Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 12
Interactive and potentially independent roles of renin-angiotensin-aldosterone system blockade and the development of cardiorenal syndrome, type 1 on in-hospital mortality among elderly patients admitted with acute decompensated congestive heart failure
Authors Iglesias J, Ghetiya S , Ledesma KJ , Patel CS, Levine JS
Received 1 September 2018
Accepted for publication 12 February 2019
Published 14 March 2019 Volume 2019:12 Pages 33—48
DOI https://doi.org/10.2147/IJNRD.S185988
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Jose Iglesias,1–4 Savan Ghetiya,5 Kandria J Ledesma,6 Chirag S Patel,7 Jerrold S Levine8,9
1Department of Medicine, Subsection of Nephrology, Rowan University School of Osteopathic Medicine, Stratford, NJ, USA; 2Department of Medicine, Subsection of Nephrology, Jersey Shore University Medical Center, Neptune, NJ, USA; 3Department of Medicine Section of Nephrology, Robert Wood Johnson School of Medicine, New Brunswick, NJ, USA; 4Department of Medicine, Subsection of Nephrology, RWJ Barnabas Health Community Medical Center, Toms River, NJ, USA; 5Department of Medicine, Coney Island University Medical Center, New York, NY, USA; 6American University of Antigua College of Medicine, Coolidge, Antigua and Barbuda; 7Department of Medicine, Jersey Shore University Medical Center, Neptune, NJ, USA; 8Department of Medicine, Section of Nephrology, University of Illinois at Chicago, Chicago, IL, USA; 9Department of Medicine Section of Nephrology, Jesse Brown Veterans Affairs Medical Center, Chicago, IL, USA
Purpose: Cardiorenal syndrome type 1 (CRS1), defined as worsening renal function from acute decompensated congestive heart failure (ADCHF), is complicated by the fact that CRS1 limits the use of common therapeutic strategies, such as angiotensin converting-enzyme inhibitors (ACEIs) or angiotensin II-receptor blockers (A2RB). The present study examines retrospectively the role of ACEI/A2RB usage on in-hospital mortality among elderly ADCHF patients, in particular those who developed CRS1.
Methods: We retrospectively examined the effects of ACEI/A2RB usage and CRS1 development (in-hospital change in serum creatinine ≥0.3 mg/dL or ≥0.5 mg/dL), as well as their potential interaction, on in-hospital mortality among elderly ADCHF patients (aged ≥65 years). Employing univariate and multivariate analyses, we performed risk-factor analysis on a cohort of 419 patients (51 nonsurvivors [12.2%]) for whom we had complete clinical and laboratory data (median follow-up 5 days) from 2,361 consecutive elderly ADCHF patients (106 nonsurvivors [4.6%]).
Results: By multivariate analysis, the two strongest independent predictors of in-hospital mortality were CRS1 development (OR 7.8, 95% CI 3.9–15.5; P=0.00001) and lack of ACEI/A2RB usage (OR 0.49, CI 0.25–0.93; P=0.043). The effect of CRS1 was graded, with increasing CRS1 severity associated with increased mortality. On multivariate subgroup analysis, the association between lack of ACEI/A2RB usage and increased mortality remained a significant independent predictor among patients not developing CRS1 (OR 0.24, CI 0.083–0.721; P=0.011).
Conclusion: Our data suggest that development of CRS1 and lack of ACEI/A2RB usage are statistically independent predictors of in-hospital mortality for elderly ADCHF patients, with CRS1 being the stronger of the two risk factors. While it remains unclear whether lack of ACEI/A2RB usage is causally related to increased mortality or reflects another risk factor inducing physicians to forego ACEIs/A2RBs, our findings nevertheless indicate the need to address this issue in future prospective studies.
Keywords: cardiorenal syndrome type 1, angiotensin converting-enzyme inhibitors, angiotensin II-receptor blockers, acute decompensated congestive heart failure, acute renal failure
Introduction
Worsening renal function (WRF) is a common complication among patients hospitalized with acute decompensated congestive heart failure (ADCHF).1 Cardiorenal syndrome type 1 (CRS1) is defined as WRF occurring as a result of ADCHF.1 Large registries have revealed that a sizable proportion of patients hospitalized with ADCHF are elderly (≥65 years of age), and moreover that the elderly are particularly prone to CRS1.2,3 Indeed, CRS1 occurs in 25%–33% of all patients and 50% of elderly patients admitted with ADCHF.2,3 CRS1 is associated with increased resource utilization, morbidity, and mortality.4,5 In addition, complications associated with CRS1, such as anemia and volume overload, may worsen the clinical course of ADCHF.1,6 Management of ADCHF is complicated by the fact that CRS1 or concerns regarding its development often limit the use of common therapeutic strategies, such as inhibition of the renin–angiotensin–aldosterone system (RAAS) and/or escalation of diuretic therapy.5,7–9 Although WRF may be transient in ADCHF patients, RAAS inhibition and/or escalation of diuretic therapy may in themselves lead to WRF, further complicating the clinical picture.10–14
An important question for patients hospitalized with ADCHF is at what level of WRF RAAS inhibitions lose its survival advantage.8,15 For example, in patients with chronic CHF, the benefits of RAAS inhibition are maintained for rises of serum creatinine (SCr) up to 30%–50%.16,17 Unfortunately, similar data in the case of ADCHF remain scarce. Despite the clear benefits of RAAS inhibition for patients with chronic CHF, the survival benefits of RAAS inhibition in patients with ADCHF have not yet been definitively established. For example, in a study by Kittleson et al, circulatory and/or renal limitations of angiotensin converting-enzyme inhibitor (ACEI) usage, including WRF, hyperkalemia, and symptomatic hypotension, were documented in 23% of patients admitted for ADCHF, and accounted for their failure to be on ACEIs at discharge.13 Patients not receiving ACEIs on discharge were more than twice as likely to die during the following year. The authors concluded that circulatory and/or renal limitations of ACEI usage, of which WRF comprised ~50%, were a marker of patients at increased risk of death. However, recently the association between WRF and poor outcomes in all ADCHF patients undergoing therapy has been challenged.9,10 For these reasons, the management of elderly ADCHF patients with CRS1 can be particularly challenging in terms of balancing the risks of WRF against the benefits of maximized therapy to improve ADCHF.
