Back to Journals » Advances in Medical Education and Practice » Volume 10
Internet use and eHealth literacy among health-care professionals in a resource limited setting: a cross-sectional survey
Authors Shiferaw KB , Mehari EA
Received 14 February 2019
Accepted for publication 15 June 2019
Published 25 July 2019 Volume 2019:10 Pages 563—570
DOI https://doi.org/10.2147/AMEP.S205414
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Kirubel Biruk Shiferaw,1 Eden Abetu Mehari2
1Department of Health Informatics, College of Medicine and Health Science, Debre Markos University, Debre Markos, Ethiopia; 2Department of Clinical Pharmacy, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
Background: Health-care professionals should be able to identify and use reputable health care–information sources from the Internet and other relevant sources of information, in order to make good medical decisions. The level in health professional eHealth literacy and the extent of Internet use in a resource-constrained setting is not well documented. The aim of this study was to assess the extent of Internet use and eHealth literacy among a cross section of health-care professionals at the University of Gondar Comprehensive Specialized Hospital, northwest Ethiopia.
Methods: An institution-based cross-sectional study was conducted to assess Internet use and eHealth literacy among health professionals working at the hospital from November 20 to January 17, 2018. Descriptive analysis was used to describe Internet use and eHealth literacy. Multivariable logistic regression was done to identify which factors were associated with the eHealth literacy of participants.
Results: In total, 291 study subjects were approached and included in the study, with a response rate of 98.6%. The majority of respondents were female (53.7%) and the mean age was 30.09±5.025 years. Only 47.4% of survey respondents said that they used the Internet regularly for professional/medical updates. The mean eHealth literacy was 27.840±5.691. The majority of participants with high eHealth literacy were aged 21–29 years. and females were slightly more literate regarding eHealth than males (33.1%). Age, type of profession, salary, and years of experience were significantly associated with eHealth literacy.
Conclusion: The present data confirm that Internet use and eHealth literacy of health professionals is noticeably good, which clearly suggests that there is an opportunity for eHealth to be integrated in the health-care system in tertiary-health facilities in northern Ethiopia if appropriate training and education is provided.
Keywords: Internet use, eHealth literacy, health professionals, Ethiopia
A Letter to the Editor has been published for this article.
Introduction
The Internet is one of the main sources of information that enables users to have access to a larger volume of information in many sectors, regardless of geographic location. Surveys have indicated that most Internet users in the world have used the Internet to get health information.1–3 Developments in Internet access and improvements in performance due to new technologies have made the Internet the focus of many new health-care improvements.3–7 As a result, the Internet is having a significant impact on health and health care, as it has the potential to advance the health-care delivery and support the decision-making of health-care providers.8 When compared with other professionals of different disciplines, health-care professionals use the Internet more.9 The impact of the Internet on the health-care profession looks to increase as health-care professionals use it more as an instrument to them stay informed and up to date on recent improvements in their respective specialties.9–11
According to Internet World Stats, the number of Internet users in Ethiopia has increased from 10,000 users to more than 16 million in the past two decades, with 15% Internet penetration.12 Although there have been no studies done in the areas of Internet cost and availability in Ethiopia, it is relatively costly when compared to other developed nations. The concept of eHealth literacy is defined as “the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to address or solve a health problem.”13 eHealth literacy includes six basic skills: traditional literacy, health literacy, information literacy, scientific literacy, media literacy, and computer literacy. As a result, eHealth literacy is affected by such factors as age, sex, education, availability and accessibility of the Internet, and income.13–16
Studies have shown that distorted information may influence health beliefs and behavior of individuals negatively.17,18 Health-care professionals should be able to identify and use reliable health care–information sources from the Internet, in order to make sound decisions and interventions.19 The existing literature has mainly focused on developed countries. There have been few studies done in developing countries, particularly in sub-Saharan Africa. Studies have been conducted regarding computer literacy and utilization among Ethiopian health professionals and medical students, which were reported to be low.20–23 However, health-care professionals’ perspectives on Internet use and their eHealth literacy are lacking. The aim of this study was to assess the extent of Internet use and evaluate eHealth literacy among a cross section of health-care professionals at the University of Gondar Comprehensive Specialized Hospital (UOGSH), northwest Ethiopia.
