Back to Journals » Psychology Research and Behavior Management » Volume 11
Influence of oncology nurses’ empathy on lung cancer patients’ cellular immunity
Authors Yang N , Xiao H, Cao Y, Li S, Yan H, Wang Y
Received 19 March 2018
Accepted for publication 18 May 2018
Published 31 July 2018 Volume 2018:11 Pages 279—287
DOI https://doi.org/10.2147/PRBM.S168649
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Igor Elman
Ningxi Yang,1,* Han Xiao,1,* Yingnan Cao,2 Shiyue Li,1,* Hong Yan,1 Yifang Wang3,*
1Department of Epidemiology, School of Health Sciences, Wuhan University, Wuhan, Hubei, China; 2Medical Insurance Office, Beijing Jishuitan Hospital/4th Medical College of Peking University, Xicheng, Beijing, China; 3Department of Medical Humanities, Institute of Medical Humanities, Peking University, Haidian, Beijing, China
*These authors contributed equally to this work
Background: Medical staff’s empathy is closely related to patients’ outcome. This research aimed to verify the influence of Chinese oncology nurses’ empathy on the cellular immunity of lung cancer patients.
Materials and methods: The study included 365 lung cancer patients, who were attended by 30 oncology nurses between October 2016 and May 2017. At the time of admission and discharge, flow cytometric analysis was used to measure the cellular immunity of patients, including T-cell subsets and natural killer (NK)-cell activity. The level of empathy of the oncology nurses was measured by the Jefferson Scale of Empathy (JSE, Chinese version). The nurses were divided into high, moderate, and low empathy groups based on JSE scores. Associations between the empathy shown by nurses and the cellular immunity of patients were examined.
Results: On admission, there was no statistical difference in the cellular immunity of the patients taken care of by the three groups of nurses (P>0.05). At discharge, patients whose nurses were in the high empathy group reported significantly higher B-cell and NK-cell percentages than those whose nurses were in the low empathy group (P<0.001). There was a positive correlation between nurse empathy and percentage of B cells (P=0.003) and NK cells (P<0.001), but no correlation was found between empathy and percentage of CD3+, CD4+, and CD8+ cells. Multiple linear regression analyses indicated that nurse empathy significantly contributed to patient percentage of B cells and NK cells after controlling for patient demographics, disease conditions, and lifestyle.
Conclusion: The effect of oncology nurses’ empathy on cellular immunity was confirmed in lung cancer patients, suggesting empathy education, such as narrative medicine education, should be strengthened to improve patient outcome.
Keywords: empathy, lung cancer, nurse, cellular immunity, narrative medicine
Introduction
Communication is important, especially between medical staff and patients. Empathy, which is an essential component of this relationship, refers to people’s understanding of each other’s positions, feelings, and emotions during interpersonal communication. People who have high empathy levels can imagine themselves in the position of other people and genuinely understand other people after listening to their narrative.1 Currently, narrative medicine has become popular in the field of clinical practice and medical education. Narrative medicine, which was first proposed by Rita Chron in 2001, refers to medicine practiced with narrative competence.2 It is a model for empathy, reflection, profession, and trust that can be applied in clinical practice, especially in the realm of oncology. If the staff respects and understands the patients’ narratives, the staff can respond to the patients’ suffering with empathy and then act on the patients’ narrative.3 If health care provider listens to many patients, then he/she can use their stories to prevent illness by praising positive behaviors.
