Back to Journals » Patient Preference and Adherence » Volume 10
Insulin glargine 300 U/ml in the management of diabetes: clinical utility and patient perspectives
Authors de Galan BE
Received 27 July 2016
Accepted for publication 27 September 2016
Published 17 October 2016 Volume 2016:10 Pages 2097—2106
DOI https://doi.org/10.2147/PPA.S92123
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Bastiaan E de Galan
Department of Internal Medicine, Radboud University Medical Center, Nijmegen, the Netherlands
Abstract: There is ongoing interest in optimizing basal insulin treatment by developing insulins with a flat pharmacological profile, a long duration of action (typically beyond 24 hours) and minimum day-to-day variation. Glargine-300 is a modified form of the long-acting insulin analog glargine in that it has been concentrated at 300 units/mL rather than the conventional 100 units/mL. Glargine-300 has a longer duration of action and a flatter pharmacological profile than original glargine-100. This property allows for more flexibility around the timing of administration, when injected once per day. Open-label studies in patients with diabetes have shown that treatment with glargine-300 achieves comparable glycemic control compared to treatment with glargine-100, albeit with consistently higher insulin requirements. These studies also showed that treatment with glargine-300 was associated with lower risks of nocturnal hypoglycemia in patients with type 2 diabetes, particularly those already on insulin, whereas data are mixed in insulin-naïve patients with type 2 diabetes or in patients with type 1 diabetes. Treatment with glargine-300 did not appear to affect the risk of overall hypoglycemia, whereas studies lacked sufficient power to investigate the effect on the risk of severe hypoglycemia. Future studies need to establish the role of glargine-300 in the treatment of diabetes alongside the other new long-acting insulin analog, insulin degludec, which was recently introduced to the market.
Keywords: insulin glargine-300, type 1 diabetes, type 2 diabetes, hypoglycemia, HbA1c, patient-reported outcomes
Introduction
Diabetes is a rapidly increasing global health problem. As of 2015, the World Health Organization (WHO) has estimated that over 415 million adults have been diagnosed with diabetes, a number expected to have risen by more than 50% by 2040.1 In the US, about a third of people with diabetes are treated with insulin.2 The number of patients requiring insulin is expected to rise more steeply. Factors contributing to this rise include longer life expectancy for people with diabetes,3 the aging of the population as a whole,4 the younger age at which both type 1 and type 2 diabetes are being diagnosed,5,6 better resource facilities for low- and middle-income countries7 and the continuation of the obesity epidemic that tends to start at younger ages.8
Basal, ie so-called long-acting, insulin agents form the backbone of most therapeutic insulin regimens. Indeed, the majority of patients with type 1 diabetes are treated with basal-bolus insulin injection regimens consisting of a once- or twice-daily long-acting insulin agent in combination with a rapid-acting insulin (analog) given prior to meals. For people with type 2 diabetes, most guidelines recommend to add basal insulin when glycemic control can no longer be maintained with alternative (usually oral) glucose-lowering treatment(s) alone,9,10 particularly in patients with impaired fasting glucose levels. Parenthetically, it should be acknowledged that the terms “long-acting” or “rapid-acting” are factually misused, as all insulins have the same duration of action once in their free form in the circulation. Thus, the term “long-acting” for particular insulin products refers to the protracted uptake of these insulins from the subcutaneous depot into the circulation or their binding to albumin from which the insulin is slowly freed.
Of the long-acting insulin agents currently available, neutral protamine Hagedorn (NPH) insulin is the insulin that is around for the longest time. Some now call this insulin intermediate-acting, because its duration of action rarely exceeds 14 hours.11 At the turn of the century, the insulin analogs glargine and detemir were marketed as alternatives to NPH insulin, as they exhibited longer duration of action that would typically provide 24-hour coverage. The duration of action is slightly longer for glargine than for detemir, although large inter-individual differences exist.11,12 Glargine has less of a peak than either NPH insulin or detemir, although the assertion that it had no peak at all was flawed from the start.13 Detemir, on the other hand, was claimed to have a more predictable glucose-lowering action than either NPH insulin or glargine.13 Both of these features have been hypothesized to explain why the use of these long-acting insulin analogs may be associated with reduced risks of (particularly) nocturnal hypoglycemia when compared to NPH insulin.14 Combining rapid-acting analogs before meals with a long-acting insulin analog before bedtime has become the default insulin treatment for patients on multi-injection basal-bolus insulin regimens, particularly those with type 1 diabetes.
Nevertheless, current insulin regimens are still far from being perfect. Iatrogenic hypoglycemia remains the barrier for optimal glucose control for both type 1 and type 2 diabetes patients on insulin,15 a problem that long-acting insulin analogs have failed to alleviate. Insulin analogs with longer duration of action, flatter profiles, and less intra- and inter-individual variations are urgently needed to allow for better glucose control at lower risk of hypoglycemia. Glargine-300 is a “new” long-acting insulin analog, recently approved by both the US Food and Drug Administration and European Medicines Evaluation Agency for marketing in the US and Europe, respectively. Glargine-300 is a three times more concentrated formulation of “traditional” glargine, ie, 300 units/mL versus 100 units/mL. In this review, I will summarize available evidence regarding the efficacy of glargine-300 with respect to important patient outcomes, including glycemic control (as reflected by glycated hemoglobin [HbA1c]), hypoglycemia and quality of life.