Methods
Study design and setting
An institution-based cross-sectional study was conducted to assess Internet use and eHealth literacy among health professionals working at the UOGSH from November 20 to January 17, 2018. During the study period, the UOGCSH had 834 permanent health-professional employees. The majority were nurses (483), medical laboratory technicians (110), and midwives (95). All health professionals who were on annual and sick leave were excluded. There were desktop computers in some departments, and very few of them had Internet connections. Most of the departments did not use the computers for information-seeking or quick referencing; rather, they used them for recording purposes only.
Sampling and participants
The sample for this study was calculated by using a single population–proportion formula, with finite population correction,24 95% confidence level, and a proportion of Internet use of 50%, since there had been no previous study done in the same population, with relative precision of 5% and 10% nonresponse rates. The sample-size formula was valid for this study, because the calculated sample was >5% of the total study population. As such, we needed to use the formula with finite-population correction:
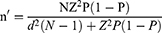
where n' is sample size with finite-population correction, N population size, Z the Z-statistic for level of confidence, P expected proportion, and d precision.
Accordingly, the total sample was 291. A simple random-sampling technique was performed to select study participants.
Data acquisition and analysis
A self-administered structured questionnaire was adapted after reviewing the relevant literature.9,25,26 It had been validated and pretested on 30 health professionals working at Debre Markos Referral Hospital for its consistency.27 The questionnaire has three main parts. The first part contains items on sociodemographic information of participants. The second part is related to participants’ use of the Internet, and the third part contains items to evaluate eHealth literacy of the participants. We asked participants 15 categorical (yes/no) items to determine their use of and access to the Internet. The eHealth literacy scale (eHEALS) was used as a measuring tool, as it has high internal consistency (α=0.88).25 The eHEALS measures the ability to locate, evaluate, integrate, and apply information gained from the Internet. Respondents evaluate their level of agreement with alternatives (strongly agree, agree, undecided and disagree) on the eight items. One can score a minimum of 8 and a maximum of 40 in this section. After collection, data were checked, cleaned, and analyzed using Epi Info and SPSS version 20. Descriptive analysis was performed to describe Internet use and eHealth literacy. Binary logistic regression was done to identify which factors were associated with eHealth literacy.
Operational definitions
In this study, “Internet use” referred to health professionals’ practice of using the Internet for browsing health-related information to make sound decisions, whereas “eHealth literacy” referred to participants' ability to locate and use credible information from the Internet. An eHealth-literacy score of 26 was used as a cutoff point to determine the level of eHealth literacy of participants. After a relevant-literature review, we labeled eHEALS score ≥26 as high eHealth literacy and eHEALS score <26 as low eHealth literacy.28–31Ethical clearance was secured from the Department of Health Informatics, College of Medicine and Health Sciences, Debre Markos University ethical review committee. Additional permission was obtained from the offices of UOGCSH hospital directors, and verbal informed consent from respondents was also attained. Verbal informed consent was acceptable and approved by the ethical review committee.
Results
In total, 291 study subjects were approached and included in the study from November 20 to January 17, 2018. The response rate was 98.6%. The majority of respondents (154, 53.7%) were females, and the mean age was 30.09±5.025 years. A large number of respondents were bachelor's degree holders (220, 76.7%). Most study participants were nurses 88 (30.7%), and regarding work experience, employees with <5 years of work experience (167, 58.2%) comprised the majority. A total of 191 (66.6%) respondents were employees earning a monthly salary of ETB 3,500–5,500 (Table 1).
 |
Table 1 Participants’ sociodemographic characteristics |
Internet use
Overall, 100% of health professionals reported that they had access to the Internet, of which 41.5% used smart phones and 54% of them a wi-fi connection to access the Internet. In sum, 41.8% of respondents had Internet access in their office, and 42.2% reported that they used the Internet several days a week. Only 47.4% of survey respondents said that they used the Internet regularly for professional/medical updates, while 66.2% stated that they would take certified web-based courses. See Table 2 for details.
 |
Table 2 Internet access and use |
eHealth literacy
Of the 287 participants, 199 (69.3%) reported that they had high eHealth literacy. Mean eHealth literacy was 27.840±5.691. The majority of participants with high eHealth literacy were aged 21–29 years, and females (104, 36.2%) were slightly more literate regarding eHealth than males (95, 33.1%). A total of 128 (44.6%) health professionals with less <5 years' work experience reported that they possessed high eHealth literacy. Among various health professionals, Nursesnand degree holders reported higher level of eHealth literacy. For more detail, see Table 3.