The focus of medical personnel is caring for sick people. For the patients, being ill is not only a physical event, but it also brings multiple traumas, including traumas of the body, the psyche, the social dimension, and the spiritual dimension. Therefore, patients would benefit from receiving more understanding and comfort. Published reports show that the empathy between doctors and patients in clinical activities can help to improve the doctors’ occupational well-being as well as patients’ satisfaction, compliance, and therapeutic outcome.4–6 Empathy is also very important for establishing good doctor–patient communication.7 Therefore, empathy education starts in medical school. The American Association of Medical Colleges (AAMC) requires all medical schools to offer empathy training courses.8
For oncology nurses, empathy is even more important. Medicine for cancer treatment in China is limited, and many cancer patients cannot be cured. Therefore, patients suffer from more physical and psychological distress. The medical staff’s mission is to provide not only technical intervention but also spiritual salvation. In the daily work of oncology nurses, they provide care and health education for patients. Also, they usually answer patients’ questions. They spend more time with each patient than the doctors. Oncology nurses who are full of empathy can give patients more spiritual care, provide warm companionship, and alleviate their anxiety, thereby enhancing the patient’s quality of life. Recently, empathy has received more attention in oncology. Relationships have been reported between empathy and hematology oncologist’ self-ascribed sense of meaning, psychological adjustment, and cancer patients’ anxiety. 9–11 Additionally, empathy plays a vital role in patients’ participation in radiation therapy safety. 12
The immune system is an important functional system of the body, which bears the functions of immune defense, immune surveillance, and immune stabilization. Malignant tumor growth is often related to immunosuppression, leading to suppression of immune responses in individuals. Thus, the immune function of a human body is highly affected by the occurrence and development of tumors. The cells that play a major role in cellular immunity include T cells, natural killer (NK) cells, and macrophages. The main function of macrophages is to kill cell fragments and pathogens and activate lymphocytes or other immune cells to respond to pathogens. Specific immune responses mediated by T cells play an important role in controlling the growth of immunological tumor cells.13 Further, NK cells can recognize and kill tumor cells efficiently.14
For cancer patients, it is critical to improve immune function, especially after surgery.15,16 Therefore, it is critical to closely monitor their T cells and NK cells. Based on previous studies in psychoneuroimmunology, patients’ mental health affects their immune function.17 Therefore, here we tried to explore a new method to improve the immune function by improving the patient’s mental health through nurses’ empathy.
To the best of our knowledge, although there are some studies reporting the role of physician or nurse empathy in taking care of the patients and several studies concerning psychoneuroimmunology, most of these studies have been conducted in developed countries. At present, there is no research on the relationship between medical staff’s empathy and patients’ immunity. Besides, it is important to conduct the study in China because of the following reasons. First, China is the most populous country in the world and is the largest developing country with increasing international influence. However, there are few studies on clinical medical humanities in China. Such research may benefit more patients and will be used for reference to other developing countries. Second, the health care system in China is different. Although China’s medical reform is continuing to push forward, people are always facing the problem of difficult and expensive medical treatment. If the patient is suffering from cancer, many medical expenses are outside the medical insurance coverage. Chinese cancer patients often face greater psychological and economic pressure. Therefore, they need more emotional comfort from nurses. Third, in developing countries, medical humanities education, such as empathy education, is lacking. The importance of medical humanities and doctor–patient communication has not yet been fully understood. Thus, owing to the imperfect development of patient care systems in developing countries, this exploratory research is necessary in such countries. In light of this situation, we conducted this study. As an evidence-based clinical medical humanities research, this study helps to diversify the sample of clinical empathy research, and sets up a bridge between clinical empathy research and psychoneuroimmunology.
The aim of this study was to study the effect of oncology nurses’ empathy on cellular immunity of lung cancer patients in China. Researchers designed this study to test the following hypothesis: lung cancer patients whose nurses had high empathy scores would have better immunity than patients whose nurses had low empathy scores.
Materials and methods
Participants
The participants were 365 lung cancer patients who were treated between October 2016 and May 2017 and who were cared for by one of the 30 oncology nurses in a cancer hospital in Liaoning Province in China. The patients met the predetermined criteria for eligibility: 1) each patient was diagnosed with lung cancer and had no distant metastasis; 2) each patient was hospitalized and stayed in the hospital for 7–10 days for their operation; 3) each patient knew their diagnosis and were able to provide informed consent and complete all questionnaires with full awareness of their cancer diagnosis; 4) each patient had at least two conversations with her nurse, focusing on the disease, health education, and psychological status. Exclusion criteria were as follows: 1) intake of alcohol or drugs that affect immune function; 2) diagnosis with small-cell lung cancer or metastases as ectopic hormone secretion may impact immune function; and 3) patients who were severely malnourished. Patients who fit the inclusion criteria were selected.
The patients in this study were taken care of by 30 primary oncology nurses. A primary nurse is responsible for the daily care and health education of her patients. Also, primary nurses give comfort to their patients when they are depressed. During the period of hospitalization, the primary nurses undertake the main nursing work of the patients they oversee.
Ethical approval
Participants were assured that there was no risk from participating in the research, and their data would be treated confidentially. All participating patients provided written informed consent. The Wuhan University School of Medicine Ethics Committee approved the study (No 20160928).