Pharmacokinetics and pharmacodynamics of glargine-100 and glargine-300
NPH insulin consists of a complex of insulin, zinc and the fish protein protamine, in which the latter component reduces the solubility of NPH within the subcutaneous area, thus delaying its absorption into the circulation. However, the insulin molecule itself is structurally unaltered.16 A limitation of NPH insulin is its need for resuspension before injection, thus contributing to large variation in glucose-lowering effects.17 Glargine has a modified molecular structure in that two arginine residues are added to the C-terminus of the B-chain and glycine replaces asparagine at position 21 of the A-chain of the insulin molecule. These alterations result in the shifting of isoelectric point to a lower pH, which reduces its solubility at the physiologic pH of the injection site.18 Glargine is therefore kept as an acidic solution, quickly forming microprecipitates after injection in the neutral environment of subcutaneous tissue. The insulin then slowly dissipates from these microprecipitates, allowing it to be absorbed into the circulation.19
The microprecipitates explain the more gradual appearance of insulin in the circulation and hence its flatter insulin profile than NPH, although as said earlier, it is not completely peakless. Glargine has an onset of action of 3–4 hours and a half-life of 12–14 hours for clinically relevant doses with a duration of glucose-lowering action of ~24 hours.17 Dosing once a day is usually sufficient, except when very low doses are being used, such as in young children and extremely insulin-sensitive adults with type 1 diabetes.
The molecular structure of glargine-300 is not different from that of glargine in the usual 100 units/mL concentration. Nevertheless, glargine-300 has a flatter pharmacokinetic and pharmacodynamic profile than the original formulation, with slower onset of action and an extended duration of glucose-lowering action by at least several hours.20 The reason for the differences in pharmacological efficacy between glargine-300 and original glargine has not been entirely clarified, but the surface dependency of insulin release from the precipitates has been suggested as a potential explanation.21 It is also possible that more condensed formulation gives it greater structural strength and relative resistance against degradation. Remarkably, however, despite its longer duration of action, biological availability is ~10% lower.20 This observation suggests that some amount of glargine-300 does not form microprecipitates or that longer presence in the subcutaneous area somehow enhances its degradation, although this remains speculative.
Clinical studies
The clinical efficacy and safety of treatment with glargine-300 have been examined in people with type 1 and type 2 diabetes in various trials of the so-called EDITION program and in one study using continuous glucose monitoring (CGM, Table 1).22–27 All trials were open-label, reportedly because of the different pen systems used to inject glargine-300 or glargine-100, which may have introduced bias. The primary end point of all EDITION trials was the change in HbA1c levels from baseline to end of treatment, but a strict treat-to-target protocol of weekly insulin dose adjustments was used to obtain fasting glucose levels of 4.4–7.2 mmol/L in type 1 and of 4.4–5.6 mmol/L in type 2 diabetes. As a consequence, differences in the end-of-study HbA1c levels between the active compound and comparator (ie, glargine-100) study arms were kept to a minimum, yet these protocols provided little guidance with respect to avoiding hypoglycemia.
Hypoglycemia, severe, nocturnal or any, was the most important secondary end point for these trials. The term “any hypoglycemia” was used for all events reported as hypoglycemia, whether accompanied by symptoms or not or confirmed with a self-measured glucose value or not. Confirmed hypoglycemia was defined as a documented glucose value at or below 3.9 mmol/L, with or without symptoms, and severe hypoglycemia as an event requiring assistance from another person for treatment. Hypoglycemic events with a cutoff at 3.0 mmol/L were analyzed separately. Instructions with respect to performing self-measured plasma glucose (SMPG) by finger stick differed from one study to an other, depending on the intensity of insulin treatment, but were similar between the study arms. As a consequence, comparing rates of hypoglycemia between studies can only be done with great caution. Another cautionary note is that SMPG frequency was not recorded; since all studies were open-label, the rate at which SMPG was performed may not necessarily be balanced between the study arms, although the direction of such potential bias remains unclear.
Sanofi Aventis was the sponsor of the EDITION trial program and was actively involved in trial design, data collection, management and interpretation, statistical analysis, and writing of the manuscripts.
Type 1 diabetes
EDITION4 and EDITIONJP1 were phase III studies conducted in patients with type 1 diabetes, the latter exclusively in Japanese patients, comprising 549 and 243 participants, respectively.25,26 In both studies, the vast majority of patients used glargine-100 at baseline and only a small minority injected basal insulin twice daily. Patients were randomized 1:1 to either glargine-300 or glargine-100 and were instructed to adjust the dose of glargine-300 by 1.5–4.5 units and that of glargine-100 by 1.0–4.0 units to achieve the beforementioned fasting glucose target. In EDITION4, half of the study population was instructed to inject the basal insulin in the evening (between evening meal and bedtime), and the other half was instructed to inject in the morning (ie, between prebreakfast and lunch).
