Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
Individual Perceived Stress Mediates Psychological Distress in Medical Workers During COVID-19 Epidemic Outbreak in Wuhan
Authors Zhang C, Peng D , Lv L, Zhuo K, Yu K , Shen T , Xu Y , Wang Z
Received 8 June 2020
Accepted for publication 12 September 2020
Published 28 October 2020 Volume 2020:16 Pages 2529—2537
DOI https://doi.org/10.2147/NDT.S266151
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jun Chen
Chen Zhang,1– 3 Daihui Peng,1– 3 Lu Lv,4 Kaiming Zhuo,1,3 Kai Yu,5 Tian Shen,4 Yifeng Xu,1,2 Zhen Wang1– 3
1Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 2Shanghai Key Laboratory of Psychotic Disorders, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 3Shanghai Psychological Medical Team Supporting Hubei, Shanghai, People’s Republic of China; 4School of Public Health, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 5MoE Key Laboratory of Artificial Intelligence, AI Institute Shanghai Jiao Tong University, Shanghai, People’s Republic of China
Correspondence: Zhen Wang Email [email protected]
Yifeng Xu Email [email protected]
Background: Since the novel coronavirus disease (COVID-19) outbreak in Wuhan, thousands of medical workers have been dispatched to support Wuhan against the virus. The purpose of this study was to identify the independent risk factors for psychological distress in order to develop a more effective strategy and precise evidence-based psychological intervention for medical workers.
Methods: This multisite cross-sectional survey recruited doctors and nurses from local and nonlocal medical teams working at 16 hospitals in Wuhan to complete this online survey from February to March, 2020. Psychological status was evaluated through Perceived Stress Scales (PSS), Patient Health Questionnaire-9 (PHQ-9), General Anxiety Disorder Scale (GAD-7) and Acute Stress Disorder Scale (ASDS).
Results: Of 966 participants, the prevalence of stress (95.9%), depression (46.0%) and anxiety (39.3%) were high. Local medical workers exhibited even higher scores of PSS, PHQ-9, GAD-7 and ASDS than those from outside Hubei (P< 0.001). Females had more severe perceived stress, depression and anxiety than males (P< 0.001). Multiple logistic regression showed that perceived stress is associated with increased odds of depression (OR=1.413; 95% CI: 1.338– 1.493; P< 0.001) and anxiety (OR=1.515; 95% CI: 1.407– 1.631; P< 0.001).
Conclusion: Our findings demonstrated a high prevalence of stress, depression, anxiety and acute distress among medical workers on the front-line during the COVID-19 outbreak in Wuhan. The level of psychological impact may be mediated by individual perceptions of stressful events.
Keywords: COVID-19, stress, anxiety, depression, Wuhan
Introduction
Since late December 2019, the novel coronavirus disease (COVID-19) has emerged and rapidly spread in Wuhan, China. COVID-19 can be transmitted person-to-person, and infected patients may develop fatal conditions. Although a number of strict measures such as quarantine and lock down were adopted to curb the spread of COVID-19, a surge of daily new confirmed cases have overwhelmed the health care system in Wuhan. This also led to severe mental health burden in the early phase.1 In order to alleviate the pressure on the medical system in Wuhan, the Chinese government dispatched medical teams from all over the country to support Wuhan. From the end of January 2020, tens of thousand doctors and nurses among other staff from other provinces in China aggregated in Wuhan to fight against COVID-19. By the end of March 2020, these supporting medical workers took over a large portion of responsibilities to diagnose, treat and care for patients with COVID-19, which greatly alleviated the burden on the local health care system in Wuhan and saved thousands of lives and families. However, the challenges these medical workers have been facing were unprecedented, with or without preparation before they landed, as they worked in the closed environment and dealt with highly traumatized infectious patients face to face.
The experience of SARS in 2003 manifested the short- and long-term psychological impact of epidemics on front-line medical workers.2–4 Such psychological distress may be associated with trauma events.5–7 The SARS outbreak has highlighted the importance of psychological intervention on front-line medical workers.8 Therefore, during the COVID-19 epidemic outbreak, the Chinese government has established psychological intervention teams for medical workers in Wuhan to offer peer psychological assistance services, such as psychological counseling, brochures and psychotherapy.9 It is believed that timely and effective psychological intervention would help medical workers take precautions against emotional and psychiatric problems.
