Back to Journals » Patient Preference and Adherence » Volume 16
Individuals’ Experiences of Being Screened for Hypertension in Dental Health Care – “No Big Deal”
Authors Andersson H , Bergh H , Bergman S, Bergsten U
Received 2 March 2022
Accepted for publication 13 May 2022
Published 11 June 2022 Volume 2022:16 Pages 1449—1456
DOI https://doi.org/10.2147/PPA.S364689
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Helen Andersson,1,2 Håkan Bergh,2,3 Stefan Bergman,2 Ulrika Bergsten3
1Hallands Hospital Varberg, Varberg, Sweden; 2School of Public Health and Community Medicine, Institute of Medicine, University of Gothenburg, Gothenburg, Sweden; 3Department of Research & Development Unit, Hospital Varberg, Region Halland, Varberg, Sweden
Correspondence: Helen Andersson, Email [email protected]
Background: Hypertension is a common disease globally that accounts for the highest number of lost healthy life years and strongly associated with sequelae such as stroke and myocardial infarction. Early detection of individuals with high blood pressure can be ensured by screening also those who consider themselves “healthy”. Screening has both positive and negative effects where a diagnosis of hypertension can lead to worry about the future. These effects need to be elucidated in order to balance between benefit and harm before screening is introduced. The aim of the study was to describe individuals’ experiences of being screened for hypertension in dental health care.
Methods: Data from individual semi-structured interviews, with twenty participants screened for cardiovascular risk factors in connection with dental examination and aged 55– 80 years, were analysed by means of qualitative content analysis.
Results: The results describe individuals’ experiences of blood pressure screening in dental health care by means of the following theme: “No big deal” based on two categories: “Convenient way of measuring blood pressure” and “Increased awareness of health”.
Conclusion: The overall message from the interviews was that having one’s blood pressure measured when visiting the dentist was convenient, easy and “No big deal”. Blood pressure screening did not create any major concerns and contributed to an increased awareness of health.
Keywords: patients´ experiences, hypertension, blood pressure, screening, dental health care
Introduction
Hypertension or high blood pressure (BP) is a significant health problem worldwide as well as a common disease that accounts for the highest number of healthy life years lost globally.1 It is strongly associated with sequelae such as stroke and myocardial infarction.2 The sequelae of hypertension cause suffering for the affected individuals as well as large costs to society. In Sweden, high BP is present in an estimated 1.8 million people, representing 27% of the adult population.3 Up to 38% of those with high BP are unaware of their condition.3 As there are effective treatments that reduce both high BP and the individual’s risk of developing sequelae, it is important to identify those who have high BP at an early stage. Early detection of individuals with high BP can be achieved by screening those who consider themselves “healthy”. One type of screening is opportunistic screening, utilizing an existing health care or other facility that provides screening in addition to its regular duties.
The goal of systematic screening is to prevent the development of disease and death in a healthy population.4 Through systematic screening, risks such as high BP can be identified. Based on the World Health Organisation (WHO) screening criteria,5–7 there are several reasons why hypertension is suitable for screening.8 These reasons are that hypertension is a health problem where the natural process is known, it constitutes an asymptomatic condition that can be detected, suitable test and effective treatment methods are available, early detection can reduce morbidity and mortality and the test method is feasible and not unpleasant. Detection of hypertension at an early stage reduces the risk of comorbidities and leads to fewer symptoms and perhaps even less extensive treatment, which in turn can lead to improved quality of life. However, the number of affected individuals identified by screening and their experiences is limited. The benefit is great for those identified, but as so few are found, it is important that the screening does not have any negative consequences for those who participate. Being diagnosed with hypertension can lead to worry about the future. There could be fear about the consequences of hypertension if persons tend to overestimate the risk of stroke. It has been shown that participation in screening for cancer or aortic aneurysm may be associated with a certain degree of anxiety,9–11 although this is usually a transient phenomenon.10–12 We have not found any previous study on individuals’ experience of hypertension screening. These effects need to be clarified so that the balance between benefit and harm can be established before screening is introduced. The aim of the study was to describe individuals’ experiences of screening for hypertension in dental health care.
Materials and Methods
This qualitative study with a content analysis approach is a complement to an ongoing screening study in Region Halland (unpublished). The study was carried out by a research group consisting of primary care doctors and registered nurses, all with long experience of patients with serious diseases. The authors each brought a different knowledge base, pre-understanding and experience to the study and data analysis.
