Back to Journals » Research and Reports in Urology » Volume 12
Infiltrating Treg and Th17 Cells of the Prostate Hypertrophy Gland Associated with Propionibacterium Acnes Infection
Authors Radej S, Płaza P, Olender A, Szewc M , Bar K, Maciejewski R
Received 29 September 2020
Accepted for publication 9 November 2020
Published 30 November 2020 Volume 2020:12 Pages 593—597
DOI https://doi.org/10.2147/RRU.S284066
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Sebastian Radej,1 Paweł Płaza,2 Alina Olender,3 Monika Szewc,1 Krzysztof Bar,2 Ryszard Maciejewski1
1Department of Normal Anatomy, Medical University of Lublin, Lublin, Poland; 2Urology and Urological Oncology, Medical University of Lublin, Lublin, Poland; 3Chair and Department of Medical Microbiology, Medical University of Lublin, Lublin, Poland
Correspondence: Sebastian Radej
Department of Normal Anatomy, Medical University of Lublin, Jaczewskiego 4, 20-090, Lublin, Poland
Tel/Fax +4881448 6020
Email [email protected]
Purpose: The aim of the study was to evaluate prostate cell infiltration by CD4(+)IL-17(+) and Treg cells in BPH and PCa patients depending on P. acnes infection in the prostate gland.
Patients and Methods: Prostate fragments were collected from 54 patients with PCa and 34 patients with BPH. Rapid ID 32 was used to identify the bacteria. Cells were analyzed by flow cytometry BD FACSCanto II. Statistical analysis was performed using Statistica 7 software (TIBCO Software Inc, USA).
Results: P. acnes was detected in 35% of patients with PCa and 41% of individuals with BPH. The infiltration of CD4(+)IL-17(+) and Treg cells was statistically significantly higher (P = 0.001) in patients with BPH and positive for P. acnes. A statistically considerably higher (P = 0.001) infiltration of Treg cells in treated for PCa with P.acnes infection was also demonstrated.
Conclusion: Prostatitis caused by P. acnes may contribute to the development of BPH and PCa.
Keywords: P. acnes, Treg cells, Th17 cells, benign prostatic hyperplasia, prostate cancer
Introduction
The etiology and pathogenesis of benign prostatic hyperplasia (BPH) and prostate cancer (PCa) have not been fully understood so far. Currently, it indicates that prostate chronic inflammation plays a significant role in the development of both diseases. Bacterial infections are among the potential sources of prostatitis.1,2 Propionibacterium acnes (P. acnes) is a common cause of acne vulgaris and also one of the causes of implant-associated infections.3,4 As recent research shows, P. acnes is isolated with high frequency from prostatic tissue of patients with BPH and PCa. The presence of this bacterium in the prostate gland may be a predisposing factor for inflammation and the development of both diseases.5,6 P. acnes induces the production of chemotactic factors and the secretion of pro-inflammatory cytokines, such as IL-17 produced by CD4(+) T-lymphocytes.7 It has been observed that the expression of IL-17 can stimulate the proliferation of malignant cells and lead to neoangiogenesis by inducing fibroblasts to upregulate vascular endothelial growth factor (VEGF).8 Furthermore, the imbalance in proportion of CD4(+)IL-17(+) cells and regulatory T CD4(+)FoxP3(+) cells (Treg cells) in the tumor microenvironment may exacerbate inflammation and promote carcinogenesis.8,9
The present study aimed to evaluate the infiltration of CD4(+)IL-17(+) and Treg cells in patients with BPH and PCa depending on the presence of P. acnes in the prostate tissue.