In both studies, HbA1c levels decreased to a similar extent in both randomized groups, with the upper bound of the mean differences between the two treatments being within the prespecified margin of 0.4% (4.4 mmol/mol), indicating non-inferiority of glargine-300 in comparison to glargine-100 (Figure 1). There were no differences between morning and evening injectors. A small-scale study that compared the effect of 4 weeks of glargine-300 with that of glargine-100 in 20 people with type 1 diabetes using a cross-over design reported no differences between the two treatments on glucose variability measured by 3-day CGM recordings.28 In all studies, patients randomized to glargine-300 on average increased their basal insulin doses more than patients randomized to comparator treatment, the difference ranging from 12% to >20%, with mealtime insulin doses remaining largely unchanged.
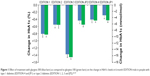  | Figure 1 Effect of treatment with glargine-300 (blue bars) as compared to glargine-100 (green bars) on the change in HbA1c levels in 6-month EDITION trials in people with type 1 diabetes (EDITION 4 and JP1) or type 2 diabetes (EDITION 1, 2, 3 and JP2).22–27 |
More than 90% of patients examined in the EDITION studies reported hypoglycemia, many of which were confirmed by glucose measurements and most were recorded during daytime. In EDITIONJP1, glargine-300 was associated with 20% and 34% lower relative risks for any confirmed or severe hypoglycemia and for such events during the night (0:00–05:59 hours, Table 2), respectively.26 However, these lower risks were mainly driven by risk reductions observed in the first 8 weeks, when insulin was titrated. In EDITION4, glargine-300 reduced the rate of nocturnal hypoglycemic episodes by 31% during the first 8 weeks, but had no risk-reducing effect beyond that time point, so that the risk reduction over the full 6-month period was a nonsignificant 10% (Table 2). There were no differences in the risk of documented hypoglycemia at any time of the day between the two treatments, irrespective of whether such an event was defined by a glucose value ≤3.9 mmol/L or <3.0 mmol/L.25 Severe hypoglycemia occurred numerically more often in patients randomized to glargine-100 than in those randomized to glargine-300, but such events were too uncommon to analyze statistically with sufficient accuracy. In both trials, the increase in body weight was somewhat less in patients assigned glargine-300 than in those assigned glargine-100. There were no differences in injection site reactions or other treatment-related adverse events between glargine-300 and glargine-100.
  | Table 2 Nocturnal hypoglycemia in studies on glargine-300 |
Type 2 diabetes
Four published phase III EDITION studies have thus far been conducted in patients with type 2 diabetes: EDITION1 in patients on basal-bolus insulin regimens (n=807),22 EDITION2 in patients on oral agents and basal insulin only (n=811),23 EDITION3 in insulin-naïve patients failing on oral agents (n=878)24 and EDITIONJP2 in Japanese patients on basal insulin (with/without oral agents, n=241).27 As in the trials involving patients with type 1 diabetes, all studies were conducted for a duration of 6 months, were multicenter and multinational (except in the Japanese trial), had an open-label study design and randomized patients 1:1 to either glargine-300 or glargine-100 once daily, to be administered in the evening. The protocols for achieving the fasting plasma glucose target had the minimal insulin dose adjustment set at 3.0 units, except in the Japanese trial where this was 1.5 units for glargine-300 and 1.0 unit for glargine-100.27
In the four studies conducted in people with type 2 diabetes, glargine-300 was as effective as glargine-100 in lowering HbA1c levels (Figure 1) and in increasing the proportion of patients achieving glycemic targets (ie, HbA1c <53 mmol/mol [7%]). In neither study did the upper confidence limit of the mean difference between the two treatments exceed the 4.4 mmol/mol (0.4%) margin, thus establishing non-inferiority of glargine-300. There were similar reductions in fasting plasma glucose, self-measured pre-meal glucose values and in 7- or 8-point self-measured glucose profiles (performed only in patients on basal-bolus insulin regimens) across the two randomized treatments. In general, the doses of glargine-300 and of glargine-100 were gradually increased in all patients, but more so in patients randomized to glargine-300, who ended with about 10%–17% greater basal insulin doses than those randomized to glargine-100. In EDITION 1, mealtime insulin use remained unchanged from baseline to end of follow-up and did not differ between glargine-300 and glargine-100 users.22
As expected, hypoglycemia was reported less frequently by patients with type 2 diabetes than those with type 1 diabetes and depended on the insulin treatment regimen, ie, the frequency was highest in patients on basal-bolus insulin regimens (EDITION 1) and lowest in insulin-naïve patients who started basal insulin alone (EDITION 3). Across studies, confirmed (ie, documented by self-measurement) nocturnal or severe nocturnal hypoglycemia occurred less frequently and among fewer people in the glargine-300 study arm than in the glargine-100 study arm. In EDITION 1–3 studies, 6 months of treatment with glargine-300 reduced the population at risk for nocturnal hypoglycemia by 22%–37%. The rate of such events was reduced by about a third in patients already on insulin, but was not affected in insulin-naïve patients with type 2 diabetes (Table 2). Although most of the difference in risk for nocturnal hypoglycemia between glargine-300 and glargine-100 occurred in the first 8 weeks after randomization, it generally persisted for the remainder of the 6-month treatment period. For any confirmed or severe hypoglycemia, ignoring the first 8 weeks, the treatments resulted in mild (ie, ~10%) risk reductions that often failed to reach statistical significance. In EDITION JP2, the curves describing cumulative event rates for confirmed or severe nocturnal hypoglycemia over time started to diverge after 8 weeks of treatment with rates progressing about 50% slower in patients assigned glargine-300 compared to those assigned glargine-100.27 Severe hypoglycemia was so infrequent that it could not be analyzed. Two studies reported that use of glargine-300 caused 0.5 and 1.0 kg lower weight gain than use of glargine-100, respectively,23,27 but this weight benefit was not achieved in two other studies.22,24 Other adverse effects occurred at similar frequency in the glargine-300 and glargine-100 treatment arms.