Study Setting and Participants
In the main study,13 1000 individuals aged 55–84 years were consecutively screened for cardiovascular risk factors (excluded individuals with atrial fibrillation and blood dialysis) in connection with their annual dental examination at two dental clinics. The participants answered a questionnaire (background and medical conditions) after which their BP, waist and hip circumference were measured, and a blood sample (glucose and lipids) collected. If their BP was high (≥ 140/90 mm Hg) they were asked to measure their BP at home for one week, and if it remained high, they were recommended to seek further assessment at their primary healthcare centre. The blood pressure was measured by well-trained dental nurse and hygienist, with a fully automatic blood pressure device (Omron M& Comfort, Omron Healthcare Ltd., Kyoto, Japan, 2013) were measure.
From the main study and based on information from the questionnaire and on the results of the BP measurement a strategic sample (n=32) of these participants (with no diagnosis of hypertension or diabetes mellitus) was selected in terms of age and gender to obtain variance. A letter with an invitation to participate in the study was sent to the potential participants. A follow-up request via text message was sent after one week. Twenty individuals agreed to participate, 9 females and 11 males aged between 56 and 77 years. Ten of the participants still had high BP, >135/85, after the home blood pressure measurement, while ten participants had normal BP, < 135/85 (Table 1). The interviews took place 3–6 months after the BP screening. This study was conducted from March to July 2020.
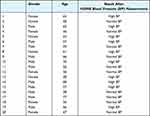 |
Table 1 Characteristics of the Informants |
Data Collection
The main data collection method in this study was semi-structured interviews. After agreeing to participate in the study and signing an informed consent, the participants were allowed to choose a time and place for the interview. Six interviews were conducted “face-to face” in a private room and fourteen took place over the telephone because of the ongoing Covid-19 pandemic. Each interview began with the question; “Can you please describe how you experienced having your blood pressure taken during the dental visit?” The follow-up questions varied, depending on the participant’s response. The interviews enabled us to gain a deeper understanding of the studied phenomenon and were recorded using a digital voice recorder. Each interview was transcribed and then analysed step by step. The duration of each interview was between 15 and 30 minutes and were including the time required to obtain informed consent. The first author, a nurse, who is well educated in interview technique, conducted all the interviews.
Data Analysis
In order to assess the participants’ views and experiences, content analysis was employed in accordance with Graneheim and Lundman.14,15 Each interview was transcribed verbatim, after which the transcripts were read several times to obtain a general understanding of the content. The data were then divided into semantic units and assigned a concept name (code). Codes with similar concepts were combined in a group, thus constituting categories. The categories and codes of each interview were constantly compared with those of the other interviews until subcategories and main categories emerged. Finally, the analysis was completed by identifying the theme that emerged from the participants’ experiences.
To ensure trustworthiness, all steps of the analysis were performed jointly by the first and the last author. The classification and formulation of subcategories, categories and the theme were discussed at meetings attended by all four authors until consensus was achieved.
Ethical Considerations
The study was approved by the Regional Ethical Review Board in Lund, Sweden (Diary no; 2019–06233) as a supplement to the first study (Diary no; 2018/60) to comply with the Swedish Ethical Review Act and subsequently, the Declaration of Helsinki.16
The aims and methods applied in this research were explained in detail to the participants. All participants were volunteers and provided their informed consent before taking part in the research. They were informed about the confidentiality and anonymity of the study, the fact that participation was voluntary and that it was possible to withdraw from the study at any time without consequences for their future care.
Results
The analysis resulted in one theme: “No big deal” and two categories: “Convenient way of measuring BP” and “Increased awareness of health”. In the presentation of the results, the theme and categories are used as headings and the subcategories as subheadings. An overview of the results is provided in Table 2.
 |
Table 2 Overview of the Results; Theme, Categories, and Subcategories |
“No Big Deal”
The overall message from the interviews was that having one’s BP measured during a visit to the dentist was “No big deal” but instead was both convenient and easy.
Participation in BP screening did not create any major concerns but led to an increased awareness of health.
A Convenient Way of Measuring BP
Easy to Do
The participants stated that there was no problem having their BP measured during their dental visit. They described it as easy and no different to having BP measured elsewhere. It was seen as an opportunity to regularly monitor their BP and health.
Because it’s so simple and if there are individuals who are far above what it [blood pressure] should be and do not think about it in everyday life, then they will have it checked at least every second year, as that is how often you visit the dentist. [14]
Saving Resources
The participants expressed that it is beneficial to have other checks performed at a dental visit, in addition to examining their teeth. Coordinating dental care and health care was considered valuable, as it saved time and money for both the population and society.
