of ocular axial length in children. Eye (Lond). 2006;20(9):1021–1024. | ||
Verhulst E, Vrijghem JC. Accuracy of intraocular lens power calculations using the Zeiss IOL master. A prospective study. Bull Soc Belge Ophtalmol. 2001;(281):61–65. | ||
Chiselită D, Cantemir A, Gălătanu C, Irod A. [Comparision [sic] of two new optical biometry devices with an ultrasonic immersion biometer]. Oftalmologia. 2011;55(4):104–110. Romanian. | ||
Hsieh YT, Wang IJ. Intraocular lens power measured by partial coherence interferometry. Optom Vis Sci. 2012;89(12):1697–1701. | ||
Rajan MS, Keilhorn I, Bell JA. Partial coherence laser interferometry vs conventional ultrasound biometry in intraocular lens power calculations. Eye (Lond). 2002;16(5):552–556. | ||
Tehrani M, Krummenauer F, Kumar R, Dick HB. Comparison of biometric measurements using partial coherence interferometry and applanation ultrasound. J Cataract Refract Surg. 2003;29(4):747–752. | ||
Gordon RA, Donzis PB. Refractive development of the human eye. Arch Ophthalmol. 1985;103(6):785–789. | ||
Eleftheriadis H. IOLMaster biometry: refractive results of 100 consecutive cases. Br J Ophthalmol. 2003;87(8):960–963. | ||
Németh J, Fekete O, Pesztenlehrer N. Optical and ultrasound measurement of axial length and anterior chamber depth for intraocular lens power calculation. J Cataract Refract Surg. 2003;29(1):85–88. | ||
Lopez de la Fuente C, Sanchez-Cano A, Segura F, Pinilla I. Comparison of anterior segment measurements obtained by three different devices in healthy eyes. Biomed Res Int. 2014;2014:498080. | ||
Roessler GF, Dietlein TS, Plange N, et al. Accuracy of intraocular lens power calculation using partial coherence interferometry in patients with high myopia. Ophthalmic Physiol Opt. 2012;32(3):228–233. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