The purpose of the present study was to examine retrospectively the effect of RAAS inhibition on short-term in-hospital mortality for elderly ADCHF patients in general, and in particular for the subset of ADCHF patients who develop CRS1. Our study population consisted of 2,361 consecutive elderly patients admitted to a 500-bed nonteaching community hospital with a diagnosis of ADCHF. Risk-factor analysis was limited to a cohort of 419 patients for whom we had complete clinical and laboratory data.
Methods
Patients
To identify risk factors associated with in-hospital mortality (1–35 days) among elderly patients (aged ≥65 years) with a diagnosis of ADCHF, we reviewed the clinical course of 2,361 consecutive patients admitted for ADCHF. Specifically, we examined the impact on mortality of the development of CRS1 (defined as WRF occurring during ADCHF) and/or the use of RAAS inhibition as a therapeutic modality. We limited our risk-factor analysis to a cohort of 419 patients for whom we had sufficient clinical and laboratory data. All patients were admitted between February 2, 2003 and September 11, 2007 to Robert Wood Johnson/Barnabas Health Community Medical Center in Toms River, New Jersey. Patients were identified in one of two ways: Trendstar decision-support software and database (McKesson, San Francisco, CA, USA) and Joint Commission of the Accreditation of Health Care Organization–Center for Medicare Services (CMS) Peer Review Organization of New Jersey seventh scope of work involving CHF.18 Patients with ADCHF were those given the diagnosis-related group (DRG) code 127 and ICD9-CM codes 428, 398.91, 402.01, 402.11, 402.91, 404.00, 404.10–13, and 404.90–93. For patients not in the cohort of 419, in whom specific laboratory data were lacking, the development of WRF was identified by ICD9-CM coding for acute kidney injury: 404.12, 404.13, 584.9, 584.5, 584.6, 584.9, and 586.19 All DRG and ICD9-CM codes were entered by professional coders who were approved by the respective agencies. All study patients had at least one sign or symptom consistent with the diagnosis of ADCHF, including dyspnea at rest, dyspnea with minimal exertion, peripheral edema, pulmonary rales, or radiological evidence of CHF. A diagnosis of coronary artery disease (CAD) required the presence of at least one of the following in the medical record: previous myocardial infarction, history of coronary artery bypass graft, history of percutaneous coronary angioplasty, positive coronary angiography, or positive noninvasive cardiac testing. Evaluation included serum sodium, blood urea nitrogen (BUN), hematocrit (Hct), SCr, plasma brain natriuretic peptide (BNP), peak SCr during hospitalization, medications, comorbidities, demographics, and admission physiological variables. Medications, comorbidities, and demographic variables were abstracted from the medical record. Estimated glomerular filtration rate (eGFR) was determined from the simplified equation developed by the Modification of Diet in Renal Disease study.20
Within the cohort of 419 patients with complete laboratory data, we stratified CRS1 into two categories based on the magnitude of the peak rise in SCr occurring at any time within the period of hospitalization: change in SCr (∆SCr) ≥0.3 mg/dL and ∆SCr ≥0.5 mg/dL. The choice of these two thresholds, while arbitrary, was based upon previous research showing that a threshold ∆SCr ≥0.3 mg/dL was associated with longer hospital stay and increased mortality, both in the hospital and long term.5 The study was undertaken in accordance with the principles of the Declaration of Helsinki and the standards of good clinical practice, and was approved by the Institutional Review Board and Ethics Committee (06–007) of Barnabas Health Community Medical Center.
Data analysis
The major primary outcome was in-hospital mortality. We initially examined the association between RAAS inhibition (use of ACEIs and/or angiotensin II-receptor blockers [A2RBs]) and in-hospital mortality for the entire population of 2,361 consecutive elderly ADCHF patients. We then performed risk-factor analyses for in-hospital mortality in a cohort of 419 of these patients for whom we had sufficient clinical and laboratory data. Specifically, the impact groups for which we performed risk-factor analysis were the entire cohort (n=419), subcohorts in which RAAS inhibitors were either administered (ACEI/A2RB group, n=251) or not administered (no-ACEI/A2RB group, n=168), subcohorts of survivors (n=368) and nonsurvivors (n=51), and subcohorts of patients who developed or did not develop CRS1, according to either of the two definitions (∆SCr ≥0.3 mg/dL or ≥0.5 mg/dL). Stratification of patients into the no-ACEI/A2RB and ACEI/A2RB subcohorts was based solely on in-hospital usage. Patients in the no-ACEI/A2RB subcohort did not receive ACEIs/A2RBs at any time during their hospitalization, whereas patients in the ACEI/A2RB subcohort received ACEIs/A2RBs at least once during their hospitalization, regardless of duration of administration, whether initiated in-hospital or continued from outpatient prescription. Therefore, for example, a patient in whom ACEIs/A2RBs were stopped prior to hospitalization was placed into the no-ACEI/A2RB subcohort.