Both EDITION1 and EDITION2 trials had a predefined extension period of another 6 months, during which participants were maintained on their assigned treatment.29,30 These extensions more or less confirmed the findings that were initially reported. Thus, glycemic control, as reflected by changes in HbA1c level, fasting glucose and self-measured glucose profiles, remained largely comparable between the two treatment arms from study start until the end of the extension period. The rate of confirmed nocturnal hypoglycemia remained 16%–37% lower in patients on glargine-300 compared to those on glargine-100, but the 6-month extension period did not appear to contribute to this difference. The annualized event rate of any confirmed hypoglycemia was not different between the two treatment arms in either of the two extension trials.
Meta-analyses
A prespecified meta-analysis of the first three EDITION trials showed 15% and 38% lower risks of any, and nocturnal, confirmed hypoglycemia (glucose ≤3.9 mmol/L), respectively, in patients with type 2 diabetes assigned glargine-300 as compared to those assigned glargine-100. The analysis revealed no differences with respect to HbA1c, fasting plasma glucose or self-measured glucose profiles.31 Network meta-analyses, also called mixed treatment comparisons, simultaneously pool data from both direct comparisons within randomized trials and indirect comparisons across trials with a common comparator (eg, placebo), to compare multiple (ie, three or more) treatment options.32 Such an analysis thus allows an estimation of comparative effects of interventions for which direct head-to-head comparisons are not yet available. In a recent network meta-analysis, 41 studies were included to compare the efficacy and safety of glargine-300 with various other basal insulins and with premixed insulin in patients with type 2 diabetes.33 The analysis focused on patients treated with basal insulin in conjunction with oral therapy, but not requiring meal-time insulin, for which 25 studies were found. This analysis revealed that glycemic control was comparable between glargine-300 and insulin detemir, NPH, degludec and premixed insulin. Glargine-300 was associated with a lower rate of nocturnal hypoglycemia (glucose <3.9 mmol/L) compared to the other insulin products, although this difference did not reach statistical significance for degludec and detemir.
Patient-reported outcomes
Most EDITION studies examined the effect of glargine-300 on treatment satisfaction and quality of life, as measured by the validated Diabetes Treatment Satisfaction Questionnaire (DTSQ) and EuroQol 5 Dimensions (EQ-5D) questionnaire, respectively. In EDITION1, treatment satisfaction increased somewhat more in patients randomized to glargine-300 than in those randomized to glargine-100.22 However, this improvement appeared unrelated to the frequency of perceived hypoglycemia, and the difference was no longer observed at the end of the 6-month extension period.29 Treatment satisfaction did not differ between randomized groups in the other three studies investigating this outcome. The two treatments also showed no differences with respect to perceived quality of life or fear of hypoglycemia. However, fear of hypoglycemia was assessed only in insulin-naïve patients with type 2 diabetes starting insulin and in patients with type 1 diabetes who had low baseline scores on the hypoglycemia-fear questionnaire.24,25
Glargine-300 in clinical context
The studies conducted thus far showed that glargine-300 was about as efficacious as glargine-100 and – by inference – other basal insulins in lowering HbA1c or in achieving targets for glycemic control. On a unit-by-unit comparison, the glucose-lowering effect of glargine-300 was ~20% lower than glargine-100, as reflected by the higher insulin doses required to obtain similar glycemic control at the end of follow-up. Some studies reported somewhat less weight gain in patients treated with glargine-300 than in those treated with conventional glargine. In patients with type 2 diabetes, treatment with glargine-300 was associated with about 25% lower rates of nocturnal hypoglycemia than treatment with glargine-100. This effect was also observed in patients with type 1 diabetes, but appeared to be limited largely to the first 8 weeks of treatment and not, or to much lesser extent, beyond that period. Severe hypoglycemia, defined as those events requiring assistance from another person, was so infrequent that it could not be analyzed with sufficient accuracy in any of the studies or in the meta-analyses.