Procedures
A correlational study design was used in this research and it followed the following steps. 1) Thirty nurses’ empathy scores were measured. To make statistical results more intuitive, according to the empathy score, they were divided into high-, moderate-, and low-score group, with each group comprising 10 individuals. 2) On the day of admission (T1) and discharge (T2), after explaining the purpose of the study and obtaining the consent of the patients, we asked patients to complete their essential information questionnaires and collected their blood samples in order to assess cellular immunity. 3) After the nurses’ empathy scores were matched to the patients they had taken care of, patients’ immune indices of the three groups of nurses were compared. 4) The correlation between nurses’ empathy and patients’ cell subsets was measured by correlation analysis. 5) In order to further determine the relationship between them, regression analysis was used. Throughout the process, all the nurses’ and patients’ information was kept anonymous and the codes were used instead.
Measures
Lung cancer patients’ essential information
In the questionnaire, we designed the essential information section. This section included sociodemographic information, such as age, sex, marital status, educational background, and monthly family income per capita. Disease condition, including staging, was also included. Lifestyle factors, such as smoking (someone who smoked cigarettes in 30 days, more than 1 cigarette a day, or smoked more than 4 cigarettes a week, but an average of less than 1 cigarette a day) and sleep status in the past 2 weeks, were also included. This section was completed by the patients themselves.
Lung cancer patients’ cellular immunity
To control for diurnal variation, peripheral venous blood samples were collected between 9 am and 10 am before the questionnaires were filled. Patients’ cellular immunity tests were completed by the professional staff working at the clinical laboratory at Anshan Cancer Hospital. They evaluated T-cell subsets including the percentage of total T cells (CD3+), helper T cells (CD4+), cytotoxic T cells (CD8+), NK cells (CD56+), and B cells (CD19+). Flow cytometry was used to assess T- and NK-cell counts with a Cytomics™ FC500 series instrument from Beckman Coulter (Brea, CA, USA). Reagents from BD Bio-Engineering Co., Ltd were used. Cells were fixed in 3% formaldehyde in an isotonic azide-free solution (Beckman Coulter). Labeled antibodies were added at the recommended concentrations and then cells were washed. Cells were cultured in dark, and then excess antibodies were washed out.
Oncology nurses’ empathy
The Chinese version of Jefferson Scale of Empathy (JSE) was used to measure individual differences in empathy of the oncology nurses when the research started. The scale was first constructed in 2001 at Jefferson Medical College to assess empathy in the context of patient care and for medical education.18 Although many scales have been used to measure empathetic abilities, JSE focuses on empathy between medical staff and patients. When measuring doctors, nurses, or medical students’ empathy and patients’ experiences, concerns, and perspectives, the ability to talk about this understanding and a will to help patients is included.19,20 There are 20 items answered on a 7-point Likert scale. Each response is converted to a numerical score ranging from 1 to 7: 1 indicates “Strongly Disagree” and 7 indicates “Strongly Agree”.21 Therefore, scores on the JSE range from 20 to 140, with higher scores indicating stronger empathy levels. There is widespread support for the JSE in many countries, and it has good reliability and validity.22 In this study, we used the Chinese version of the JSE to measure oncology nurses’ empathy. This scale has satisfactory reliability and validity when applied in clinical studies, and it has been widely used in China.23
Statistical analyses
We used the mean and inter-quartile range to describe the concentration and dispersion of nurses’ empathy scores. Empathy among nurses in different groups was compared with the Kruskal–Wallis rank sum test. We used single factor analysis of variance to compare the immune indexes of patients in different nurse groups. We used Spearman correlation analysis to explore the correlations between patients’ immune indexes and nurses’ empathy. We used multiple linear regression to examine the possible confounding effects of patients’ sociodemographic information, disease condition, and lifestyle factors on the relationships between nurses’ empathy scores and patients’ immune indexes. A dummy variable was used when analyzing independent variables. In this study, alpha=0.05 and the tests were two-tailed. We used SPSS version 19.0 for Windows to carry out the processing and analysis of the previously mentioned data.
