Back to Journals » Drug, Healthcare and Patient Safety » Volume 14
Influence of Medical Education on Medicine Use and Self-Medication Among Medical Students: A Cross-Sectional Study from Kabul
Authors Daanish AF, Mushkani EA
Received 9 February 2022
Accepted for publication 18 May 2022
Published 23 May 2022 Volume 2022:14 Pages 79—85
DOI https://doi.org/10.2147/DHPS.S360072
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hemalkumar B Mehta
Ahmad Farid Daanish, Ershad Ahmad Mushkani
Department of Pharmacology, Kabul University of Medical Sciences, Kabul, Afghanistan
Correspondence: Ershad Ahmad Mushkani, Department of Pharmacology, Kabul University of Medical Sciences, Kabul, Afghanistan, Tel +93-74460022, Email [email protected]
Objective: To compare the prevalence of self-medication among first- and fifth-year medical students at Kabul University of Medical Sciences.
Methods: A cross-sectional study was conducted with the participation of all first- and fifth-year medical students by using a short, self-administered questionnaire. The prevalence of self-medication was estimated in the entire study population and also in those who had used medicines in the preceding one week.
Results: Of the total 302 students, the prevalence of medicine use was 38%. The prevalence of self-medication in all study population was 25.16%, whereas in those who had used medicines was 64.9%. Prescription-only medicines consisted of 59.2% of self-medication. The practice of self-medication and the use of prescription-only medicines were more prevalent among students in their fifth year and among males. While the prevalence of medicine use was the same among males and females, it differed between students in the fifth and first year. Paracetamol, anti-infectives, and non-steroidal anti-inflammatory drugs (NSAIDs) were more frequently used medicines.
Conclusion: The use of medicines, self-medication and the use of prescription-only medicines were more prevalent among fifth-year students compared to those in the first-year. This apparently reflects the effect of medical education and training. More specific studies are required to address the issue in more detail and to facilitate interventions. The estimation of the prevalence of self-medication by using a short acceptable recall period, confined in those who had used medicines, seems to be more reasonable and accurate than by using a longer recall period in the entire study population. The prevalence of prescription-only medicines in self-medication could also be a useful indicator.
Keywords: self-medication, medical students, medicine use, prescription-only medicines
Introduction
Self-medication (SM) is such a broad subject in the health sector that even one of its subcategories, ie, SM among medical students, has been the subject of numerous studies.1–5 However, these studies have been carried out by different methods, study populations and recall periods, leading to disparate results.
Although SM is quite unambiguous term, it has been defined as the use of medication to treat oneself without getting any medical supervision6 or as the choosing and utilization of medicines to treat self-recognized diseases or symptoms by oneself.7
Allocating some medicines under the category of over-the-counter (OTC) medicines implies that they are to be used in SM. OTC medicine is a medicine “that can be purchased direct from the attendant at the counter of a pharmacy, chemist’s shop, or drugstore without a physician’s prescription”.8 SM as an element of self-care,7 that has been integrated into many health care systems in the world, has some social and economic benefits, but also has several risks.9 If SM with OTC items is practiced appropriately, it may have economic advantages not only to patients but also to employers and healthcare systems.10 On the other hand, it seems that SM is associated with some disadvantages like misdiagnosis, under- or over-dosage, shorter or longer course of treatment, microbial resistance (in case of antibiotics), drug interactions and use in a contraindicated condition. These disadvantages may be more common if Prescription-Only Medicines (POMs) are used in SM.
Divergent results about the prevalence of SM in medical students have been reported: 99%3 and 97.2% in six months,11 49.3%12 and 57.05% in one month;13 and 44.8% in unspecified period.14 No definite period for the calculation of SM prevalence was found. The difference in SM prevalence reported by the above-mentioned studies is probably due to different recall periods and methods.
Most of the studies that focused on the prevalence of SM in medical students, comprised indiscriminately all students. The comparison of SM prevalence among different years has been examined by a few studies, eg, Banerjee et al13 showed that 79.31% of final-year students practiced more SM compared to 41.67% of first-year students and James, H.et al.14 reported that students of Year 4 practiced SM more often than students of Year 2 (73.3% versus 52.6%).
Despite the availability of several studies about the prevalence of SM, data about the prevalence of SM out of total medicines used are scarce worldwide; see, for example, the study done by Bertoldi et al15 in which they have calculated SM prevalence in those who have used medicines. The SM of POMs that has been reported to be widespread9 is an issue that needs attention since it is more prone to be hazardous. Not all studies made a distinction between SM of OTC and POMs. SM may comprise OTC medications and POMs. Limited studies examined the ratio of these two components of SM in medical students. Albusalih et al reported that in nearly half of SM cases either POMs alone or both OTC and POMs were used.12 In a study in India, around two-third of SM were of non-prescription type.16
If the prevalence is being merely determined by students’ opinions about SM; or during a long recall period; it may be prone to biases.