A ~25% reduction in nocturnal hypoglycemia may seem trivial, because most hypoglycemic events occur during daytime (which were not affected by glargine-300 treatment) and because evidence is missing that this effect is mirrored by a similar reduction in severe hypoglycemia that is regarded as clinically more meaningful. However, many patients and their partners view nocturnal hypoglycemia as deeply disturbing and of more concern than events that occur during daytime.34 Nocturnal hypoglycemia causes loss of several hours of sleep when patients are awakened and retains a negative impact on sleep quality,35 even when patients do not awake.36 The majority of patients are fatigued and have a reduced functioning capacity the day following a nocturnal event, and many report taking or requiring a nap.36 Twenty to 30% of patients skip a day at the office or are unable to fulfill their tasks, thus falling behind in work productivity.37 Approximately 25% of patients contact their health care provider and 15% reduce their insulin doses.36 Finally, 50% of partners are also awakened by a nocturnal hypoglycemia in their spouse.35
Although the lower incidence of nocturnal hypoglycemia associated with glargine-300 was fairly consistent across studies, there are some potential flaws with the design of the EDITION studies that need to be discussed to assess the clinical relevance of this observation. First, one may question the definition of hypoglycemia as any SMPG value at or below 3.9 mmol/L. Although this was based on a recent consensus report from the American Diabetes Association,38 the report argued that this single threshold value, chosen mainly for pragmatic reasons, should be used as an alert value for people on medication known to cause hypoglycemia rather than as a strict separation between normal and below-normal glucose values, a vision that was recently reiterated by another expert group.39 Indeed, although plasma glucose levels ≤3.9 mmol/L usually elicit a counterregulatory hormone response in nondiabetic individuals, this threshold shifts to lower glucose values after antecedent hypoglycemia (eg, in well-controlled type 1 diabetes)40–42 and to higher values in poorly controlled diabetes.43 This concerns in particular the nocturnal period, because sleep attenuates counterregulatory responses and shifts its elicitation to lower glucose concentrations,44,45 so that plasma glucose values around the 3.9 mmol/L cutoff can still be considered physiologic. Also, glucose values well below 3.9 mmol/L are needed for the appearance of hypoglycemic warning symptoms, even in people without diabetes.43,46,47 Finally, the allowed imprecision of current point-of-care glucose meters and continuous glucose monitors precludes detection of hypoglycemia with sufficient accuracy when this is based on a very narrow distinction between normo- and hypoglycemia.48 The clinical relevance of using the 3.9 mmol/L threshold value can be further questioned, when considering the treat-to-target algorithm that was used by the trials. Importantly, the close proximity of the 4.4 mmol/L lower bound of the treat-to-target glucose range to the cutoff value may have amplified the number of “hypoglycemic” events, particularly during the night and in patients with the dawn phenomenon.49
The lower glucose-lowering potency of glargine-300 compared to glargine-100 underlies another methodological concern. In all EDITION studies, instructions for the initiation of insulin were based on prior insulin dose requirements or on body weight, which were similar for both glargine-300 and glargine-100 study arms, despite the lower potency of the first. Thereafter, insulin dose adjustments were generally performed once weekly and restricted by protocol to increase by no more than 6 units. Consequently, it took longer for the patients randomized to the glargine-300 study arms to reach the glucose targets in the treat-to-target insulin regimens than for the patients randomized to the glargine-100 study arms. Such relative underdosing of glargine-300 as compared to glargine-100 may have contributed to the lower hypoglycemic event rates, especially since the threshold for the definition of hypoglycemia was set at such a relatively high glucose level (mentioned earlier). Indeed, the differences in hypoglycemic incidence between glargine-300 and glargine-100 treatments were usually set during the first 8 weeks, when most of the dose titrations took place, particularly in the insulin-naïve population.
From a patient perspective, however, there are other potential benefits of glargine-300 over conventional glargine. Patients with profound insulin resistance who require very large doses of insulin may benefit from reduced injection site discomfort associated with the lower injection volume. A long-acting insulin with a longer half-life time suffers less from differences in timing of injection. Indeed, the product information leaflet of glargine-300 states that although the insulin is to be injected once daily, the time of administration may vary by 3 hours. A recent study demonstrated that increasing the insulin dosing range from 23–25 hours to 21–27 hours did not affect the efficacy and safety of glargine-300 in people with type 2 diabetes.50 More flexibility of glargine-300 may particularly benefit shift workers or other patients with large variation in sleeping time and hours awake, and to some extent may benefit patients frequently passing time zones. Another group likely to benefit (and who are usually excluded from clinical trials) are in- or outpatients who depend on nurses for the administration of insulin, particularly when the nurses have more tasks to perform and more patients to take care of. Finally, given the underlying mechanism of glargine, a more protracted release of insulin from the subcutaneous precipitates is expected to provide a more predictable glucose-lowering effect, resulting in less variation in glucose excursions. In daily practice, many patients complain about the poor reproducibility of the glucose-lowering effects of insulin, the variability of which can be as high as 68% for NPH insulin, but has still been estimated at 48% for glargine-100.13 A recent study showed a pharmacodynamic variability of ~35% for glargine-300 in people with type 1 diabetes,51 which appears somewhat less than what has been previously reported for glargine-100.13 Better reproducibility may be welcomed by patients, as it allows both more accurate dose titration and may improve confidence in the ability to self-control diabetes management.