I suppose that doing several things at the same time saves time and cost. As both myself and society allocate time to this, it seems wise to do things that are helpful for keeping people safe from diseases and such like. [7]
Getting It Done
The participants mentioned various reasons for why they did not check their BP themselves and generally only had it done in connection with primary health care, blood donation or similar visits. They explained that one does not usually seek care or monitor one’s BP when one feels healthy. For the most part, their experience was that BP is only checked before surgery or in the event of accidents.
I would actually like to have an appointment, but it is difficult for me to find time to go and test my levels, so I have just postponed it. [4]
Positive Attitude to Prevention
The interviews clearly showed that the participants are of the opinion that prevention strategies such as examinations or screening are important. The participants expressed that it is vital to know if one is in the risk zone and if such knowledge comes at an early stage, there is an opportunity to do something about the condition.
Then you get to know if you are at risk of various things. And I was informed that I have high blood pressure. [5]
It makes you aware of having a disease at an early stage, which makes it easier to do something about it, so to speak. [9]
Impact of Dental Fear
Participants concluded that fear of dental care could affect their BP and appreciated the opportunity to measure their BP at home in order to determine if fear of the dental examination was the reason for their high BP.
I suppose it was a bit high at the time, but although I have no dental fear it was not exactly something that I had been looking forward to. So, I was definitely a bit tense, because my blood pressure was not high when I measured it at home. [6]
And then, going to the dentist is not exactly pleasant …. at that time my blood pressure was high but when I brought the monitor home with me, my level was normal. [9]
Increased Awareness of Health
Measuring is Beneficial
The interviews revealed that the participants believed it was positive to have an extra health check. As a result, the awareness of their BP became somewhat greater, and they gained a little more control over their health. An interest in acquiring one’s own BP measurement device was also revealed.
I think it was a good opportunity to have my health checked. My diastolic pressure was a bit high, so I was allowed to take the device home with me, and it felt good to do an extra check. An extra health check is not a bad idea, you know, and we talked about it at home and concluded that perhaps we ought to have such a monitor to be able to check now and then. [2]
Gaining Knowledge
The participants considered it was easy, fun and educational to measure their BP at home. But it could also make them a little nervous in case their BP would be high.
I was able to observe that it was at a satisfactory level when there was no stress. My blood pressure somehow rises when I become stressed but perhaps that is normal. It’s good to know though. [7]
The good thing was that I was allowed to bring the monitor home and was able to check. I find being allowed to bring the device home a very positive experience. [7]
Evoking Emotions
The participants described that at the time of the screening they focused on BP, which could create some anxiety but also increase awareness. They felt calmer when they heard that their BP was normal, but there were also thoughts about why BP was high at times and on other occasions almost normal. The interviews also revealed that the participants thought about their lifestyle.
While you are doing it you become more focused on it, which is both good and bad. Perhaps you feel more aware, which can increase your worry. [13]
Becoming Aware of Cardiovascular Risk
It appears from the interviews that the participants were not very concerned about cardiovascular disease, despite knowing people who suffered from hereditary high BP or cardiovascular disease.
I have not given it much though. There’s a lot of talk, but I have not really thought about it. But my relatives have high BP, my brothers. So perhaps it’s in the genes. I have not thought much about it, but apparently exercising can make it go away. [3]
Discussion
In this study we examined the experiences of “healthy” individuals who attended a BP screening for hypertension in a dental health care setting. We found that the participants described the experiences as “No big deal” and highlighted the fact that it was convenient and easy to have their BP measured during a visit to the dentist. In addition, it created an awareness of health, which was enhanced by performing BP monitoring at home. It was also educational, as it led to reflection on health and lifestyle. Another aspect that was highlighted in the interviews was possible dental fear, which could affect the BP measurement. As previously pointed out, the screening can result in false positive results, called White coat hypertension.17,18 This phenomenon can lead to unnecessary meetings, overcrowding in health care and some patients experiencing needless concern about their health.19 However, despite their fear of dentists, it emerged that the participants found it positive to have their BP checked during the dental visit.
Surprisingly, screening BP for hypertension does not seem to create as much anxiety as cancer screening9–11 and cardiovascular disease does not appear to be a concern. This may be because high BP and hypertension are not perceived as a disease, but a chronic condition.20 The participants did not experience any major concern about the fact that at times their BP was high, such as during a dental visit. The home BP measurement probably helped to calm the participants, thus making them less anxious. In addition, hypertension is mainly a condition caused by an affluent lifestyle. The participants felt that it was good to know if they were in the risk group, as they believed that they could deal with the condition themselves through lifestyle changes or medication.