Results
Sample
In this study, all the selected nurses agreed to participate. They were females with a median age of 30.13±5.11 years. Four hundred twelve patients received our invitation, but 47 patients refused to participate; 365 patients took part in the research with a participation rate of 88.59%. The average age was 55.64±9.35 years. Two hundred ninety-one (79.7%) patients were male and 74 (20.3%) were female. With regard to marital status, 327 (89.6%) patients were married and 38 (10.4%) patients were single or divorced. Concerning educational background, 53 (14.5%) patients received primary education or had no formal schooling, 113 (31.0%) patients graduated from junior middle school, 119 (32.6%) graduated from senior middle school, and 80 (21.9%) patients had college educational background or above. With regard to monthly family income per capita, 22 (6%) patients’ income was less than 3000 yuan, 320 (87.7%) patients’ income was between 3000 yuan and 5000 yuan, and 23 (6.3%) patients were paid more than 5000 yuan. With regard to staging of patients, 141 (38.6%) were at stage I, 158 (43.3%) were at stage II, and 66 (18.1%) were at stage III. Smoking status revealed that 54 (14.8%) were smokers and 311 (85.2%) were not. On evaluation of sleep situation, 58 (15.9%) reported they suffered from insomnia and 307 (84.1%) not.
Nurses’ empathy scores
Empathy scores of the three groups of high-, moderate-, and low-scoring nurses are presented in Table 1. Because nurses’ empathy scores did not coincide with normal distribution, the Kruskal–Wallis test was used to compare empathy scores between the three groups of nurses. The differences of the mean empathy scores for the three groups of nurses were statistically significant (c2=323.771, P<0.001, high scorers > moderate scorers > low scorers).
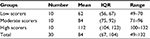  | Table 1 Mean and IQR of the empathy score of 30 participating oncology nurses Notes: χ2=323.771, P<0.001 (high scorers > moderate scorers > low scorers). Abbreviation: IQR, interquartile range. |
Patients’ immune indexes by levels of nurses’ empathy
The immune indexes by levels of nurses’ empathy are given in Table 2. Because the five immune indexes showed normal distribution, single factor analysis of variance was used to compare the patients’ immune indexes among different nurse groups. It showed that on admission, there was no statistical difference in the cellular immunity of the patients taken care of by the three groups of nurses (P>0.05), while at discharge, the percentage of B cells was significantly higher in the patients of nurses with high and moderate empathy scores than in the patients of nurses with low scores (F=14.526, P<0.001). Similar with this finding, the percentage of NK cells was significantly higher in the patients of nurses with high empathy scores than in the patients of nurses with low scores (F=282.292, P<0.001).
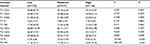  | Table 2 Comparison of patients’ immune indexes among different nurse groups at admission (T1) and at discharge (T2) Abbreviation: NK, natural killer. |
The correlations between patients’ immune indexes and nurses’ empathy
The correlations between patients’ immune indexes and nurses’ empathy are given in Table 3. Nurses’ empathy scores were in positive correlation to patients’ B-cell percentage (P=0.003) and NK-cell percentage significantly (P<0.001).
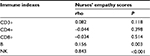  | Table 3 Spearman’s correlation between empathy and cell subsets (%) Abbreviation: NK, natural killer. |
Regression analyses of factors that affect patients’ immune indexes
Multiple linear regression was used to examine the unique effect of nurses’ empathy on patients’ immune indexes after controlling for patients’ demographic and clinical characteristics. When controlling for other variables, a one-point increase on the primary nurse’s empathy score led the patient’s B-cell percentage to increase by 0.025 points (P=0.01). Also, a one-point increase on the primary nurse’s empathy score led the patient’s NK-cell percentage to increase by 0.242 points (P<0.001). This finding showed that the nurses’ empathy was significantly associated with the patients’ B-cell percentage and NK-cell percentage. The results of the regression analysis are summarized in Table 4.