Patients and Methods
Study Population
The study group included 54 patients who underwent surgical treatment due to organ-confined prostate cancer and 34 patients treated for BPH. The average age of the patients was 64 (51–78). Material from patients with BPH was obtained by the TURP (transurethral resection of the prostate). The result of the pathomorphological examination was the basis for the classification of the group of BPH patients. Before prostatectomy, patients with PCa were diagnosed by a core needle biopsy of the prostate gland. The aggressiveness of cancer was determined using the Gleason Score. Patients were classified for the study without any Gleason score limitations. The study group consists of patients who, during our research and collecting surgical material, underwent surgery in the Urology Clinic of the Medical University of Lublin. In the study group of patients with PCa: 27 patients had 3 + 3 Gleason score and 27 patients had 3 + 4 Gleason score (Table 1).
 |
Table 1 Characteristics of Patients |
Surgical the Walsh-Donker technique was performed. After removal of the prostate gland fragments, 1 mL each from both lobes was taken in a sterile condition and directly put into the culture medium. The study was approved by the Bioethics Committee at the Medical University of Lublin (Poland) and all subjects gave informed consent. The research complied with the Declaration of Helsinki.
Procedures
The microbiological identification was performed. The fragment of the prostate was taken and incubated on Casman’s medium base and Columbia agar base with 5% sheep blood. The incubation was cultivated in anaerobic conditions. Identification of the cultivated bacteria was made based on morphological and biochemical characteristics using Rapid ID 32. The results were read out using the APILAB program.
The Th17 and Treg intratumoral identification was performed. The mononuclear cells were isolated from the fragment of the prostate samples by density gradient centrifugation using the Gradisol L (Aqua Medica, Poland). The cells were stained with the following antibody conjugates to the surface receptors: anti-CD45 FITC/anti-CD14 PE, anti-CD4 FITC/anti-CD8 PE, and anti-CD3 FITC (Becton–Dickinson, San Jose, CA, USA). The intracellular detection of the FoxP3 and IL-17 was performed, stained with anti-FoxP3 PE and anti-IL-17 PE antibody (Becton–Dickinson, San Jose, CA, USA). The fluorescence-minus-one method or the unstained cell was used for the negative control. The cells were analyzed by flow cytometry BD FACSCanto II. For each analysis, 20,000 events were acquired and analyzed using BD FACSDiva™ software (Becton Dickinson, Franklin Lakes, New Jersey, USA).
Statistical Analysis
The Mann–Whitney U-test was used to assess differences between studied patient group. Differences from baseline within each group were evaluated using the Wilcoxon test. All p values lower than 0.05 were considered significant. Statistical analysis was performed using Statistica 7 software (TIBCO Software Inc, USA).
Results
In the studied samples of the prostate tissue material, P. acnes was detected in 35% of patients with PCa and 41% of individuals treated for BPH.
The relationship between the percentage of CD4(+)IL-17(+) cells and the presence of P.acnes in the prostate gland was analyzed for both disease entities. In patients with BPH who were positive for P. acnes, the infiltration of CD4(+)IL-17(+) cells was statistically significantly higher (P = 0.001) than in patients with BPH in whom this bacterium was not found. In contrast, the percentage of CD4(+)IL-17(+) cells did not differ considerably in individuals with PCa and positive for P.acnes compared to patients with PCa without the presence of this bacterium in the prostate tissue. There were also no significant differences between the infiltration of CD4(+)IL-17(+) cells in treated for PCa with 3 + 3 Gleason score and patients with PCa who had 3 + 4 Gleason score. The correlation between the percentage of CD4(+)IL17(+) cells and the presence of P.acnes in the prostate gland depending on the degree of cancer aggressiveness was also analyzed. However, in the group of patients with PCa and 3 + 3 Gleason score, the infiltration of CD4(+)IL-17(+) cells did not differ statistically prominently in individuals who were positive for P.acnes compared to patients in whom this bacterium was not detected. The same result was obtained in the group of treated for PCa who had 3 + 4 Gleason score (Tables 2 and 3).