It is known that designated and Fangcang shelter hospitals play important role in this massive rescue operation against COVID-19.10,11 Medical workers in both hospitals probably face different risk factors and cope with different psychological distress. Although there are surveys showing the mental distress of medical workers in Wuhan,12–14 it is not known if there is a differencein psychological status between different working locations (designated and shelter hospitals) or different origins of medical teams (Hubei and outside Hubei). This knowledge would facilitate the strategy of developing more effective and precise evidence-based psychological intervention for medical workers. The purpose of this study was to investigate the psychological status in medical workers who work in different locations and from different medical teams in Wuhan in order to identify the independent risk factors.
Methods
Subjects
All procedures were reviewed and approved by Institutional Review Boards of Shanghai Mental Health Center (IRB number: 2020–10). This study was performed in accordance with the guidelines laid out in the Declaration of Helsinki as revised in 1989. This multisite cross-sectional survey recruited doctors and nurses from local and nonlocal medical teams working in 16 hospitals in Wuhan to complete this online survey from February, 2020 to March, 2020. The period of this survey covered the peak of COVID-19 epidemic outbreak in Wuhan. We collected the data via Wenjianxing platform (www.wjx.cn) with an anonymous self-rated questionnaire. All participants were required to meet the following conditions: (1) age >20 years, (2) no dyslexia, (3) front-line medical workers in Wuhan, (4) in good physical health with no heart, liver, kidney or other physical diseases, not take any medicine for nearly 1 month, (5) never been diagnosed with a mental disorder, (6) willing to participate in this survey. The exclusion criterion was that the answer time for all questions was > 30 min or < 2 min. All subjects provided electronicinformed consent before any study-related procedures were performed. Only subjects who selected yes were taken to the questionnaire page and participated in this study.
Clinical Evaluation
The 14-item Perceived Stress Scales (PSS)15 was used to assess life stress with subjects responding how often they had epidemic thoughts and feelings over the last month (0 equating to “never”, 1 equating to “rarely”, 2 equating to “sometimes”, 3 equating to “fairly often”, 4 equating to “very often”). The total PSS score summarizes the total scores of each item, with higher values indicating more life stress. The total PSS score is interpreted as: normal (0–3), mild (4–10), moderate or severe (≥11) perceived stress.
The Patient Health Questionnaire-9 (PHQ-9)16 was used to evaluate the occurrence and severity of depressive symptoms, which exhibits good validity and reliability for screening depression. Subjects rate the frequency of depressive symptoms with the last two weeks on a 4-point scale ranging from 0 equating to “not at all” to 3 equating to “nearly every day”. The severity of depressive symptoms was evaluated as a continuously summarized score (from 0 to 27). The total PHQ-9 score is interpreted as: normal (0–4), mild (5–9), moderate or severe (≥10) depression.
The 7-item General Anxiety Disorder scale (GAD-7)17 was used to measure anxiety severity in the past two weeks. A 4-point Likert scale ranging from 0 equating to “not at all” to 3 equating to “almost every day” in the past two weeks was required for question answering. The total score ranges from 0 to 21 with higher values indicating more severe anxiety. The total GAD-7 score is interpreted as: normal (0–4), mild (5–9), moderate or severe (≥10) anxiety.
The 19-item Acute Stress Disorder Scale (ASDS)18 was used to evaluate the prevalence of psychiatric symptoms of acute distress induced by COVID-19. The ASDS composed of 4 subscales referring to ASD symptoms of dissociation, re-experiencing, avoidance and arousal. Each item is scored on a 5-point Likert scale from 0 equating to “not at all” to 4 equating to “extremely”. The ASDS total score ranges from 0 to 76 with higher values indicating stronger stress. The total ASDS score is interpreted as: normal (0–55), acute stress disorder (≥56).