  | Table 4 Multivariate regression analysis of factors affecting patients’ immunity Abbreviation: NK, natural killer. |
Discussion
This research confirmed that patients whose oncology nurses had high empathy scores had more percentage of B cells and NK cells. The effect of nurses’ empathy on their patients’ cellular immunity was the emphasis of this research. We found close associations between nurses’ empathy and lung cancer patients’ cellular immunity. Previous studies found that medical staff/clinican’s empathy was related to patient’s outcomes, including increasing satisfaction and psychological well-being,24 reducing patients’ anxiety before a bronchoscopy,25 reducing distress,26 and improving self-efficacy of patients with HIV.27 Empathy also has an impact on the patients’ physiological parameters. For example, Hojat et al confirmed physicians’ empathy was associated with diabetic patients’ hemoglobin A1c and LDL-C, and Canale et al found empathy helps diabetic patients reduce incidence of acute metabolic complications.28,29 Mack et al reported cancer patients showed better functional status if they felt more empathy from oncologists.30 Through Smith et al’s intervention study, it was confirmed that doctor–patient empathy and communication quality was related to breast cancer patients’ pain management.31
This study provided new knowledge in the field of psychosocial oncology by revealing that nurses’ empathy and patients’ immunity are related. This is because the empathy of nurses affects the patients’ immune system by influencing their psychology. Many cancer patients suffer from negative emotions such as anxiety, depression, and psychological distress caused by various reasons.32–34 These negative emotions are activated by the hypothalamic–pituitary–adrenal axis and the autonomic nervous system, which in turn leads to the secretion of large amounts of adrenal glucocorticoids and catecholamines. These substances lead to immune-reduced surveillance.35
When it comes to the impact of nurses’ empathy on patients’ psychology, several factors must be taken into consideration. First, regarding empathy, patients can feel devotion and support. With adequate communication, patients trust staff more and have better self-management and treatment compliance.36 Additionally, medical providers can better explore patients’ symptoms and needs as well as provide a better diagnosis and individualized treatment regimens, which are good for patients’ bodies and mental health.37 Second, empathy is the process of medical staff listening to and understanding the patient narrative. Patients reveal their concerns and worries when telling their stories and experiences.38 Having the ability to empathize helps staff identify patients’ concerns quickly. Then, the staff can support and comfort the patients better and provide proper individual health education and psychological intervention. These actions will improve patients’ mental health. More importantly, telling the story to their doctors and nurse also relieves psychological distress and releases pressure. Third, if the nurse has high empathy level, in the nurse–patient communication, the patient’s view of life and death, suffering, and health care can be reshaped. So, they will be more open-minded on their illness. Also, the nurses can help patients understand medicine, know the limitations of medicine, and then have a more rational expectation of their treatment, which is good for their mental health. Fourth, empathy promotes patient-centered care.39 In the narrative of the patient, the doctor takes the patient as the center, and the patient perceives the clinician as a helping member of a social support system so that the patient’s psychological burden is lighter.40 Further, empathy is the basis for shared decision-making. In shared decision-making, patients think that their feelings and suggestions receive more attention, which encourages them and makes them feel more dignified. In empathy and shared decision-making, patients take an active role in caring for their own health.41,42 Since empathy affects the patients’ psychology and view in these areas, and psychology affects immunity, this study provided a preliminary conclusion in the relationship between oncology primary nurses’ empathy and lung cancer patients’ immunity.
Another finding of this study was that the empathetic ability of Chinese nurses was lower than that reported in literature for other countries. This is because nurses’ function in China is somewhat different from the ones in other developed countries. In China, nurses often are overworked and have a lot of psychological pressure. Although based on relevant regulations, the proportion of beds to nurses in a general hospital should not be less than 1:0.4, and nurses have to take care of more number of patients. Further, their division of labor is not clear. Considering that they are already overworked, they lack the time to communicate with patients. Because the workload is huge, they focus on physical therapy rather than psychological, social, and spiritual care. On the contrary, in the USA or other developed countries, nurse function is multivariate. They provide physical, psychosocial, and spiritual support for patients; they participate in their patient’s health education and communicate well with them. They even spend time with their patients, just to accompany them. These are great benefits to patients.
Since empathy has a positive impact on patients’ outcome, psychological and social needs have been met. This finding suggests that empathy should constitute an important part of medical personnel’s competency and can be enhanced through training.43,44 Narrative medicine education and other educational interventions are advised to carry out in order to improve medical professionals’ empathy abilities.
Also, these findings have implications for clinical practice. Oncology nurses should improve their ability to empathize. Additionally, our findings suggest that narrative medicine based on empathy may have beneficial effects; this hypothesis should be tested in future research. The medical staff in oncology should listen to patients’ personalized narratives and show empathy toward them, especially when doing health education. In this way, patients can get more humane care and treatment.45
However, there are limitations of our present study. First, there are many factors affecting the patients’ cellular immunity, including disease progression, individual constitution, sport, diet, and other factors. In the present study, we incorporated limited factors. Clearly, it is difficult and unpractical to control for all these factors in a study. We can only control a certain number of the factors. Second, in the selection of the object, the sample size was small because participants were sampled from only one hospital. Third, this was a cross-sectional study that only reflected nurses’ empathy level and patients’ cellular immunity at a single timepoint. Therefore, it has a certain contingency; long-term intervention studies and cohort studies need to be conducted in the future.