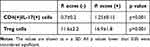 |
Table 2 Percentage of CD4(+)IL-17(+) and Treg Cells. Results for BPH Patients |
 |
Table 3 Percentage of CD4(+)IL-17(+) and Treg Cells. Results for PCa Patients |
The next part of the research was to assess the infiltration of Treg cells depending on the presence of P.acnes in the prostate gland. The percentage of Treg cells was statistically prominently higher (P = 0.001) in patients with BPH and positive P.acnes than in patients with BPH without P.acnes in the prostate tissue. Similarly, there was statistically considerably higher (P = 0.001) infiltration of Treg cells in treated for PCa who had P.acnes compared to individuals with PCa without this bacterium. There was also a statistically significant difference (P = 0.001) between the percentage of Treg cells in patients with PCa who had 3 + 4 Gleason score and those with PCa who had 3 + 3 Gleason score. In the group of patients with PCa and 3 + 3 Gleason score, the infiltration of Treg cells was statistically prominently higher (P = 0.001) in patients with the presence of P.acnes compared to others in whom this bacterium was not detected. Similarly, in the group of patients with PCa who had 3 + 4 Gleason score, a statistically significantly higher (P = 0.001) percentage of Treg cells was found in patients with positive P.acnes compared to the rest (Tables 2 and 3).
Discussion
P. acnes is considered to be one of the pathogens initiating inflammation of the prostate gland and promoting the occurrence of BPH and PCa.5,6 Thus, prostatitis may be the immune system’s response to a bacterial infection.1 It has been also shown that chronic inflammation leads to the prolonged presence of inflammatory cells and factors. Consequently, it can inhibit the apoptosis of transformed cells and contribute to the tumor genesis.2 The conducted research confirmed that the presence of P. acnes in the prostate tissue – in patients with BPH and PCa – is associated with an expanded response of the immune system.
The observed increased percentage of CD4(+)IL-17(+) cells infiltrating the prostate gland in patients with BPH who were positive for P. acnes compared to those in whom the bacterium was not detected suggest that the presence of P. acnes enhances the secretion of IL-17. This pro-inflammatory cytokine is responsible for the occurrence and maintenance of inflammatory lesions.7 It has been also reported that IL-17-producing T cells were found in many tumors, including prostate cancer.8,10
The analyses also showed that the presence of P. acnes in both BPH and PCa patients may significantly affect the intensity of prostate infiltration by Treg cells. The presence of Treg cells in the tumor microenvironment has been previously described. It has been noticed that the abundance of Treg cells infiltration in cancer disease is often associated with a more advanced stage of malignancy.11,12 Our investigation also confirms that the increased frequency of Treg cells is related to the aggressiveness of cancer. Additionally, increased Treg cell prevalence, similar to IL-17 expression, is associated with poor prognosis in cancer patients.8,11,12 This research also found that Treg cell infiltration of the prostate in individuals who had 3 + 3 Gleason score is dependent on the presence of P. acnes. The same correlation was found in the group of patients with a 3 + 4 Gleason score. These results suggest that bacterial infection is crucial to maintaining the inflammation and increasing Treg cell expression.
The magnitude of Treg cell infiltration in PCa patients and the significant difference between Treg cell infiltration in PCa patients with and without P. acnes infection indicate high activity of these cells in the tumor microenvironment. Treg cells may play a role in the development of PCa by inhibiting the immune system’s response. Thus, Treg cells can also prevent the pro-inflammatory reactions by inhibiting the activity of pro-inflammatory cells such as CD4(+)IL-17(+) cells. This may explain the lack of differences in CD4(+)IL-17(+) cell infiltration in the evaluation for PCa patients in this study. A significant increase in PCa inhibitory factors affects the percentage of pro-inflammatory cells and may also be the reason for the difference in CD4(+)IL-17(+) cell infiltration between PCa patients and BPH patients.