Statistical Analysis
The data was analyzed using SPSS statistical software version 22.0 (IBM Corp). All tests were two-tailed, and the significance level was set at α=0.05. As the scores of the 4 measurement tools were not normally distributed, so they were presented as median with interquartile ranges (IQRs). Numbers and percentages were used to present the severity of symptoms, which were derived from scores of the scales about stress, depression, anxiety and acute stress disorder. The severity of symptoms between 2 or more groups were compared using the nonparametric Mann–Whitney U-test and Kruskal–Wallis test. To explore the relationship between the potential risk factors and the severity of symptoms, the Kendall’s tau-b, univariate and multivariate logistic regression analysis were performed. The associations between potential risk factors and outcomes were presented as odds ratios (ORs) and 95% Cis after adjustment for confounders including sex, age, type of hospital, place of residence and the Perceived Stress Scale (PSS) score.
Results
Demographic Characteristics
A total of 966 participants completed this survey. The statistical power was more than 80% (α=0.05) under the assumption of a moderate effect size. Table 1 showed that 33.9% and 66.1% were from Hubei and outside Hubei, respectively. The participants tended to be female (76.4%) and worked in designated hospitals (90.4%).
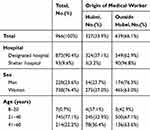 |
Table 1 Demographic and Occupational Characteristics of Responders |
Severity of Measurements and Associated Factors
As shown in Table 2, of all participants, medical workers exhibited high prevalence of stress (95.9%), depression (46.0%) and anxiety (39.3%). Local medical workers had higher scores of PSS, PHQ-9, GAD-7 and ASDS than those from outside Hubei (P<0.001). Female medical workers felt more severe perceived stress, depression and anxiety than males (P<0.001). In contrast, there was no significant difference of perceived stress, depression and anxiety between designated and shelter hospitals (P>0. 05).
 |
Table 2 Severity Categories of Stress, Depression, Anxiety and Acute Stress Disorder Measurements in Total Responders and Subgroups |
Scores of Measurements and Associated Factors
The median (IQR) scores on the PSS for stress, the PHQ-9 for depression, the GAD-7 for anxiety, and the ASDS for acute stress disorder for all respondents were 15.0 (11.0–19.0), 4.0 (2.0–8.0), 3.0 (0.0–7.0), and 30.0 (24.0–38.5), respectively. Similar to the findings in severity of symptoms, participants who were local medical workers and female had higher scores of PSS, PHQ-9, GAD-7 and ASDS compared to those who were medical workers from outside Hubei, and male (eg, median [IQR] scores of the measurements among those worked in Hubei vs those worked outside Hubei: PSS, 17.0 [14.0–21.0] vs 14.0 [10.0–17.0], P<0.001; PHQ-9, 6.0 [3.0–9.5] vs 3.0 [1.0–7.0], P<0.001; GAD-7, 5.0 [2.0–8.0] vs 2.0 [0.0–5.0], P<0.001; ASDS, 35.0 [28.0–43.5] vs 28.0 [23.0–17.0], P<0.001; median [IQR] scores of the measurements among men vs women: PSS, 14.0 [9.0–17.0] vs 16.0 [12.0–20.0], P<0.001; PHQ-9, 2.0 [1.0–7.0] vs 4.0 [2.0–8.0], P<0.001; GAD-7, 2.0 [0.0–5.0] vs 4.0 [1.0–7.0], P<0.001; ASDS, 26.5 [22.0–35.0] vs 31.0 [25.0–40.0], P<0.001.). There were no significant differences of perceived stress, depression and anxiety between designated and shelter hospitals (median [IQR] scores of the measurements among designated hospital vs shelter hospitals: PSS, 15.0 [11.0–19.0] vs 14.0 [11.0–18.0], P=0.075; PHQ-9, 4.0 [2.0–8.0] vs 3.0 [1.0–8.0], P=0.267; GAD-7, 3.0 [0.0–6.0] vs 2.0 [0.0–7.0], P=0.61) (Table 3).