Conclusion
In summary, this study showed that oncology nurses’ empathy was an important factor for the cellular immunity of lung cancer patients. The nurses’ empathy helped patients to have better immunity. Empathy education, such as narrative medicine, needs to strengthen in order to improve patients’ outcome.
Acknowledgments
The authors thank all the patients, who generously attended the study at such a rough time in their lives, and all of the nurses who participated in the study. This study received financial support for the research, authorship, and/or publication of this article from School of Health Sciences, Wuhan University, Wuhan, Hubei, China. Ningxi Yang and Han Xiao are co-first authors for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Kataoka HU, Koide N, Ochi K, Hojat M, Gonnella JS. Measurement of empathy among Japanese medical students: psychometrics and score differences by gender and level of medical education. Acad Med. 2009;84(9):1192–1197. | ||
Charon R. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA. 2001;286(15):1897–1902. | ||
Charon R. Narrative Medicine: Honoring the Stories of Illness. New York: Oxford University Press; 2006: 218–225. | ||
Williams B, Lau R, Thornton E, Olney LS. The relationship between empathy and burnout – lessons for paramedics: a scoping review. Psychol Res Behav Manag. 2017;10:329–337. | ||
Lipp MJ, Riolo C, Riolo M, Farkas J, Liu T, Cisneros GJ. Showing you care: an empathetic approach to doctor–patient communication. Semin Othod. 2016; 22(2):88–94. | ||
Lelorain S, Brédart A, Dolbeault S, Sultan S. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psychooncology. 2012;21(12):1225–1264. | ||
Larso EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. JAMA. 2005;293(9):1100–1106. | ||
Hojat M, Gonnella JS, Mangione S. Empathy in medical students as related to academic performance,clinical competence and gender. Med Educ. 2002;36(6):522–527. | ||
Komisar J, Mcfarland DC. Is empathy associated with a self-ascribed sense of meaning among resident physicians working with patients nearing the end of life on a hematology-oncology ward? Psychooncology. 2016;26(9):1403–1406. | ||
Labay LE, Walco GA. Brief report: empathy and psychological adjustment in siblings of children with cancer. J Pediatr Psychol. 2004; 29(4):309–314. | ||
Zwingmann J, Baile WF, Schmier JW, Bernhard J, Keller M. Effects of patient-centered communication on anxiety, negative affect, and trust in the physician in delivering a cancer diagnosis: a randomized, experimental study. Cancer. 2017; 123(16):3167–3175. | ||
Bibault JE, Pernet A, Mollo V, Gourdon L, Martin O, Giraud P. Empowering patients for radiation therapy safety: results of the EMPATHY study. Cancer Radiother. 2016;20(8):790–793. | ||
Bethune MT, Joglekar AV. Personalized T cell-mediated cancer immunotherapy: progress and challenges. Curr Opin Biotechnol. 2017;48:142–152. | ||
Granzin M, Wagner J, Köhl U, Cerwenka A, Huppert V, Ullrich E. Shaping of natural killer cell antitumor activity by ex vivo cultivation. Front Immunol. 2017;8:458. | ||
Cata JP, Bauer M, Sokari T, et al. Effects of surgery, general anesthesia, and perioperative epidural analgesia on the immune function of patients with non-small cell lung cancer. J Clin Anesth. 2013;25(4):255–262. | ||
Kruijsen-Jaarsma M, Révész D, Bierings MB, Buffart LM, Takken T. Effects of exercise on immune function in patients with cancer: a systematic review. Exerc Immunol Rev. 2013;19:120–143. | ||
Fagundes CP, Lindgren ME, Kiecolt-Glaser JK. Carr B and Steel J, editors. Psychoneuroimmunology and cancer: incidence, progression, and quality of life. In: Psychological Aspects of Cancer. New York: Springer US; 2013:1–11. | ||
Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61(2):349–365. | ||
Hojat M. Ten approaches for enhancing empathy in health and human services cultures. J Health Hum Serv Admin. 2009;31(4):412–450. | ||
Hojat M, Gonnella JS. What matters more about the Interpersonal Reactivity Index and the Jefferson Scale of Empathy? Their underlying constructs or their relationships with pertinent measures of clinical competence and patient outcomes? Acad Med. 2016;92(6):743–745. | ||
Hojat M. Empathy in Patient Care: Antecedents, Development, Measurement, and Outcomes. New York: Springer; 2007:12–20. | ||