Summary statistics were computed for the entire cohort of 419 patients, ACEI/A2RB vs no-ACEI/A2RB subcohorts, for the survivor vs nonsurvivor subcohorts, and for the CRS1 vs no CRS1 subcohorts. We performed both univariate and multivariate analyses. Continuous variables are expressed as mean ± SD, and were compared with Student’s t-test or the Wilcoxon rank-sum test, as appropriate. Categorical values were compared with Pearson’s c2. Kaplan–Meier survival curves and log-rank analyses were stratified according to the development of CRS1 by the two definitions given and according to ACEI/A2RB usage in patients developing or not developing CRS1, also by the two definitions given. Variables that were significant by univariate analysis at P<0.05 were candidates for multivariate analysis. Multivariate analysis, either multiple logistic regression or Cox proportional hazards, both with forward variable selection, was performed to determine variables independently predictive of mortality. Cox proportional-hazard analysis was performed only when CRS1 was not a variable, in order not to violate the assumption of constant proportionality. Step selections were based on the maximum-likelihood ratio. For continuous variables, ORs represent the relative amount by which the probability of obtaining the outcome variable increased or decreased when the independent variable was increased by exactly 1 unit. ORs and 95% CIs were determined by exponentiation of the regression coefficient and its upper and lower CI, respectively.
Results
Association of ACEI/A2RB usage with decreased mortality and decreased development of CRS1 in elderly ADCHF patients
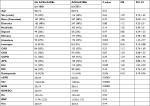
To determine the impact of ACEI/A2RB usage on in-hospital mortality and development of CRS1 in elderly patients with ADCHF, we retrospectively evaluated 2,361 consecutive patients admitted with a diagnosis of ADCHF. Of these, 1,726 (73%) received ACEI/A2RB therapy. In-hospital mortality decreased significantly in patients receiving ACEIs/A2RBs (6.8% vs 32.8%, OR 0.34, 95% CI 0.25–0.49; P=0.00001; Table 1). The development of CRS1 was significantly associated with increased in-hospital mortality (6.0% vs 3.9%, OR 1.54, 95% CI 1.03–2.3; P=0.035; Table 1). Despite the protective association of ACEI/A2RB usage with mortality, there was no significant difference in the development of CRS1 among patients receiving vs not receiving ACEI/A2RB therapy (26.6% vs 27.8%, OR 0.94, 95% CI 0.72–1.05; P=0.55; Table 1).
As multiple acausal explanations may exist for an association between ACEI/A2RB usage and decreased in-hospital mortality, we addressed this issue more closely in a cohort of 419 patients for whom we had complete clinical and laboratory data (Table 2). A total of 251 patients (61%) in this cohort received ACEI/A2RB therapy. Although mortality was increased in the study cohort compared with the entire population (12.2% vs 4.6%), ACEI/A2RB usage was again associated with a decreased risk of in-hospital mortality (8.0% vs 18.5%, OR 0.38, 95% CI 0.21–0.74; P=0.001; Table 2). One potential explanation for the greater mortality within the study cohort is that patients with more severe illness on presentation were more likely to receive a more extensive clinical and laboratory work-up. Regardless of the explanation, it is notable that despite overall increased in-hospital mortality, the protective association of ACEI/A2RB usage with increased in-hospital survival was replicated in the study cohort of 419 patients.
As for the entire study population, there was no statistically significant difference in the development of CRS1, defined as ∆SCr ≥0.3 mg/dL, for patients receiving vs not receiving ACEI/A2RB therapy (22.3% vs 18.5%, OR 1.25, 95% CI 0.78–2.07; P=0.34; Table 2). When CRS1 was defined more strictly as ∆SCr ≥0.5 mg/dL, ACEI/A2RB usage became associated with lower incidence (12.4% vs 20.3%, OR 0.56, 95% CI 0.33–0.95; P=0.029; Table 2). This raises the possibility that ACEI/A2RB usage may reduce mortality by protecting ADCHF patients from developing CRS1.
Univariate and multivariate analyses of risk factors for in-hospital mortality of ADCHF patients
To determine factors predictive of in-hospital mortality and to examine more closely the possible protective role of ACEI/A2RB usage, we analyzed multiple demographic, clinical, and laboratory variables routinely obtained on admission in our study cohort of 419 elderly patients admitted with ADCHF. Table 3 gives the results of a univariate analysis comparing survivors vs nonsurvivors. Admission demographic, clinical, and laboratory values associated with an increased risk of mortality were increased age (P=0.009), usage of inotropes (P=0.0001), development of CRS1, defined as either ∆SCr ≥0.3 mg/dL (P=0.00001) or ∆SCr ≥0.5 mg/dL (P=0.00001), usage of darbepoetin (P=0.024), reduced renal function on admission defined by decreased eGFR (P=0.009), elevated SCr levels (P=0.02), elevated BUN (P=0.001), and increased BNP (P=0.010). Increased risk of mortality was also associated with lack of ACEI/A2RB usage (P=0.001), lack of usage of β-blockers (P=0.006), and absence of CAD (P=0.005). Most of these univariate predictors of in-hospital mortality were in accord with previous studies, and may be grouped into categories of greater severity of ADCHF (usage of inotropes and increased BNP), preexisting renal dysfunction (decreased eGFR, increased SCr, increased BUN, and usage of darbepoetin), and development of CRS1. The absence of usage of β-blockers and CAD may be acting as surrogates for another factor linked to decreased mortality in ADCHF patients. Alternatively, recent data suggest that use of β-blockers in patients with ADCHF may decrease mortality.21 Finally, replicating the results of Table 1, ACEI/A2RB usage was associated with decreased mortality. It is pertinent to note that there was no significant difference in rate for history of chronic kidney disease in the development of CRS1 defined by either ∆SCr ≥0.3 mg/dL or ∆SCr ≥0.5 mg/dL (36% OR 1.14, 95% CI 0.760–1.174%, P=0.50; 43%, OR 1.36, 95% CI 0.80–2.3; P=0.25).