 |
Table 3 eHealth literacy–response frequency and percentage |
From the eHEALS, the statement “I know what health resources are available on the Internet” had the highest level of agreement (254 of 287, 88.5%). The two statements that health professionals had the highest level of disagreement with were related to confidence in using information received from the Internet to make health decisions (129 of 287 [45.5%] disagreed and strongly disagreed) and ability to find helpful resources on the Internet (103 of 287 [35.9%] disagreed and strongly disagreed). On binary logistic regression, age 20–29 years, physicians, and those with <5 years' work experience demonstrated a higher likelihood of self-reported eHealth literacy. See Table 4 for details.
 |
Table 4 Multivariable logistic regression for eHealth literacy |
Discussion
The findings from this study revealed that although health professionals have access to use the Internet, most do not use it for searching reputable health information from online databases like PubMed and websites. Their self-reported eHealth literacy was also found to be reasonably good. Internet access in this study was 100%, but in other relevant studies conducted in developed countries, there was relatively less access. This disparity could be because of study setting: this study was conducted at a single institution.9,32 In sum, 47.4% of participants in this study confirmed that they used the Internet for regular medical/professional updates, which is very low compared to health-care professionals in developed countries like the UK, where it is 97%.33 A possible reason for this could be the poor computer hardware and very slow Internet connection at the hospital. More than half the participants in this study were willing to take certified web-based courses, similar to online surveys among health professionals in other countries.34,35 The effect of Internet use on clinical decisions was also notably significant and confirmed studies conducted in the US and Taiwan.36,37 On the contrary, the quality of health-care information was less trusted, similar to findings of Benigeri and Pluye.38 Only 2.4% of health professionals recommended a website for their patients. On the other hand, patients never asked health professionals for a website recommendation to get more information on their condition, and this could have been due to the socioeconomic and infrastructural limitations of the underdeveloped world.35,39 Our findings in this study illustrate that physicians use the Internet for medical updates more and other professionals like pharmacists and medical laboratory technicians use the Internet for finding health-related information less, which is similar to studies in Nigeria and Malaysia.40,41
Regarding eHealth literacy, this study found that most health professionals (69.3%) reported high eHealth literacy, which confirms other findings.42 This study revealed that doctors and nurses had higher eHealth literacy than pharmacists and other health professionals, which confirms a Scottish study.43 Monthly salary and years of experience were predictive of low eHealth literacy. This could be due to lower-paid health professionals not usually being degree holders, which implies that they do not have college education. Aside from the concept of digitizing health care being a new concept for underdeveloped countries like Ethiopia, health professionals with more work experience are unwilling to use new technologies. Although it was not on the regression table, Internet use significantly predicted the eHealth literacy of health professionals, which coincides with other research.42Finally, although the majority of health professionals have access to the Internet, most of them do not use it for finding health information from credible sources. Findings from the eHEALS indicate high potential for future developments in eHealth interventions. The hospital might consider conduct training on how to find credible health information from reputable online sources.
Limitation
The major limitation of this study was the small sample, which was due to limited resources, and it was conducted among health professionals working at the UOGSH. For this reason, the results may not be attributable to the entire health-professional population. It would be more useful and generalizable if this study were conducted in the Amhara region as a whole with appropriate stratum samples to determine the extent of Internet use and eHealth literacy of a larger sample of health professionals in more facilities than we were able to cover.
Conclusion
Besides the mounting indication of efficacy, the present data confirm that Internet use and eHealth literacy of health professionals are noticeably good. This clearly suggests that there is an opportunity for eHealth to be fully integrated into the health-care system at tertiary-health facilities if appropriate training and education is provided.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Acknowledgments
The authors of this study would like to thank all health professionals for their time and effort spent during the data-collection period.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bujnowska-Fedak MM. Trends in the use of the internet for health purposes in Poland. BMC Public Health. 2015;15:194. doi:10.1186/s12889-015-1473-3
2. James DCS, Harville Cedric II. eHealth literacy, online help-seeking behavior, and willingness to participate in mhealth chronic disease research among African Americans, Florida, 2014-2015. Prev Chronic Dis. 2016;13:E156. doi:10.5888/pcd13.160231
3. Burrus MT, Werner BC, Starman JS, et al. Patient perceptions and current trends in internet use by orthopedic outpatients. Hss J. 2017;13(3):271–275. doi:10.1007/s11420-017-9568-2
4. Aardoom JJ, Dingemans AE, Spinhoven P, Roijen LH-V, Van Furth EF. An Internet-based intervention for eating disorders consisting of automated computer-tailored feedback with or without supplemented frequent or infrequent support from a coach: study protocol for a randomized controlled trial. Trials. 2013;14:340. doi:10.1186/1745-6215-14-340