 |
Table 3 Scores of Stress, Depression, Anxiety and Acute Stress Disorder |
Risk Factors of Depression and Anxiety
A major purpose of this study was to detect independent risk factors influencing the levels of depression and anxiety in medical workers in Wuhan. Table 4 presented the results of multiple logistic regression models while sequentially adding controls for demographic characteristics, showing that perceived stress is associated with increased odds of depression (OR=1.413; 95% CI: 1.338–1.493; P<0.001) and anxiety (OR=1.515; 95% CI: 1.407–1.631; P<0.001). In this regression model, hospital, sex, age, origin of medical workers and the score of PSS were included, and the backward stepwise logistic regression was applied. A sketch of independent factors influencing the levels of depression and anxiety in medical workers in Wuhan was shown in Figure 1.
 |
Table 4 Risk Factors for Mental Health Outcomes Identified by Multivariable Logistic Regression Analysis |
 |
Figure 1 Sketch of independent risk factors influencing the levels of depression and anxiety in medical workers in Wuhan. **P<0.01. |
Discussion
In this study, we investigated the prevalence of stress, depression, anxiety and acute distress across different medical teams from all of the country working in Wuhan. There are 83.1% and 8.8% of medical workers working in designated and shelter hospitals, respectively. In total, 33.9% of samples are local medical workers from Hubei, and 66.1% originate from other regions in China. Our data demonstrated that front-line medical workers had high prevalence rates of stress, depression and anxiety during the COVID-19 epidemic. This is in line with previous studies,14,19,20 but overall higher than those reported in Singapore.21 When the samples are stratified by the working location, there is no significant difference of stress, depression and anxiety between designated and shelter hospitals. We then detected the differences of mental status in term of origin. Our results showed that local medical workers from Hubei have significantly higher severe stress, depression, anxiety and acute distress than those from other regions.
To the best of our knowledge, this is the first psychological status investigation of medical workers from different regions fighting against COVID-19 in Wuhan. It is a common problem for medical workers to have a psychological response to an epidemic of infectious diseases.22 However, our results showed that local medical workers from Hubei obviously suffered more severe stress, depression, anxiety and acute distress than those from other regions. Since the outbreak of COVID-19 epidemic in Wuhan, local medical workers had to face more and more patients suffering from a known pneumonia caused by the novel coronavirus. Local health care systems were put under tremendous tension by the rapidly rising number of infected cases. As such, the predictable shortage of supplies, fear of being infected, concern about health of self and family, feelings of vulnerability, and being isolated in order not to spread infection at early stage of the epidemic were the sources of distress for the local medical workers from Hubei.23,24 Since the 1st batch of medical teams from outside Hubei arrived in late January 2020, more than 22,000 medical workers fought against COVID-19 together with the local medical workers. Meanwhile, Chinese manufacturers recalled workers from spring festival holiday to plug a shortage of protective suits, masks and other medical supplies. These efforts alleviated the tension on the medical health system as well as the psychological status of medial workers in Wuhan. Therefore, nonlocal medical workers did not experience the duration of acute stress that local ones exposed at early stage of epidemic experienced. This may explain the reason why local medical workers suffered more severe stress, depression, anxiety and acute distress than those from outside Hubei.
Our results showed that gender is another risk factor for the mental status. Female medical workers suffered more severe stress, depression, anxiety and acute distress than males. Most epidemiological studies that have examined the impact of gender on emotion have indicated that females have predisposition for anxiety and depression than males. Its genuine mechanism is still not known, albeit sex role hormones and psychosocial factors are suggested.25 Environmental exposure to COVID-19 may represent a sustained psychosocial stress.26 Stressful events have been long considered relevant triggers for activation of the hypothalamic-pituitary-adrenal (HPA) axis.27 The HPA axis has been implicated in the pathophysiology of a variety of mood disorders, such as depression and anxiety with overactivity of HPA responses.28 HPA axis exhibits a sex-biased activity to control hormonal responses to stress.29 Sex differences in the activation of HPA axis may be influenced by the level of estradiol.30 Therefore, the differences of mental status between male and female medical workers are likely driven by sex hormone in the psychological response to chronic stress caused by COVID-19.