There was limited classification based on ICD9-CM documentation as to etiology of ADCHF, and in 237 patients (57%) cause was not specified. Of the remaining 182 patients, documentation revealed the causes of ADCHF to be systolic dysfunction 6.4% (n=27), diastolic dysfunction 5% (n=21), valvular heart disease 27% (n=113), and hypertensive heart disease 5% (n=21). There was no statistically significant difference in mortality among causes of ADCHF (P=0.52).
To identify independent predictors of mortality, we next performed multiple logistic regression analysis with forward variable selection. In descending order of coefficient of determination, independent predictors of mortality were development of CRS1 defined as ∆SCr ≥0.5 mg/dL, lack of usage of ACEIs/A2RBs, increased BUN on admission, and increased age (Table 4). To better understand the role of CRS1 and to determine whether its definition altered the association, we repeated the multiple logistic regression analysis, retaining one or the other definitions of CRS1, but not both, in the forward variable selection. As expected, when CRS1 was defined as ∆SCr ≥0.5 mg/dL, the same four variables emerged as independent predictors of mortality, and in the same order of coefficient of determination (Table 4). When CRS1 was defined less strictly as ∆SCr ≥0.3 mg/dL, increased BUN on admission dropped out, and inotrope usage and absence of CAD entered as independent risk factors for mortality (Table 4). Taken together, these data suggest that while the development of CRS1, regardless of definition, is associated with increased mortality, a greater rise in SCr (≥0.5 mg/dL) may be the stronger risk factor. Moreover, the fact that in all three analyses, lack of ACEI/A2RB usage and development of CRS1 emerged as independent risk factors suggests that the association between ACEI/A2RB usage and reduced mortality is independent of any effect of ACEIs/A2RBs on the likelihood of developing CRS1 during hospitalization.
Kaplan–Meier survival analysis of effect of CRS1 development on mortality
To confirm the association between the development of CRS1 and in-hospital mortality, we used Kaplan–Meier survival analysis to compare the outcomes of patients who did or did not develop CRS1 during their hospitalization (Figure 1). Defined by ∆SCr ≥0.3 mg/dL, CRS1 developed in 87 (20.8%) of the 419 patients, whereas for ∆SCr ≥0.5 mg/dL, CRS1 developed in 65 (15.5%) of patients. Although in general, survival was better for patients who did not develop CRS1 by either definition, a significant difference in survival was seen only when CRS1 was defined more strictly (∆SCr ≥0.5 mg/dL, P=0.037; ∆SCr ≥0.3 mg/dL, P=0.19). These results are consistent with those of multiple logistic regression analysis, and further indicate that a stricter definition of CRS1, defined by ∆SCr ≥0.5 mg/dL, may be a more specific marker of increased risk for mortality.
Comparison of risk factors for in-hospital mortality in ADCHF patients receiving vs not receiving ACEIs/A2RBs
We next addressed the nature of the association between ACEI/A2RB usage and decreased in-hospital mortality. We first compared baseline characteristics of patients who received ACEIs/A2RBs vs those who did not (Table 5). On univariate analysis, patients who did not receive ACEIs/A2RBs were characterized by increased admission BUN and SCr, reduced eGFR on admission, greater likelihood of usage of inotropes, darbepoetin, and β-blockers, and lower prevalence of hypertension. These results suggest that ACEI/A2RB usage may have been limited by two major factors: severity of ADCHF (usage of inotropes) and renal insufficiency on admission (increased BUN and SCr, reduced eGFR, and darbepoetin usage).
Despite these baseline differences, suggesting greater severity of disease in patients not given ACEI/ARB, multivariate analysis demonstrated a lack of ACEI/A2RB usage still emerges as an independent risk factor for mortality (Table 4). To better understand the role of ACEI/ARB usage, we next determined separately risk factors for mortality in those patients who received ACEIs/A2RBs (n=251) vs those who did not (n=168; Tables 6 and 7). By univariate analysis, risk factors for mortality in patients who received ACEIs/A2RBs were inotrope usage, absence of CAD, development of CRS1 regardless of definition, and reduced eGFR on admission (Table 6). On multiple logistic regression analysis, only reduced eGFR on admission and development of CRS1 defined by ∆SCr ≥0.5 mg/dL were independent predictors of in-hospital mortality (Table 8). Similar results were obtained for patients who did not receive ACEIs/A2RBs. Risk factors on univariate analysis were inotrope usage, development of CRS1 regardless of definition, darbepoetin usage, and greater age (Table 7). Independent predictors of mortality were greater age and development of CRS1 defined by ∆SCr ≥0.5 mg/dL (Table 9). For both groups, the results of multiple logistic regression analysis were essentially unchanged when we repeated the analysis, retaining one or the other definitions of CRS1, but not both, in the forward variable selection (Tables 8 and 9).