Areas of uncertainty
All clinical trials performed thus far were severely underpowered to study the effect of glargine-300 on the risk of severe hypoglycemia. Examining patients at high risk of severe hypoglycemia, such as, those with impaired awareness of hypoglycemia, is eagerly awaited. An issue that remains to be resolved concerns the biochemical explanation for the observed longer duration of action of glargine-300 as compared to glargine-100. Resolving this issue is important for two reasons. From a clinical perspective, it would allow for better understanding of the trial data on glucose-lowering efficacy and hypoglycemic risks in people with diabetes. On a more fundamental level, however, revealing the underlying mechanism may also reveal whether it would be valuable to aim for further dose concentration of glargine (or of other long-acting insulins). Glargine-300 will be marketed for the same price as conventional glargine. However, expenditure is expected to increase by 10%–20% due to its lower potency. A cost-effectiveness study is needed to assess the justification for such higher expected costs. Glargine-300 is not the only “new” long-acting insulin on the market. Insulin degludec was recently introduced to the market. This insulin analog has a half-life that is about twice that of glargine-100, which results in a flat and stable glucose-lowering effect after steady-state conditions have been reached.52 The development of PEGylated insulin lispro, a long-acting insulin analog with hepatic preference and relatively lower peripheral hyperinsulinemia,53 has been recently stopped. Degludec has been reported to reduce the risk of nocturnal hypoglycemia in patients with both type 1 and type 2 diabetes, when compared to glargine-100,54 with recent analyses suggesting reductions in the risk of severe hypoglycemia in type 1 diabetes as well.55 Which of these next-generation long-acting insulin analogs perform better can only be satisfactorily answered by appropriately-sized head-to-head clinical trial comparisons. Such studies are underway and are urgently needed to provide guidance for clinicians as to which of these analogs fits best with individual patient requirements. Finally, future studies also need to address how well glargine-300 combines with newly developed glucose-lowering agents, including DPP-IV inhibitors, SGLT-2 inhibitors and, in particular, glucagon-like peptide-1 (GLP-1) receptor agonists. Indeed, adding GLP-1 receptor agonists to a long-acting insulin analog, sometimes in a fixed combination, is extensively investigated for the treatment of type 2 diabetes,56,57 but to date no studies have been published on combinations with glargine-300.
Conclusion
Glargine-300 is a new formulation of glargine that contains the same amount of insulin units in one-third of the volume of glargine-100. Glargine-300 has a prolonged and flatter pharmacokinetic and pharmacodynamic profile than glargine-100, allowing more flexibility for the timing of administration. Clinical studies suggest a lower risk of nocturnal hypoglycemia in people with insulin-requiring type 2 diabetes, although it remains to be determined whether this effect sustains over longer periods of time. Paradoxically, patients with type 1 diabetes, although at much greater risk of hypoglycemia than people with type 2 diabetes, seem to derive less hypoglycemia-reducing benefit from switching to glargine-300. Further study is required to establish the place of glargine-300 in clinical practice in relation to existing and newly developed long-acting insulin formulations.
Disclosure
The author has received honoraria for serving on advisory boards for Novo Nordisk (Bagsværd, Denmark) and Sanofi Aventis (Gentilly, France). The author reports no other conflicts of interest in this work.
References
International Diabetes Federation. IDF Diabetes Atlas. 7th ed. 2015. | ||
CDC. Prevention. CfDCa. Treating diabetes (insulin and oral medication use). Available from: http://www.cdc.gov/diabetes/statistics/treating_national.htm. Accessed July 18, 2016. | ||
Gregg EW, Cheng YJ, Saydah S, et al. Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: findings from the National Health Interview Survey. Diabetes Care. 2012;35(6):1252–1257. | ||
Sudharsanan N, Ali MK, Mehta NK, Narayan KM. Population aging, macroeconomic changes, and global diabetes prevalence, 1990–2008. Popul Health Metr. 2015;13:33. | ||
Pavkov ME, Hanson RL, Knowler WC, Bennett PH, Krakoff J, Nelson RG. Changing patterns of type 2 diabetes incidence among Pima Indians. Diabetes Care. 2007;30(7):1758–1763. | ||
Harjutsalo V, Sjöberg L, Tuomilehto J. Time trends in the incidence of type 1 diabetes in Finnish children: a cohort study. Lancet. 2008;371(9626):1777–1782. | ||
Gill GV, Yudkin JS, Keen H, Beran D. The insulin dilemma in resource-limited countries. A way forward? Diabetologia. 2011;54(1):19–24. | ||
Narayan KM, Boyle JP, Thompson TJ, Gregg EW, Williamson DF. Effect of BMI on lifetime risk for diabetes in the U.S. Diabetes Care. 2007;30(6):1562–1566. | ||