The undefined prevalence of SM, ie, without specifying the period, without identifying OTC and POMs, and/or without clear differentiation between general and medicine users’ group-specific prevalence, will not be a practically useful indicator.
Most of the above-mentioned issues are considered in this article, and for the first time, various aspects of medicine use (MU) and SM among medical students at Kabul University of Medical Sciences (KUMS) have been simultaneously studied.
Objective
To compare the prevalence of SM among first- and fifth-year medical students at KUMS.
Method
Study Population
A cross-sectional study was carried out at KUMS, the largest medical university in Afghanistan.
All first- (N = 142) and fifth-year (N = 190) students of the faculty of medicine, KUMS, who completed the questionnaires were included in the study. Students who were absent on the day of data collection, as well as students who returned incomplete questionnaires were excluded.
Study Tool: The Questionnaires
A short self-administered questionnaire including open-ended and close-ended items was designed in which students were asked whether they had taken any medicine within the past week. In case of affirmative, they were asked to specify who advised them to take the medicine (doctor, attendant at the pharmacy, nurse, classmate, others or themselves), and the names of medicines that they had used. Finally, they were asked to write down the names of medicines that they had used. Except for year of education and sex, the socioeconomic and demographic information was excluded, as these were not supposed to be studied. To reduce recall bias, the recall period was confined to one previous week.
The five studied variables were sex (to compare the results between sex), years of medical education (to see the impact of five-year medical education on SM and its characteristic), use of any medication (to describe the prevalence of medicine use), names of the medicines used (to see if they were OTC or POMs and to determine the frequency of use of different classes of medicines), and the person who advised them to take (to identify SM).
The students were approached at the end of their scheduled course classes, and after a short explanation about the study, questionnaires were handed out. The questionnaire was anonymous, and it was designed to take not more than ten minutes. Both classes, first, and fifth, were approached separately, on the same day.
Analysis
To calculate the prevalence of MU and the general prevalence of SM, the total number of studied students was used as the denominator. Group-specific SM prevalence was also calculated in students who had used any medicine; in which the denominator was the number of students who had used any medicine during the one-week recall period. Finally, POMs use prevalence was calculated in those who practiced SM. The reported medicine names were checked with the OTC list of National Licensed Medicine List of Afghanistan. Since all students who completed the questionnaires were included in the study, only descriptive statistics were used.
Ethical Issues
This is a non-interventional study. The participation was not mandatory. Unanimous questionnaires were used to preserve confidentiality. The study was carried out by Pharmacology Department staff who did not teach in both classes. The researcher orally disclosed that the participation was voluntary, and this was regarded as oral consent. The questionnaire was anonymous and was designed to be filled within about ten minutes. Approval from Research Committee KUMS (Reference: 21/46-21/1/1401) was obtained.
Results
Of 332 students, 312 (93.9%) questionnaires were collected. Ten incomplete or illegible questionnaires were excluded and finally, 302 questionnaires (90.9%) were included in the study.
The prevalence of MU in all studied students was 38%, and general SM prevalence was 25.16% in the preceding one week. Medicine users’ group-specific prevalence of SM was 64.9%, which is higher than the general prevalence. Among those that practiced SM, 45 (59.2%) used POMs. The prevalence of medication use, SM and POMs in SM was higher in the fifth-year students compared to the first-year students (Table 1).
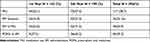 |
Table 1 Prevalence of Medicine Use and Self-Medication |
The prevalence of MU was found to be the same among males and females, while males practiced more SM and used more POMs than females (Table 2). Students of fifth-year practiced more SM than did the first-year students.
 |
Table 2 MU, SM and POMs in SM According to Gender |
Among those who did not practice SM, most of the fifth-year students used medicines advised by doctors, while most of the first-year students used medicines advised by others (Table 3).
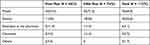 |
Table 3 The Person Who Advised Students to Take the Medicine |
In total, 103 item medicines were used, among which Paracetamol 26.2% followed by anti-infectives 21.3% and NSAIDs 10.6% were most frequently self-medicated medicines/medicine groups in the previous week. Among anti-infectives, the most common practiced group as SM was antibacterials. Anti-infectives and Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) were more used medicines by fifth-year students compared to first-year, but combined analgesics were more used by first-year students (Table 4).
 |
Table 4 Self-Medicated Medicines/Medicine Groups According to Year of Education |
Discussion
Because of differences in how SM prevalence is calculated (all studied students vs those that used medicines) and dissimilarities of recall periods, it seems to be difficult to compare the findings of this study with others. The general SM prevalence found in this study (25.16%) is lower compared to that reported by others that varied from 44.8%14 to 99%3,14 but the prevalence of SM in medicine users’ specific group was found to be 64.9%.