Taken together, these data suggest that irrespective of ACEI/A2RB usage, the most important risk factor for in-hospital mortality was the development of CRS1. This was true despite baseline differences between patients who received and did not receive ACEIs/A2RBs (Table 5), suggesting that any impact of these differences in determining risk of mortality is overridden by the occurrence of CRS1.
Comparison of risk factors for in-hospital mortality in ADCHF patients stratified according to development of CRS1
In light of the apparent dominance of CRS1 as a risk factor for mortality, we performed separate risk-factor analyses for patients who did and did not develop CRS1. Our aim in doing this was to clarify further the role of ACEI/A2RB usage and other potential risk factors distinct from that of the development of CRS1.
By univariate analysis, among patients who developed CRS1 defined by ∆SCr ≥0.3 mg/dL (n=144), risk factors for mortality were older age, severity of ADCHF (usage of inotropes and increased BNP), and baseline renal insufficiency (reduced eGFR and usage of darbepoetin). Of these, only older age and reduced eGFR on admission were independent predictors of mortality (Table 10). Similarly, among patients who developed CRS1 defined by ∆SCr ≥0.5 mg/dL (n=65), univariate risk factors for mortality were severity of ADCHF (increased BNP) and baseline renal insufficiency (usage of darbepoetin). There was no statistically significant difference among causes of ADCHF with the development of CRS1 defined as a rise in SCr ≥0.3 mg/dL (P=0.96) or CRS1 defined as a rise in SCr ≥0.5 mg/dL (P=0.97). On multivariate analysis, there were no independent predictors, most likely because of the small number of patients developing CRS1 by this definition.
Among patients who did not develop CRS1, univariate risk factors for mortality were the same, irrespective of whether CRS1 was defined by ∆SCr ≥0.3 mg/dL (n=275) or by ∆SCr ≥0.5 mg/dL (n=354). These were older age, severity of ADCHF (usage of inotropes, higher serum Na, elevated BUN, elevated BUN:SCr ratio), presence of hypertension, absence of CAD, lack of usage of β-blockers, and lack of usage of ACEIs/A2RBs. Of these, hypertension, higher serum Na, and lack of usage of ACEIs/A2RBs were independent predictors of mortality (Table 10). While the emergence of higher serum Na as an independent predictor of mortality in ADCHF patients may appear inconsistent with the reported literature,22 several studies have found that both hypernatremia and hyponatremia are associated with increased mortality in patients with ADCHF.23
To confirm the association between lack of usage of ACEIs/A2RBs and in-hospital mortality when patients were stratified according to the development of CRS1, we used Kaplan–Meier survival analysis (Figure 2). In accordance with the results of multivariate analysis, survival was significantly better with usage of ACEIs/A2RBs among patients who did not develop CRS1, irrespective of whether CRS1 was defined by ∆SCr ≥0.3 mg/dL (P=0.0048) or by ∆SCr ≥0.5 mg/dL (P=0.0499). Among patients who developed CRS1, though there was a trend toward improved survival with ACEI/A2RB usage, this effect was not significant. These analyses demonstrate the potential dominance of CRS1 as a risk factor for mortality in patients with ADCHF that may blunt the survival advantage of ACEI/A2RB use.
Discussion
The development of CRS1 is a complex and multifactorial pathophysiological disorder, with abnormalities or imbalances within multiple systems, including the RAAS, sympathetic nervous system, venous circulation, renal hemodynamics, and endogenous renal vasodilators and constrictors. As a result, it is likely that CRS1 is not one single entity, but instead comprised of several distinct entities, each with its own pathophysiological mechanism and its own potentially distinct impact on mortality.1,10 Therapeutic measures that can lead to WRF, such as the use of ACEIs/A2RBs, may not necessarily increase the mortality associated with CRS1, and under certain circumstances may even improve clinical outcome.8,15,24,25 Therefore, teasing apart the interaction and independent roles of CRS1 and ACEI/A2RB usage in determining in-hospital mortality among patients admitted with ADCHF can be extremely challenging.
In this study, we applied a risk-adjusted approach to determine the effect of ACEI/A2RB usage on short-term in-hospital mortality in a cohort of elderly ADCHF patients. Specifically, we sought to distinguish the role of ACEI/A2RB usage independently of that of the development of CRS1, a known risk factor for in-hospital mortality.4,5,26,27 Overall, our data suggest that lack of ACEI/A2RB usage and the development of CRS1 are statistically independent predictors, with the development of CRS1 being the stronger of the two risk factors for in-hospital mortality.