Previous research has addressed the issue of “labelling” and suggested that hypertension labelling might evoke fear of a serious disease in patients.21–23 It has also been demonstrated that living with a chronic condition can be stigmatizing depending on the visibility of the condition and whether it is congenital or acquired.24 Furthermore, it may lead to poorer physical and mental health as well as a limited life.25 The results of this study did not indicate any of these concerns. Instead, the findings clearly showed that the participants appreciated preventive healthcare measures and considered examinations and screening important. They expressed that it was valuable to know if they were in the risk zone, as early detection provides an opportunity to do something about it as well as stating that it was easy and educational to check their BP at home.
In recent years, a great deal has changed in both society and health care. The healthcare organization has altered its approach from seeing patients as passive recipients of care to encountering them as active partners with the right to be involved in and take responsibility for their own health. Self-care is mostly described as tasks performed by healthy persons to prevent the onset of an illness, while self-management involves tasks performed on a day-to-day basis to control or reduce the impact of an illness.26 Self-management could help patients to achieve BP control and prevent complications such as heart failure and stroke, thus improving their overall health status.27 This form of self-care for monitoring BP becomes lifestyle-centred and contextually anchored in the individual’s own daily activities.28 This new perspective poses a challenge to promote and develop such self-care initiatives.
To enable broad preventive public health work, dental care in collaboration with the healthcare system could carry out regular medical screening to identify risk groups at an early stage, thereby reducing both oral and general ill health in the population.
The interviews clearly revealed that regular BP monitoring was desirable as an extra precaution because the participants believed it was important to know if they were in the risk zone, even at an early stage of the condition. The aim of BP screening in dental care is to identify patients at risk, not to make medical diagnoses. Therefore, it is essential to have well-established cooperation with primary healthcare for optimal management of opportunistic medical screening.19
Limitations and Strengths
Studies on individuals’ experiences of being offered BP screening are more or less non-existent. Therefore it is important to describe individuals’ experiences of screening for hypertension. Our results should be considered in the context of some limitations and strengths.
The first limitation is that because of the Covid-19 situation, most interviews were conducted by telephone. It is possible that the participants experienced a distance between themselves and the interviewer and that a personal meeting would have led to a different result. However, the authors are of the opinion that the data from the telephone interviews do not differ from those of the face-to-face interviews. The second limitation is that the participants were recruited from a medical screening study where the aim was to identify a link between oral status and cardiovascular risk factors so the focus may not have been on BP measurement. Finally, we know nothing about the participants’ socio-economic background, which could affect the result. There is also a possibility that those who agreed to participate are generally more positive about screening and prevention, which could also have an impact on the result. The age selection between 55 and 84 years could also be a limitation that can have an impact. However, as hypertension increases with age, the age selection is relevant from a cost-effective perspective. All interviews ended with a question about whether the participant wished to add anything. Such a concluding question strengthens reliability, as it can provide additional relevant information that corresponds to the aim.15 The interviews were conducted 3–6 months after the BP screening which can be considered a long time to remember. But in order to be able to take part in the participants’ experiences of participating in screening for hypertension, from BP measurement to possible diagnosis, it was important to ensure that all participants had the time to complete the entire screening process, which is about 3 months. A strength of the present study is the variation among the participants in terms of age, gender and screening outcome, which can contribute to a richer variation in experiences.15 Another strength is the difference in the authors’ knowledge base, pre-understanding and disciplines (nurses and general practitioners).
Conclusion
Mass examinations and screening can be very useful – but this is not always the case. There is growing scepticism about screening surveys and their results. However, in the present study the participants stated that having their blood pressure measured when visiting the dentist was “No big deal” but convenient and easy. Blood pressure screening did not create any major concerns and led to an increased awareness of health.
Acknowledgments
The authors would like to thank the participants from the dental health and primary care clinics for their time and effort.
Funding
This work was supported by grants from the County Council of Halland, Sweden.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi:10.1016/S0140-6736(12)61766-8
2. Lewington S, Clarke R, Qizilbash N, Peto R, Collinset R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913.
3. Lindholm LH, Carlberg B Moderately elevated blood pressure. A systematic literature review. Volumes 1 & 2. Stockholm: The Swedish Council on Technology Assessment in Health Care 2004. SBU-rapport 170=1: 1–514 and 170=2:1–248.
4. Epidemiology, A basis for public health and disease prevention Dag S. Thelle 2015.
5. Wilson J, Junger G. Principles and Practice of Screening for Disease, Public Health Papers. Geneva: World Health organization; 1986.