American Diabetes Association. 7. Approaches to glycemic treatment. Diabetes Care. 2016;39(Suppl 1):S52–S59. | ||
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American diabetes association and the European association for the study of diabetes. Diabetes Care. 2015;38(1):140–149. | ||
Lepore M, Pampanelli S, Fanelli C, et al. Pharmacokinetics and pharmacodynamics of subcutaneous injection of long-acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro. Diabetes. 2000;49(12):2142–2148. | ||
Koehler G, Treiber G, Wutte A, et al. Pharmacodynamics of the long-acting insulin analogues detemir and glargine following single-doses and under steady-state conditions in patients with type 1 diabetes. Diabetes Obes Metab. 2014;16(1):57–62. | ||
Heise T, Nosek L, Rønn BB, et al. Lower within-subject variability of insulin detemir in comparison to NPH insulin and insulin glargine in people with type 1 diabetes. Diabetes. 2004;53(6):1614–1620. | ||
Horvath K, Jeitler K, Berghold A, et al. Long-acting insulin analogues versus NPH insulin (human isophane insulin) for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2007;(2):CD005613. | ||
Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care. 2003;26(6):1902–1912. | ||
Deckert T. Intermediate-acting insulin preparations: NPH and lente. Diabetes Care. 1980;3(5):623–626. | ||
Heinemann L, Linkeschova R, Rave K, Hompesch B, Sedlak M, Heise T. Time-action profile of the long-acting insulin analog insulin glargine (HOE901) in comparison with those of NPH insulin and placebo. Diabetes Care. 2000;23(5):644–649. | ||
Wang F, Carabino JM, Vergara CM. Insulin glargine: a systematic review of a long-acting insulin analogue. Clin Ther. 2003;25(6):1541–1577. | ||
Dunn CJ, Plosker GL, Keating GM, McKeage K, Scott LJ. Insulin glargine: an updated review of its use in the management of diabetes mellitus. Drugs. 2003;63(16):1743–1778. | ||
Becker RH, Dahmen R, Bergmann K, Lehmann A, Jax T, Heise T. New insulin glargine 300 units mL-1 provides a more even activity profile and prolonged glycemic control at steady state compared with insulin glargine 100 units mL-1. Diabetes Care. 2015;38(4):637–643. | ||
Blair HA, Keating GM. Insulin Glargine 300 U/mL: a review in diabetes mellitus. Drugs. 2016;76(3):363–374. | ||
Riddle MC, Bolli GB, Ziemen M, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using basal and mealtime insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 1). Diabetes Care. 2014;37(10):2755–2762. | ||
Yki-Järvinen H, Bergenstal R, Ziemen M, et al; EDITION 2 Study Investigators. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using oral agents and basal insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 2). Diabetes Care. 2014;37(12):3235–3243. | ||
Bolli GB, Riddle MC, Bergenstal RM, et al; EDITION 3 study investigators. New insulin glargine 300 U/mL compared with glargine 100 U/mL in insulin-naïve people with type 2 diabetes on oral glucose-lowering drugs: a randomized controlled trial (EDITION 3). Diabetes Obes Metab. 2015;17(4):386–394. | ||
Home PD, Bergenstal RM, Bolli GB, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 1 diabetes: a randomized, Phase 3a, open-label clinical trial (EDITION 4). Diabetes Care. 2015;38(12):2217–2225. | ||
Matsuhisa M, Koyama M, Cheng X, et al; EDITION JP 1 study group. New insulin glargine 300 U/mL versus glargine 100 U/mL in Japanese adults with type 1 diabetes using basal and mealtime insulin: glucose control and hypoglycaemia in a randomized controlled trial (EDITION JP 1). Diabetes Obes Metab. 2016;18(4):375–383. | ||
Terauchi Y, Koyama M, Cheng X, et al. New insulin glargine 300 U/mL versus glargine 100 U/mL in Japanese people with type 2 diabetes using basal insulin and oral antihyperglycaemic drugs: glucose control and hypoglycaemia in a randomized controlled trial (EDITION JP 2). Diabetes Obes Metab. 2016;18(4):366–374. | ||
Jinnouchi H, Koyama M, Amano A, et al. Continuous glucose monitoring during basal-bolus therapy using insulin glargine 300 U mL(−1) and glargine 100 U mL (−1) in Japanese people with type 1 diabetes mellitus: a crossover pilot study. Diabetes Ther. 2015;6(2):143–152. | ||
Riddle MC, Yki-Järvinen H, Bolli GB, et al. One-year sustained glycaemic control and less hypoglycaemia with new insulin glargine 300 U/mL compared with 100 U/mL in people with type 2 diabetes using basal plus meal-time insulin: the EDITION 1 12-month randomized trial, including 6-month extension. Diabetes Obes Metab. 2015;17(9):835–842. | ||
Yki-Järvinen H, Bergenstal RM, Bolli GB, et al. Glycaemic control and hypoglycaemia with new insulin glargine 300 U/mL versus insulin glargine 100 U/mL in people with type 2 diabetes using basal insulin and oral antihyperglycaemic drugs: the EDITION 2 randomized 12-month trial including 6-month extension. Diabetes Obes Metab. 2015;17(12):1142–1149. | ||
Ritzel R, Roussel R, Bolli GB, et al. Patient-level meta-analysis of the EDITION 1, 2 and 3 studies: glycaemic control and hypoglycaemia with new insulin glargine 300 U/mL versus glargine 100 U/mL in people with type 2 diabetes. Diabetes Obes Metab. 2015;17(9):859–867. | ||