Our study population consisted of 2,361 consecutive elderly patients admitted with a diagnosis of ADCHF to a nonteaching community hospital. Risk-factor analysis was limited to a cohort of 419 patients for whom we had complete clinical and laboratory data. For both the entire study population and the cohort of 419 patients, the development of CRS1 was strongly associated with in-hospital mortality (Tables 1 and 3). Indeed, as demonstrated by multivariate analysis, the development of CRS1 was the strongest independent predictor of mortality (Table 4). This was true irrespective of the definition of CRS1, ∆SCr ≥0.3 mg/dL or as ∆SCr ≥0.5 mg/dL. Notably, in accord with previous studies by Daman et al and Parikh et al,28–30 our data suggest that increasing severity of CRS1 is associated with an increasing risk of mortality. This was evident in several ways. First, on univariate analysis, the OR for mortality was more than double for patients developing CRS1 defined by ∆SCr ≥0.5 mg/dL vs those developing CRS1 defined by ∆SCr ≥0.3 mg/dL (Table 3). This was confirmed on multivariate analysis, as the β-coefficient for development of CRS1 defined by ∆SCr ≥0.5 mg/dL was around double that of CRS1 defined by ∆SCr ≥0.3 mg/dL (Table 4). Second, when patients were stratified according to ACEI/A2RB usage, development of CRS1 regardless of definition persisted as the strongest predictor of mortality (Tables 8 and 9). In both cases, the β-coefficient for development of CRS1 was greater with the stricter definition of CRS1. Finally, by Kaplan–Meier survival analysis, a significant difference in mortality was observed only when patients were stratified according to the stricter definition of CRS1 (Figure 1).
Therefore, while development of CRS1 is associated with increased mortality among elderly patients admitted for ADCHF, its specificity as a risk factor appears to increase with the strictness of the definition of CRS1. These findings are consistent with those of a meta-analysis in ADCHF patients demonstrating a biological gradient between severity of CRS1 and increased mortality.28
The role of ACEI/A2RB usage is more complex, and its effects on survival must be disentangled from its effects on the development of CRS1. For example, an association between ACEI/A2RB usage and reduced mortality may occur through renal protection and reduced incidence of CRS1, or it may even be independent of the renal effects of RAAS blockade. In this study, ACEI/A2RB usage was associated with reduced mortality within both the entire population (Table 1) and the study cohort (Table 2). ACEI/A2RB usage was also associated with reduced incidence of CRS1 in the study cohort, though only when a stricter definition of CRS1 was applied (Table 2). Notably, as shown by multivariate analysis (Table 4), at least part of the protective association between ACEI/A2RB usage and reduced mortality was independent of an effect of ACEI/A2RB usage on the likelihood of developing CRS1. Therefore, regardless of the definition of CRS1, lack of ACEI/A2RB usage emerged as an independent risk factor for mortality. In fact, when the stricter definition of CRS1 was applied (∆SCr ≥0.5 mg/dL), the β-coefficient for ACEI/A2RB usage was exceeded only by that for the development of CRS1 (Table 4).
These data do not in and of themselves establish a causal relationship between ACEI/A2RB usage and reduced mortality. Lack of ACEI/A2RB use may instead be a surrogate for another direct determinant of mortality, such as circulatory and/or renal limitations of ACEI usage, including WRF and hyperkalemia, and accounted for their failure to be on ACEIs/A2RBs during an index hospitalization. For example, failure to use ACEIs/A2RBs may reflect physicians’ concerns over the potential adverse effects of RAAS blockade, especially WRF, and thus be a marker of increased severity of ADCHF, an obvious risk factor of mortality. Possibly consistent with this interpretation, univariate comparison of the subgroups of patients receiving vs not receiving ACEIs/A2RBs suggested that ACEI/A2RB usage was limited by two major factors: severity of ADCHF and baseline renal insufficiency (Table 5). Nevertheless, despite these differences between patients who received and did not receive ACEIs/A2RBs, the most important risk factor of in-hospital mortality in both subgroups by multivariate analysis remained the development of CRS1 (Tables 8 and 9). In fact, markers of the severity of ADCHF were not retained as independent predictors of mortality. Rather, for patients receiving ACEIs/A2RBs, reduced eGFR upon admission was the only other independent predictor, while for patients not receiving ACEIs/A2RBs, more advanced age was the only other predictor.
To clarify the role of ACEI/A2RB usage, distinct from that of development of CRS1, we performed separate risk-factor analyses for patients who did and did not develop CRS1. By Cox proportional-hazard analysis, among patients who did not develop CRS1, irrespective of definition, independent risk factors for mortality were presence of hypertension, lack of ACEI/A2RB usage, and higher serum Na (Table 10). Among patients who developed CRS1 defined by ∆SCr ≥0.3 mg/dL, independent risk factors were greater age and reduced eGFR on admission. Finally, among patients who developed CRS1 by the stricter definition of ∆SCr ≥0.5 mg/dL, there were no independent predictors, most likely because of the small number of patients developing CRS1 by this definition.
These results were confirmed by Kaplan–Meier survival analysis. As with Cox proportional-hazard analysis, survival was significantly better with ACEI/A2RB usage among patients who did not develop CRS1, irrespective of definition. Among patients who developed CRS1, there was an insignificant trend toward improved survival with ACEI/A2RB usage. From a management perspective, it is clearly impossible to predict which patients will develop CRS1. While the beneficial association with ACEI/A2RB usage is confined to patients not developing CRS1, the absence of an adverse association and even a trend toward benefit among patients developing CRS1 can be seen as encouraging.
It is worth noting that two established risk factors for CRS1 in the setting of ADCHF — use of nonsteroidal anti-inflammatory drugs (NSAIDs) and radiographic contrast dye1,31,32 — seem not to have played a role in the current study. No patient in our study was prescribed NSAIDs at the time of admission, nor was any patient administered NSAIDs while hospitalized. We cannot exclude the possibility that patients took NSAIDs without prescription prior to hospitalization. Also, no patient received an acute angiographic procedure, since the hospital was not approved for acute coronary angiographic intervention during the period of study.