6. 1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens. 1999;17(2):151–183.
7. Available from: http://www.socialstyrelsen.se/riktlinjer/nationellascreeningprogram.
8. WHO. World Health Organization; 2011; Available from: http://www.who.int/cancer/detection/en.
9. Bolejko A, Zackrisson S, Hagell P, Wann-Hansson C. A roller coaster of emotions and sense–coping with the perceived psychosocial consequences of a false positive screening mammography. J Clin Nurs. 2014;23:2053–2062. doi:10.1111/jocn.12426
10. Kus T, Aktas G, Ekici H, Elboga G, Djamgoz S. Illness perception is a strong parameter on anxiety and depression scores in early-stage breast cancer survivors: a single-center cross-sectional study of Turkish patients. Support Care Cancer. 2017;25(11):3347–3355. doi:10.1007/s00520-017-3753-1
11. Spencer CA, Norman PE, Jamrozik K, Tuohy R, Lawrence-Brown M. Is screening for abdominal aortic aneurysm bad for your health and well-being? ANZ J Surg. 2004;74:1069–1075. doi:10.1111/j.1445-1433.2004.03270.x
12. Wardle J, Pope R. The psychological costs of screening for cancer. J Psychosom Res. 1992;36:609–624. doi:10.1016/0022-3999(92)90051-3
13. Bergh H, Albrektson M, Kastberg C, Baigi A, Hedström H. The Association Between Sublingual Varices and Cardiovascular Risk Factors. Vasc Health Risk Manag. 2022;18:319–327. doi:10.2147/VHRM.S354021
14. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures, and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112. doi:10.1016/j.nedt.2003.10.001
15. Graneheim UH, Lidngren B, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today. 2017;56:29–34. doi:10.1016/j.nedt.2017.06.002
16. World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79(4):373.
17. Franklin SS. On behalf of the International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators. Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes population. Hypertension. 2012;59(3):564–571. doi:10.1161/HYPERTENSIONAHA.111.180653
18. Andersson H, Hedström L, Bergh H. White coat hypertension detected during opportunistic blood pressure screening in dental healthcare setting. Scand J Prim Health Care. 2021;39(3):348–354. doi:10.1080/02813432.2021.1958496
19. Friman G, Golestani G, Kalkali A, Wårdh I, Hultin M. Patient experiences of medical screening performed by dental services: a qualitative study. Open J Stomatol. 2013;3(9):497–503. doi:10.4236/ojst.2013.39081
20. Silva FMD. Hypertension as a conditioner of non-disease: the meaning of chronicity in subjects ‘perspective. Texto Contexto Enferm. 2013;22(1):123–131. doi:10.1590/S0104-07072013000100015
21. Pickering TG. Now we are sick: labeling and hypertension. J Clin Hypertension. 2006;8:57–60. doi:10.1111/j.1524-6175.2005.05121.x
22. Hamer M, Batty GD, Stamatakis E, Kivimaki M. Hypertension awareness and psychological distress. Hypertension. 2010;56:547–550. doi:10.1161/HYPERTENSIONAHA.110.153775
23. Michal M, Wiltink J, Lackner K, et al. Association of hypertension with depression in the community: results from the Gutenberg Health Study. J Hypertens. 2013;31:893–899. doi:10.1097/HJH.0b013e32835f5768
24. Joachim G, Acorn S. Stigma of visible and invisible chronic conditions. J Adv Nurs. 2000;32(1):243–248. doi:10.1046/j.1365-2648.2000.01466.x
25. Charmaz K, Charmaz K. Loss of self: a fundamental form of suffering in the chronically ill. Sociol Health Illn. 1983;5(2):168–195. doi:10.1111/1467-9566.ep10491512
26. Clark NM, Becker MH, Janz NK, Lorig K, Rakowski W, Anderson L. Self- Management of Chronic Disease by Older Adults. J Aging Health. 1991;3(1):3–27. doi:10.1177/089826439100300101
27. Dickson VV, Lee C, Yehle KS, Abel WM, Riegel B. Psychometric testing of the self-care of hypertension inventory. J Cardiovascular Nursing. 2017;32(5):431–438. doi:10.1097/JCN.0000000000000364
28. Bengtsson U, Kjellgren K, Hallberg I, Lundin M, Mäkitalo Å. Patient contributions during primary care consultations for hypertension after self-reporting via a mobile phone self-management support system. Scand J Prim Health Care. 2018;36(1):70–79. doi:10.1080/02813432.2018.1426144
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