5. Gray M. Making the future of healthcare. Z Evid Fortbild Qual Gesundhwes. 2008;102(4):231–233.
6. Laugesen J, Hassanein K. The impact of internet health information on patient compliance: a research model and an empirical study. J Med Internet Res. 2015;17(6):e143. doi:10.2196/jmir.4333
7. Biruk K, Abetu E. Modeling predictors of acceptance and use of electronic medical record system in a resource limited setting: using modified UTAUT model. Inf Med Unlocked. 2019;100182. Epub 13 April, 2019.
8. Kantor D, Bright JR, Burtchell J. Perspectives from the patient and the healthcare professional in multiple sclerosis: social media and participatory medicine. Neurol Ther. 2018;7(1):37–49. doi:10.1007/s40120-017-0088-2
9. Podichetty VK, Booher J, Whitfield M, Biscup RS. Assessment of internet use and effects among healthcare professionals: a cross sectional survey. Postgrad Med J. 2006;82(966):274–279. doi:10.1136/pgmj.2005.040675
10. Lialiou P, Mantas J. Evaluation of health professionals in the use of internet information retrieval systems in health: a literature review. Stud Health Technol Inform. 2013;190:80–82.
11. McInnes DK, Gifford AL, Kazis LE, Wagner TH. Disparities in health-related internet use by US veterans: results from a national survey. Inform Prim Care. 2010;18(1):59–68.
12. Usage and population statistics, https://internetworldstats.com/stats1.htm. Available from: https://internetworldstats.com/stats1.htm. Accessed December 5, 2018.
13. Norman C, Skinner H. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J Med Internet Res 2006;8(2):e9.
14. Xesfingi S, Vozikis A. eHealth literacy: in the quest of the contributing factors. Interact J Med Res. 2016;5(2):e16. doi:10.2196/ijmr.5767
15. Lewis T. Seeking health information on the internet: lifestyle choice or bad attack of cyberchondria? Media, Culture & Society. 2006;28(4):521–539. doi:10.1177/0163443706065027
16. Osei Asibey B, Agyemang S, Boakye Dankwah A. The Internet Use For Health Information Seeking among Ghanaian university students: a cross-sectional study. Int J Telemed Appl. 2017;2017:9. doi:10.1155/2017/1756473
17. Lewandowsky S, Ecker UK, Seifert CM, Schwarz N, Cook J. Misinformation and its correction: continued influence and successful debiasing. Psychol Sci Public Interest. 2012;13(3):106–131. doi:10.1177/1529100612451018
18. Dutta-Bergman M. trusted online sources of health information: differences in demographics, health beliefs, and health-information orientation. J Med Internet Res. 2003;5(3):e21. doi:10.2196/jmir.5.3.e21
19. Metzger MJ, Flanagin AJ. Using Web 2.0 technologies to enhance evidence-based medical information. J Health Commun. 2011;16 Suppl 1(Suppl 1):45–58. doi:10.1080/10810730.2011.589881
20. Alwan K, Awoke T, Tilahun B. Knowledge and utilization of computers among health professionals in a developing country: a cross-sectional study. JMIR Hum Factors. 2015;2(1):e4. doi:10.2196/humanfactors.4184
21. Mohammed E, Andargie G, Meseret S, Girma E. Knowledge and utilization of computer among health workers in Addis Ababa hospitals, Ethiopia: computer literacy in the health sector. BMC Res Notes. 2013;6:106. doi:10.1186/1756-0500-6-106
22. Woreta SA, Kebede Y, Zegeye DT. Knowledge and utilization of information communication technology (ICT) among health science students at the university of Gondar, North Western Ethiopia. BMC Med Inform Decis Mak. 2013;13:31. doi:10.1186/1472-6947-13-31
23. Biruk K, Abetu E. Knowledge and attitude of health professionals toward telemedicine in resource-limited settings: a cross-sectional study in North West Ethiopia. J Healthc Eng. 2018;2018:7. doi:10.1155/2018/2389268
24. Naing L, Winn T, Rusli BN. Practical issues in calculating the sample size for prevalence studies. Arch Orofacial Sci. 2006;1:9–14.