There are several limitations to our study. First, its retrospective nature limited our ability to determine and adjust for all differences in baseline characteristics and comorbidities. Second, there were insufficient data to adjust for unmeasured potential confounders, such as proteinuria,1 or markers of clinical response, such as increased urine output. Third, there were insufficient data to adjust for titration of ACEI/A2RB dose or exact timing and duration of ACEI/A2RB administration. Furthermore, there were insufficient data to determine if there occurred cardiohemodynamic instability limiting ACEI/A2RB use or resulting in the discontinuation of therapy. Therefore, stratification of patients into ACEI/A2RB usage vs nonusage was based solely on in-hospital administration. Finally, the diagnosis of ADCHF was based solely on clinical criteria, and did not include measurements of ejection fraction or systolic function.
The phenomenon of ecological fallacy in a sense is a potential issue for any retrospective study in which subgroups are analyzed. Awareness of this issue helped to guide our approach and analysis. As such, we analyzed the potential impact of ACEIs/A2RBs not only by several stratifications — entire population (Tables 1 and 2), survivors vs nonsurvivors (Tables 3 and 4), CRS1 vs No CRS1 (Table 10), and ACEIs/A2RBs vs no ACEIs/A2RBs (Tables 5–7) — but also by complementary statistical approaches (multivariate and Kaplan–Meier survival analyses). The consistency among these approaches and analyses, while in no way conclusive, does suggest the potential importance of our findings and indicates the need for future prospective controlled studies.
Despite these limitations, a major strength of our study is its study population, which comes from a large community hospital and is thus clinically and demographically similar to elderly ADCHF patients in the general population. The rate of ACEI/A2RB use in our patient population was consistent with published heart-failure registry data that demonstrated wide variability in ACEI/A2RB use in eligible hospitalized patients: 56%–87%.33,34 Moreover, sufficient data were available to permit adjustment for many comorbidities and prognostic factors known to affect the clinical outcome of elderly ADCHF patients.
In summary, we report that within a cohort of elderly patients admitted with a diagnosis of ADCHF, the most dominant risk factor for short-term in hospital mortality was the development of CRS1. The strength of this risk factor is supported by its graded effect, with increasing severity of CRS1 associated with increased risk of mortality. Lack of ACEI/A2RB usage also emerged as an independent risk factor for mortality in the entire cohort. On subgroup analysis, although this association was significant only among patients not developing CRS1, no adverse association or even a trend toward a beneficial association was seen in patients who developed CRS1. This suggests at worst a neutral effect associated with the decision to use ACEIs/A2RBs. While it remains unclear whether lack of ACEI/A2RB usage is causally related to increased mortality or merely an epiphenomenon reflective of another risk factor inducing physicians to forego ACEIs/A2RBs, our findings nonetheless indicate the need to address this issue in future prospective studies.
Ethics approval and informed consent
This study was undertaken in accordance with the principles of the Declaration of Helsinki and the standards of good clinical practice. The study was approved by the Institutional Review Board and Ethics Committee (06–007) of Robert Wood Johnson/Barnabas Health Community Medical Center. Because of the retrospective study design, the requirement for patient consent was waived as per Institutional Review Board decision and in accordance with title 45, part 46 of the US Department of Health and Human Services’ Code of Federal Regulations. Patients’ data were kept confidential, and no patient’s identifier was included in data files handled for the purposes of this study.
Data use
The data sets generated and/or analyzed during the current study are not publicly available, due to the fact that they contain human–patient data and protected medical history. Institutional Review Board approval is limited to use by study investigators only, and does not extend to any other users. Data sets are available from the corresponding author on reasonable request, but only after Institutional Review Board approval for their use has been obtained.
Acknowledgment
This work was supported by institutional funds from Dr José A Arruda and the Section of Nephrology, University of Illinois at Chicago (to JSL).
Author contributions
JI was the principal investigator and participated in study design, statistical analysis, manuscript creation and preparation, data management, and review of the literature. SG participated in study design, review of the literature, and copyediting of the manuscript. KJL participated in study design and review of the literature. CSP participated in study design, review of the literature, and statistical analysis. JSL was the senior investigator and participated in study design, statistical analysis, manuscript editing and preparation, and review of the literature. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Ronco C, Cicoira M, McCullough PA. Cardiorenal syndrome type 1: pathophysiological crosstalk leading to combined heart and kidney dysfunction in the setting of acutely decompensated heart failure. J Am Coll Cardiol. 2012;60(12):1031–1042. | ||
Heywood JT. The cardiorenal syndrome: lessons from the adhere database and treatment options. Heart Fail Rev. 2005;9(3):195–201. | ||