Practicing SM is unknown among those who did not use any medication; consequently, general SM prevalence estimation based on the entire population study would be dubious. The normal range of SM prevalence cannot be determined but could be evaluated by considering other factors like the literacy and health knowledge of the study population.
SM prevalence may increase by increasing the recall period, since the lifetime prevalence of SM, is most probably near 100% in the adult population. Furthermore, if recall period is increased, recall bias would be more probable. The differences in recall period are apparent in other studies.11–14 In this study, the recall period was limited to one week.
The prevalence of medication use was found to be the same in males and females, which is similar to findings from Karachi in which they did not find difference between the self-medication practices of males and females.17 But it contradicts other findings showing more females used medicines than males,18–20 and also contradicts findings of studies that reported more females practicing SM.3,13,21
The use of POMs in SM has special importance since disadvantages may be more common if POMs are used in SM. Among those that practiced SM, 45 (59.2%) used POMs. Although there are ample studies about single specific POMs SM, like SM of antibiotics,22,23 the prevalence of SM of all POMs vs OTC has rarely been studied, except a few studies like that of Shehnaz et al24 and Kanwal et al,3 who reported that OTC was the most commonly used medicines in those who practiced SM. The use of POMs in SM was more prevalent in the fifth-year compared to first-year, which may be because of more drug information gathered during five years of medical training. Males used more POMs in SM than females. The use of POMs in SM has to be studied in more detail in the future.
The study reveals that final-year students more frequently practiced SM compared to first-year students, this finding is in accordance with other studies that showed an increase in SM according to years of medical study.14,16,21,25 But it contradicts finding from Karachi in which they did not find difference between the self-medication practices and the year of study.17
In total, 103 item medicines were self-medicated by 76 students. Paracetamol 26.2% (N = 27) followed by anti-infective 21.3% (N = 22) and NSAIDs 10.6% (N = 11) were the most frequently self-medicated medicines/medicine groups. Anti-infectives were used more than that found by Albusalih et al,12 ie,16.59% but less than that reported by others.1,13,21,22,24,25 Paracetamol/NSAIDs were used less than that reported in other studies, ie, NSAID 74.3%,3 antipyretic analgesic 80.6%16 and 79.6%.25 Vitamins were used less than that found by Albusalih, ie, 30.5%.12 Fifth-year students used more anti-infectives and NSAIDs compared to first-year, but first-year students used more combined analgesics.
Strength of the study: The prevalence of SM is estimated not only in the entire study population but also in those who used medicines. The analysis was based on the name of drugs that the respondents had used, not merely on their opinions and answers about the practice of SM. The prevalence of POMs in SM was also calculated. The questionnaires were filled by both classes on the same day. The response rate (93.9%) was quite high that even after the exclusion of ten incomplete or illegible questionnaires, 90.9% of questionnaires were included in the study. It was a cross-sectional study that included all first- and fifth-year medical students at KUMS, who completed the questionnaires. And finally, a short recall period that would reduce recall bias is among the distinctiveness of this study.
Weakness: It cannot be understood from the study whether medications were rationally used. This study cannot be generalized neither to the general population nor to other fields’ students. The dosage forms were not reported by participants, which may be due to the lack of specific question in this regard in the questionnaire.
Conclusion
The use of medicines, self-medication and the use of prescription-only medicines were more prevalent among fifth-year students compared to those in the first-year. This apparently reflects the effect of medical education and training. More specific studies are required, to address the issue in more detail and to facilitate interventions. The estimation of the prevalence of self-medication by using a short acceptable recall period, confined in those who had used medicines, seems to be more reasonable and accurate than by using a longer recall period in the entire study population. The prevalence of prescription-only medicines in self-medication could also be a useful indicator.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Alshahrani SM, Alavudeen SS, Alakhali KM, Al-Worafi YM, Bahamdan AK, Vigneshwaran E. Self-medication among King Khalid University Students, Saudi Arabia. Risk Management Healthcare Policy. 2019;12:243. doi:10.2147/RMHP.S230257
2. Malik IJ, Bhatti AA, Din AT, et al. Assessment of knowledge, attitude, and practices regarding self-medication for acne among medical students. Cureus. 2019;11:8.
3. Kanwal ZG, Fatima N, Azhar S, Chohan O, Jabeen M, Yameen MA. Implications of self-medication among medical students – a dilemma. J Pak Med Assoc. 2018;68(9):1363–1367.