25. Norman CD, Skinner HA. eHEALS: the ehealth literacy scale. J Med Internet Res. 2006;8(4):e27. doi:10.2196/jmir.8.4.e27
26. Dashti S, Peyman N, Tajfard M, Esmaeeli H. E-Health literacy of medical and health sciences university students in Mashhad, Iran in 2016: a pilot study. Electron Physician. 2017;9(3):3966–3973. doi:10.19082/3966
27. Perneger TV, Courvoisier D, Hudelson P, Gayet-Ageron A. Sample Size for Pre-Tests of Questionnaires. Qual Life Res. 2014;24(1):147–151.
28. Milne RA, Puts MT, Papadakos J, et al. Predictors of high eHealth literacy in primary lung cancer survivors. J Cancer Educ. 2015;30(4):685–692. doi:10.1007/s13187-014-0744-5
29. Mitsutake S, Shibata A, Ishii K, Okazaki K, Oka K. [Developing Japanese version of the eHealth literacy scale (eHEALS)]. Nihon Koshu Eisei Zasshi. 2011;58(5):361–371.
30. van der Vaart R, van Deursen AJ, Drossaert CH, Taal E, van Dijk JA, van de Laar MA. Does the eHealth Literacy Scale (eHEALS) measure what it intends to measure? validation of a dutch version of the eHEALS in two adult populations. J Med Internet Res. 2011;13(4):e86. doi:10.2196/jmir.1658
31. Richtering SS, Hyun K, Neubeck L, et al. eHealth literacy: predictors in a population with moderate-to-high cardiovascular risk. JMIR Hum Factors. 2017;4(1):e4. doi:10.2196/humanfactors.6217
32. Tod AM, Harrison J, Morris Docker S, Black R, Wolstenholme D. Access to the internet in an acute care area: experiences of nurses. Br J Nurs. 2003;12(7):
33. Nicolaou M, Armstrong R, Hassell AB, Walker D, Birrell F. Musculoskeletal health professional use of internet resources for personal and patient education: results from an online national survey. Open Rheumatol J. 2012;6:190–198. doi:10.2174/1874312901206010190
34. Huckstadt A, Hayes K. Evaluation of interactive online courses for advanced practice nurses. J Am Acad Nurse Pract. 2005;17(3):85–89. doi:10.111/j.1041-2972.2005.0015.x
35. Kaufman N, Internet and information technology use in treatment of diabetes. Int J Clin Pract Suppl. 2010;166:41–46. doi:10.1111/j.1742-1241.2009.02277.x
36. Lee C-J, Hornik RC. Physician trust moderates the internet use and physician visit relationship. J Health Commun. 2009;14(1):70–76. doi:10.1080/10810730802592262
37. Chen -Y-Y, Li C-M, Liang J-C, Tsai -C-C. Health information obtained from the internet and changes in medical decision making: questionnaire development and cross-sectional survey. J Med Internet Res. 2018;20(2):e47. doi:10.2196/jmir.9370
38. Benigeri M, Pluye P. Shortcomings of health information on the internet. Health Promot Int. 2003;18(4):381–386. doi:10.1093/heapro/dag409
39. Emond Y, de Groot J, Wetzels W, van Osch L. Internet guidance in oncology practice: determinants of health professionals’ Internet referral behavior. Psycho-oncology. 2013;22(1):74–82. doi:10.1002/pon.2056
40. Ajuwon GA. Use of the internet for health information by physicians for patient care in a teaching hospital in Ibadan, Nigeria. Biomed Digit Libr. 2006;3:12. doi:10.1186/1742-5581-3-12
41. Ong SW, Hassali MA, Saleem F. Community pharmacists’ perceptions towards online health information in Kuala Lumpur, Malaysia. Pharm Pract (Granada). 2018;16(2):1166. doi:10.18549/PharmPract.2018.02.1166
42. Hennemann S, Beutel ME, Zwerenz R. Ready for eHealth? Health professionals’ acceptance and adoption of ehealth interventions in inpatient routine care. J Health Commun. 2017;22(3):274–284. doi:10.1080/10810730.2017.1284286
43. MacLure K, Stewart D. A qualitative case study of ehealth and digital literacy experiences of pharmacy staff. Res Social Adm Pharm. 2018;14(6):555–563. doi:10.1016/j.sapharm.2017.07.001
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