Hu W, He W, Liu W, et al. Risk factors and prognosis of cardiorenal syndrome type 1 in elderly Chinese patients: a retrospective observational cohort study. Kidney Blood Press Res. 2016;41(5):672–679. | ||
Forman DE, Butler J, Wang Y, et al. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol. 2004;43(1):61–67. | ||
Butler J, Forman DE, Abraham WT, et al. Relationship between heart failure treatment and development of worsening renal function among hospitalized patients. Am Heart J. 2004;147(2):331–338. | ||
Lu KJ, Kearney LG, Hare DL, et al. Cardiorenal anemia syndrome as a prognosticator for death in heart failure. Am J Cardiol. 2013;111(8):1187–1191. | ||
Legrand M, Mebazaa A, Ronco C, Januzzi JL Jr. When cardiac failure, kidney dysfunction, and kidney injury intersect in acute conditions: the case of cardiorenal syndrome. Crit Care Med. 2014;42(9):2109–2117. | ||
Kane JA, Kim JK, Haidry SA, Salciccioli L, Lazar J. Discontinuation/Dose reduction of angiotensin-converting enzyme Inhibitors/Angiotensin receptor blockers during acute decompensated heart failure in African-American patients with reduced left-ventricular ejection fraction. Cardiology. 2017;137(2):121–125. | ||
Salah K, Kok WE, Eurlings LW, et al. Competing Risk of Cardiac Status and Renal Function During Hospitalization for Acute Decompensated Heart Failure. JACC Heart Fail. 2015;3(10):751–761. | ||
Damman K, Testani JM. The kidney in heart failure: an update. Eur Heart J. 2015;36(23):1437–1444. | ||
Voors AA, Davison BA, Felker GM, et al; Pre-RELAX-AHF study group. Early drop in systolic blood pressure and worsening renal function in acute heart failure: renal results of Pre-RELAX-AHF. Eur J Heart Fail. 2011;13(9):961–967. | ||
Wattad M, Darawsha W, Solomonica A, et al. Interaction between worsening renal function and persistent congestion in acute decompensated heart failure. Am J Cardiol. 2015;115(7):932–937. | ||
Kittleson M, Hurwitz S, Shah MR, et al. Development of circulatory-renal limitations to angiotensin-converting enzyme inhibitors identifies patients with severe heart failure and early mortality. J Am Coll Cardiol. 2003;41(11):2029–2035. | ||
Metra M, Nodari S, Parrinello G, et al. Worsening renal function in patients hospitalised for acute heart failure: clinical implications and prognostic significance. Eur J Heart Fail. 2008;10(2):188–195. | ||
Berra G, Garin N, Stirnemann J, et al. Outcome in acute heart failure: prognostic value of acute kidney injury and worsening renal function. J Card Fail. 2015;21(5):382–390. | ||
Schmidt M, Mansfield KE, Bhaskaran K, et al. Serum creatinine Elevation after renin-angiotensin system blockade and long term cardiorenal risks: cohort study. BMJ. 2017:356:j791. | ||
Clark H, Krum H, Hopper I. Worsening renal function during renin-angiotensin-aldosterone system inhibitor initiation and long-term outcomes in patients with left ventricular systolic dysfunction. Eur J Heart Fail. 2014;16(1):41–48. | ||
Centers for Medicare and Medicaid Services National Heart Failure Quality Improvement Project. United States Department Health and Human Services; 2001;1–13. | ||
US Health Care Financing Administration. Diagnosis-related Groups Definitions Manual. Wallingford CT: 3M Health Information Services; 1993. | ||
Rule AD, Larson TS, Bergstralh EJ, Slezak JM, Jacobsen SJ, Cosio FG. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Ann Intern Med. 2004;141(12):929–937. | ||
Zafrir B, Amir O. Beta blocker therapy, decompensated heart failure, and inotropic interactions: current perspectives. Isr Med Assoc J. 2012;14(3):184–189. | ||
Deubner N, Berliner D, Frey A, et al. Dysnatraemia in heart failure. Eur J Heart Fail. 2012;14(10):1147–1154. | ||
Gheorghiade M, Abraham WT, Albert NM, et al; OPTIMIZE-HF Investigators and Coordinators. Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE-HF registry. Eur Heart J. 2007;28(8):980–988. | ||
Testani JM, Brisco MA, Chen J, McCauley BD, Parikh CR, Tang WH. Timing of hemoconcentration during treatment of acute decompensated heart failure and subsequent survival: importance of sustained decongestion. J Am Coll Cardiol. 2013;62(6):516–524. | ||
Damman K, Tang WH, Testani JM, McMurray JJ. Terminology and definition of changes renal function in heart failure. Eur Heart J. 2014;35(48):3413–3416. | ||
Damman K, Valente MA, Voors AA, O’Connor CM, van Veldhuisen DJ, Hillege HL. Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J. 2014;35(7):455–469. | ||
Krishnamoorthy A, Greiner MA, Sharma PP, et al. Transient and persistent worsening renal function during hospitalization for acute heart failure. Am Heart J. 2014;168(6):891–900. | ||
Damman K, Navis G, Voors AA, et al. Worsening renal function and prognosis in heart failure: systematic review and meta-analysis. J Card Fail. 2007;13(8):599–608. | ||
Parikh CR, Coca SG, Wang Y, Masoudi FA, Krumholz HM. Long-term prognosis of acute kidney injury after acute myocardial infarction. Arch Intern Med. 2008;168(9):987–995. | ||
Cruz DN. Cardiorenal syndrome in critical care: the acute cardiorenal and renocardiac syndromes. Adv Chronic Kidney Dis. 2013;20(1):56–66. | ||
Akinbamowo AO, Salzberg DJ, Weir MR. Renal consequences of prostaglandin inhibition in heart failure. Heart Fail Clin. 2008;4(4):505–510. | ||
Scott PA, Kingsley GH, Scott DL. Non-steroidal anti-inflammatory drugs and cardiac failure: meta-analyses of observational studies and randomised controlled trials. Eur J Heart Fail. 2008;10(11):1102–1107. | ||
Fonarow GC. Adherence to heart failure quality-of-care indicators in US hospitals. Arch Intern Med. 2005;165(13):1469–1477. | ||
Gheorghiade M, Filippatos G. Reassessing treatment of acute heart failure syndromes: the adhere registry. Eur Heart J Suppl. 2005;7(suppl_B):B13–B19. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.