Costa P, de Carvalho-Filho MA, Schweller M, et al. Measuring medical students’ empathy: exploring the underlying constructs of and associations between two widely used self-report instruments in five countries. Acad Med. 2017; 92(6):860–867. | ||
Wen D, Ma X, Li H, Xian B. Empathy in Chinese physicians: preliminary psychometrics of the Jefferson Scale of Physician Empathy (JSPE). Med Teach. 2013; 35(7):609–610. | ||
Lelorain S, Brédart A, Dolbeault S, Sultan S. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psychooncology. 2012;21(12):1255–1264. | ||
Choi SM, Lee J, Park YS, Lee CH, Lee SM, Yim JJ. Effect of verbal empathy and touch on anxiety relief in patients undergoing flexible bronchoscopy: can empathy reduce patients’ anxiety? Respiration. 2016;92(6):380–388. | ||
Olson JK. Relationships between nurse-expressed empathy, patient-perceived empathy and patient distress. Image J Nurs Sch. 1995;27(4):317–322. | ||
Flickinger TE, Saha S, Roter D, et al. Clinician empathy is associated with differences in patient-clinician communication behaviors and higher medication self-efficacy in HIV care. Patient Educ Couns. 2015;99(2):220–226. | ||
Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011; 86(3):359–364. | ||
Canale S, Louis D, Maio V, et al. The relationship between physician empathy and disease complications. Acad Med. 2012; 87(9):1243–1249. | ||
Mack JW, Block SD, Nilsson M, et al. Measuring therapeutic alliance between oncologists and patients with advanced cancer: the Human Connection Scale. Cancer. 2009;115(14):3302–3311. | ||
Smith MY, DuHamel KN, Egert J, Winkel G. Impact of a brief intervention on patient communication and barriers to pain management: results from a randomized controlled trial. Patient Educ Couns. 2010;81(1):79–86. | ||
Sharp L, Carsin AE, Timmons A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psychooncology. 2013;22(3):745–755. | ||
Cho J, Choi EK, Kim SY, et al. Association between cancer stigma and depression among cancer survivors: a nationwide survey in Korea. Psychooncology. 2013;22(10):2372–2378. | ||
Bao Y, Li L, Guan Y, et al. Prevalence and associated positive psychological variables of anxiety and depression among patients with central nervous system tumors in China: a cross-sectional study. Psychooncology. 2017;26(2):262–269. | ||
Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci. 2008;31(9):464–468. | ||
Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237–251. | ||
Ernstmann N, Weissbach L, Herden J, Herden J, Winter N, Ansmann L. Patient-physician communication and health-related quality of life of patients with localised prostate cancer undergoing radical prostatectomy_a longitudinal multilevel analysis. BJU Int. 2016;119(3):396–405. | ||
Maguire P, Faulkner A, Booth K, Elliott C, Hillier V. Helping cancer patients disclose their concerns. Eur J Cancer. 1996;32A(1):76–81. | ||
Thompson C, Barforoshi S, Kell C, Banerjee D. Uncovering the patient experience: empathy mapping promotes patient-centered care for improved heart failure patient outcomes. J Card Fail. 2016;22(8):S87–S88. | ||
Hojat M. Empathy and Patient Outcomes. Heidelberg: Springer International Publishing; 2016:1–10. | ||
Ruberton PM, Huynh HP, Miller TA, Kruse E, Chancellor J, Lyubomirsky S. The relationship between physician humility, physician-patient communication,and patient health. Patient Educ Couns. 2016;99(7):1138–1145. | ||
Roberts CS, Cox CE, Reintgen DS, Baile WF, Gibertini M. Influence of physician communication on newly diagnosed breast patients’ psychologic adjustment and decision-making. Cancer. 1994;74(1 Suppl):336–341. | ||
Casas RS, Xuan Z, Jackson AH, Stanfield LE, Harvey NC, Chen DC. Associations of medical student empathy with clinical competence. Patient Educ Couns. 2017;100(4):742–747. | ||
Delvaux N, Merckaert I, Marchal S, et al. Physicians’ communication with a cancer patient and a relative: a randomized study assessing the efficacy of consolidation workshops. Cancer. 2005;103(11):2397–2411. | ||
Cobos B, Haskard-Zolnierek K, Howard K. White coat hypertension: improving the patient-health care practitioner relationship. Psychol Res Behav Manag. 2015;8:133–141. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