Li T, Puhan MA, Vedula SS, Singh S, Dickersin K; Ad Hoc Network Meta-analysis Methods Meeting Working Group. Network meta-analysis-highly attractive but more methodological research is needed. BMC Med. 2011;9:79. | ||
Freemantle N, Chou E, Frois C, et al. Safety and efficacy of insulin glargine 300 u/mL compared with other basal insulin therapies in patients with type 2 diabetes mellitus: a network meta-analysis. BMJ Open. 2016;6(2):e009421. | ||
Martyn-Nemeth P, Schwarz Farabi S, Mihailescu D, Nemeth J, Quinn L. Fear of hypoglycemia in adults with type 1 diabetes: impact of herapeutic advances and strategies for prevention – a review. J Diabetes Complications. 2016;30(1):167–177. | ||
Brod M, Wolden M, Christensen T, Bushnell DM. A nine country study of the burden of non-severe nocturnal hypoglycaemic events on diabetes management and daily function. Diabetes Obes Metab. 2013;15(6):546–557. | ||
Brod M, Christensen T, Bushnell DM. Impact of nocturnal hypoglycemic events on diabetes management, sleep quality, and next-day function: results from a four-country survey. J Med Econ. 2012;15(1):77–86. | ||
Brod M, Wolden M, Christensen T, Bushnell DM. Understanding the economic burden of nonsevere nocturnal hypoglycemic events: impact on work productivity, disease management, and resource utilization. Value Health. 2013;16(8):1140–1149. | ||
Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American diabetes association and the endocrine society. Diabetes Care. 2013;36(5):1384–1395. | ||
International Hypoglycaemia Study Group. Minimizing hypoglycemia in diabetes. Diabetes Care. 2015;38(8):1583–1591. | ||
Heller SR, Cryer PE. Reduced neuroendocrine and symptomatic responses to subsequent hypoglycemia after 1 episode of hypoglycemia in nondiabetic humans. Diabetes. 1991;40(2):223–226. | ||
Boyle PJ, Kempers SF, O’Connor AM, Nagy RJ. Brain glucose uptake and unawareness of hypoglycemia in patients with insulin-dependent diabetes mellitus. N Engl J Med. 1995;333(26):1726–1731. | ||
Amiel SA, Sherwin RS, Simonson DC, Tamborlane WV. Effect of intensive insulin therapy on glycemic thresholds for counterregulatory hormone release. Diabetes. 1988;37(7):901–907. | ||
Boyle PJ, Schwartz NS, Shah SD, Clutter WE, Cryer PE. Plasma glucose concentrations at the onset of hypoglycemic symptoms in patients with poorly controlled diabetes and in nondiabetics. N Engl J Med. 1988;318(23):1487–1492. | ||
Jones TW, Porter P, Sherwin RS, et al. Decreased epinephrine responses to hypoglycemia during sleep. N Engl J Med. 1998;338(23):1657–1662. | ||
Gais S, Born J, Peters A, et al. Hypoglycemia counterregulation during sleep. Sleep. 2003;26(1):55–59. | ||
Schwartz NS, Clutter WE, Shah SD, Cryer PE. Glycemic thresholds for activation of glucose counterregulatory systems are higher than the threshold for symptoms. J Clin Invest. 1987;79(3):777–781. | ||
Mitrakou A, Ryan C, Veneman T, et al. Hierarchy of glycemic thresholds for counterregulatory hormone secretion, symptoms, and cerebral dysfunction. Am J Physiol. 1991;260(1 Pt 1):E67–E74. | ||
Freckmann G, Baumstark A, Jendrike N, et al. System accuracy evaluation of 27 blood glucose monitoring systems according to DIN EN ISO 15197. Diabetes Technol Ther. 2010;12(3):221–231. | ||
King AB, Clark D, Wolfe GS. Contribution of the dawn phenomenon to the fasting and postbreakfast hyperglycemia in type 1 diabetes treated with once-nightly insulin glargine. Endocr Pract. 2012;18(4):558–562. | ||
Riddle MC, Bolli GB, Home PD, et al. Efficacy and safety of flexible versus fixed dosing intervals of insulin glargine 300 U/mL in people with type 2 diabetes. Diabetes Technol Ther. 2016;18(4):252–257. | ||
Becker RH, Nowotny I, Teichert L, Bergmann K, Kapitza C. Low within- and between-day variability in exposure to new insulin glargine 300 U/mL. Diabetes Obes Metab. 2015;17(3):261–267. | ||
Vora J, Cariou B, Evans M, et al. Clinical use of insulin degludec. Diabetes Res Clin Pract. 2015;109(1):19–31. | ||
Caparrotta TM, Evans M. PEGylated insulin Lispro, (LY2605541) – a new basal insulin analogue. Diabetes Obes Metab. 2014;16(5):388–395. | ||
Russell-Jones D, Gall MA, Niemeyer M, Diamant M, Del Prato S. Insulin degludec results in lower rates of nocturnal hypoglycaemia and fasting plasma glucose vs. insulin glargine: a meta-analysis of seven clinical trials. Nutr Metab Cardiovasc Dis. 2015;25(10):898–905. | ||
Lane W, Bailey TS, Gerety G, et al. SWITCH 1: reduced risk of hypoglycaemia with insulin degludec vs insulin glargine U100 in patients with type 1 diabetes: a randomised, double-blind, crossover trial. Diabetologia. 2016;59(Suppl 1):S42–S43. | ||
Carris NW, Taylor JR, Gums JG. Combining a GLP-1 receptor agonist and basal insulin: study evidence and practical considerations. Drugs. 2014;74(18):2141–2152. | ||
Vedtofte L, Knop FK, Vilsbøll T. Fixed combination of insulin and a glucagon-like peptide-1 analog for the treatment of type 2 diabetes, exemplified by insulin degludec and liraglutide. Expert Rev Clin Pharmacol. 2015;8(3):273–282. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