It seems that the role of CD4(+)IL-17(+) and Treg cells in the development of chronic inflammation, which may lead to BPH and PCa, should be considered together. The activity of CD4(+)IL-17(+) and Treg cells are antagonistic. The pro-inflammatory cytokine IL-17 as well as the suppressor Treg cells are responsible for controlling inflammation. IL-17-producing T cells may contribute to excess inflammation, in contrast to Treg cells, which may induce too much immunosuppression. This may promote carcinogenesis.8,9 There are many reports indicating that expression of CD4(+)IL17(+) and Treg cells are associated with tumor progression.8,11,12
Conclusions
Infection P. acnes of the prostate gland may play a significant role in the infiltration of prostate tissue by CD4(+)IL17(+)cells and Treg cells in patients with BPH. Similarly, there is also a relevant relationship between infection P. acnes of the prostate gland and Treg cell infiltration of prostate tissue in patients with PCa.
Acknowledgments
The work is subsided from the NCN grant No. NN403 2833 40 (granted to SR).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cai T, Santi R, Tamanini I, et al. Current knowledge of the potential links between inflammation and prostate cancer. Int J Mol Sci. 2019;20:3833.
2. Korniluk A, Koper O, Kemona H, Dymicka-Piekarska V. From inflammation to cancer. Ir J Med Sci. 2017;186(1):57–62. doi:10.1007/s11845-016-1464-0
3. McLaughlin J, Watterson S, Layton AM, Bjourson AJ, Barnard E, McDowell A. Propionibacterium acnes and Acne Vulgaris: new insights from the integration of population genetic, multi-omic, biochemical and host-microbe studies. Microorganisms. 2019;7(5):128. doi:10.3390/microorganisms7050128
4. Achermann Y, Goldstein EJ, Coenye T, Shirtliff ME. Propionibacterium acnes: from commensal to opportunistic biofilm-associated implant pathogen. Clin Microbiol Rev. 2014;27:419–440.
5. Kakegawa T, Bae Y, Ito T, et al. Frequency of Propionibacterium acnes infection in prostate glands with negative biopsy results is an independent risk factor for prostate cancer in patients with increased serum PSA titers. PLoS One. 2017;12(1):e0169984. doi:10.1371/journal.pone.0169984
6. Dadashi M, Eslami G, Taghavi A, et al. Is Propionibacterium acnes a causative agent in benign prostate hyperplasia and prostate cancer? Arch Clin Infect Dis. 2018;13(3):e58947. doi:10.5812/archcid.58947
7. Kistowska M, Meier B, Proust T, et al. Propionibacterium acnes promotes Th17 and Th17/Th1 responses in acne patients. J Invest Dermatol. 2015;135(1):110–118. doi:10.1038/jid.2014.290
8. Liu J, Duan Y, Cheng X, et al. IL-17 is associated with poor prognosis and promotes angiogenesis via stimulating VEGF production of cancer cells in colorectal carcinoma. Biochem Biophys Res Commun. 2011;407(2):348–354. doi:10.1016/j.bbrc.2011.03.021
9. Saleh R, Elkord E. FoxP3+ T regulatory cells in cancer: prognostic biomarkers and therapeutic targets. Cancer Lett. 2020;490:174–185. doi:10.1016/j.canlet.2020.07.022
10. Fabre J, Giustiniani J, Garbar C, et al. Targeting the tumor microenvironment: the protumor effects of IL-17 related to cancer type. Int J Mol Sci. 2016;17(9):1433. doi:10.3390/ijms17091433
11. Shou J, Zhang Z, Lai Y, Chen Z, Huang J. Worse outcome in breast cancer with higher tumor-infiltrating FOXP3+ Tregs: a systematic review and meta-analysis. BMC Cancer. 2016;16(1):687. doi:10.1186/s12885-016-2732-0
12. Tang Y, Xu X, Guo S, et al. An increased abundance of tumor-infiltrating regulatory T cells is correlated with the progression and prognosis of pancreatic ductal adenocarcinoma. PLoS One. 2014;9(3):e91551. doi:10.1371/journal.pone.0091551
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