4. Helal RM, Abou-ElWafa HS. Self-medication in university students from the city of Mansoura, Egypt. J Environ Public Health. 2017;2017:1–7. doi:10.1155/2017/9145193
5. Hu Y, Wang X, Tucker JD, et al. Knowledge, attitude, and practice with respect to antibiotic use among Chinese medical students: a multicentre cross-sectional study. Int J Environ Res Public Health. 2018;15(6):1165. doi:10.3390/ijerph15061165
6. Barber K, Ed. The Canadian Oxford Dictionary.
7. World Health Organization. The Role of the Pharmacist in Self-Care and Self-Medication: Report of the 4th WHO Consultative Group on the Role of the Pharmacist, the Hague, the Netherlands, 26-28 August 1998 (No. WHO/DAP/98.13). World Health Organization; 1998.
8. Porta M. A Dictionary of Public Health. Oxford University Press; 2018.
9. Home WH. The benefits and risks of self-medication. WHO Drug Information. 2000;14(1):548.
10. Noone J, Blanchette CM. The value of self-medication: summary of existing evidence. J Med Econ. 2018;21(2):201–211. doi:10.1080/13696998.2017.1390473
11. Alshogran OY, Alzoubi KH, Khabour OF, Farah S. Patterns of self-medication among medical and nonmedical University students in Jordan. <![CDATA[Risk Management and Healthcare Policy]]>. 2018;11:169. doi:10.2147/RMHP.S170181
12. Albusalih FA, Naqvi AA, Ahmad R, Ahmad N. Prevalence of self-medication among students of pharmacy and medicine colleges of a public sector university in Dammam City, Saudi Arabia. Pharmacy. 2017;5(4):51. doi:10.3390/pharmacy5030051
13. Banerjee I, Bhadury T. Self-medication practice among undergraduate medical students in a tertiary care medical college, West Bengal. J Postgrad Med. 2012;58(2):127. doi:10.4103/0022-3859.97175
14. James H, Handu SS, Khaja KA, Sequeira RP. Influence of medical training on self-medication by students. Int. Journal of Clinical Pharmacology and Therapeutics. 2008;46(1):23–29. doi:10.5414/CPP46023
15. Bertoldi AD, Silveira MP, Menezes AMB, Assunção MC, Gonçalves H, Hallal PC. Tracking of medicine use and self-medication from infancy to adolescence: 1993 Pelotas (Brazil) birth cohort study. J Adolescent Health. 2012;51(6):S11–5. doi:10.1016/j.jadohealth.2012.06.027
16. Kasulkar AA, Gupta M. Self medication practices among medical students of a private institute. Indian J Pharm Sci. 2015;77(2):178. doi:10.4103/0250-474X.156569
17. Zafar SN, Syed R, Waqar S, et al. Self-medication amongst university students of Karachi: prevalence, knowledge and attitudes. JPMA. The Journal of the Pakistan Medical Association. 2008;58(4):214.
18. Moraes ACFD, Delaporte TRM, Molena-Fernandes CA, Falcão MC. Factors associated with medicine use and self medication are different in adolescents. Clinics. 2011;66(7):1149–1155. doi:10.1590/S1807-59322011000700005
19. Arrais PSD, Brito LL, Barreto ML, Coelho HL. Prevalência e fatores determinantes do consumo de medicamentos no Município de Fortaleza, Ceará, Brasil. Cadernos de saúde pública. 2005;21(6):1737–1746. doi:10.1590/S0102-311X2005000600021
20. Loikas D, Wettermark B, von Euler M, Bergman U, Schenck-Gustafsson K. Differences in drug utilisation between men and women: a cross-sectional analysis of all dispensed drugs in Sweden. BMJ open. 2013;3(5):e002378. doi:10.1136/bmjopen-2012-002378
21. Osemene KP, Lamikanra A. A study of the prevalence of self-medication practice among university students in Southwestern Nigeria. Tropical J Pharmaceutical Res. 2012;11(4):683–689. doi:10.4314/tjpr.v11i4.21
22. Sarahroodi S, Arzi A, Sawalha AF, Ashtarinezhad A. Antibiotics self-medication among southern Iranian university students. Int J Pharmacol. 2009;6(1):48–52. doi:10.3923/ijp.2010.48.52
23. Suaifan GA, Shehadeh M, Darwish DA, Al-Ijel H, Yousef AM, Darwish RM. A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in Jordan. Afr J Pharm Pharmacol. 2012;6(10):763.
24. Shehnaz SI, Khan N, Sreedharan J, Issa KJ, Arifulla M. Self-medication and related health complaints among expatriate high school students in the United Arab Emirates. Pharmacy Practice (Internet). 2013;11(4):211. doi:10.4321/S1886-36552013000400006
25. Prabhakaran S, P.p V, Koppad R, Acharya A. A cross-sectional study on self medication pattern among medical students at Kannur, North Kerala. J Evol Med Dent Sci. 2013;2(45):8693–8700. doi:10.14260/jemds/1509
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