Our multiple logistic regression analysis showed that PSS score is the only independent risk factor for both PHQ-9 and GAD-7 scores. This suggested that high stress level is associated with a higher risk of anxiety and depression. Other factors including working location, origin of medical teams, gender and age did not influence the risk for anxiety and depression in medical workers. We used PSS to scale the level of stress, which requires subjects how often they have found the situations in their unpredictable, uncontrollable, or overwhelming over the past month. Thus, our findings implied that perceivable stress level may play the most important role in the development of anxiety and depression in medical workers. To effectively deal with stress, individuals are naturally equipped with a coping mechanism. However, individuals without the ability to implement positive coping effectively and resolving the stressors may eventually develop psychological health issues.31 As mentioned above, the types of challenges that medical workers faced are similar, such as high risk of being infected, heavy workload and isolated living environment. The differences of coping styles determined the onset or occurrence of anxiety and depression in medical workers in Wuhan. Coping style refers to a cognitive and behavioral strategy used by individuals to overcome, tolerate and offset the internal and external demands of stressful events.32 Then, how to cope with the perceived occupational stress? A Cochrane review has demonstrated that cognitive-behavioral therapy, work-schedule management, mental and physical relaxation could reduce stress to a manageable level.33 Taken together, our results implied that more stress levels the front-line medical workers in Wuhan perceived, more severe levels of anxiety and depression suffered. Self-efficacy has been proven to influence the individual choices of behavioral activities, effort expenditure and persistence when facing obstacle and task performance.34 A growing body of studies most recently has focused on the mediation effect of self-efficacy between stress and physical and psychological outcomes. Studies investigating the relationship between perceived stress and self-efficacy found that high level of perceived stress is associated with low levels of self-efficacy.35 Furthermore, several studies indicated that high level of perceived stress predicted low levels of self-efficacy. Therefore, timely psychological support including availing counseling services, informal or formal supervision and establishing peer support systems are helpful to improve self-efficacy and required to take measures to decrease the stress levels and encourage medical workers to adopt their coping styles.36 Recently, we have investigated the psychological impacts and depression in the nonmedical staff in Wuhan. Our findings suggested that nonmedical staff on the front-line of COVID-19 outbreak also had high rates of symptoms of depression. The female gender, younger age, and increased stress reactions were associated with the increased risk for depression.37 As such, psychological inventions are required for both the medical workers and nonmedical staff.38
This study has several limitations that should be taken into account. First, this is a cross-sectional survey and it is difficult to exhibit the systematic changes of psychological status of medical workers in Wuhan. Second, we used self-rating scales to evaluate stress, anxiety, depression and PTSD. Compared with clinical interviews, self-rating can be a source of bias, with risks of false and over judgment. Third, we did not evaluate the duration of the exposition to the stressful condition when significant differences in multiple outcomes were found between local and nonlocal medical workers. As such, our present findings should be interpreted with caution, and future studies on this subject are suggested to employ a mixed-methods design to explore specific themes and intervention strategies.
In conclusion, our results demonstrated a high prevalence of stress, depression, anxiety and acute distress among medical workers during COVID-19 outbreak in Wuhan. The level of psychological impact may be mediated by individual perceptions of stressful events. Therefore, personalized psychological care from psychotherapists and psychiatrists would benefit the medical workers to decrease the stress levels and adopt their coping styles.
Acknowledgment
We are deeply grateful to all participants.
Funding
This work was supported by the Shanghai Jiao Tong University Key Program for the Medical Engineering Cross Project (YG2020YQ25 to ZW); Shanghai Jiao Tong University Specific Project for COVID-19 Prevention and Control (2020RK60 to CZ).
Disclosure
The authors report no conflicts of interest for this work.
References
1. Moccia L, Janiri D, Pepe M, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun. 2020;87:75–79. doi:10.1016/j.bbi.2020.04.048
2. Chen CS, Wu HY, Yang P, Yen CF. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr Serv. 2005;56(1):76–79. doi:10.1176/appi.ps.56.1.76
3. Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54(5):302–311. doi:10.1177/070674370905400504
4. Lee AM, Wong JGS, McAlonan GM, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007;52(4):233–240. doi:10.1177/070674370705200405
5. Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31(4):318–326. doi:10.1016/j.genhosppsych.2009.03.001
6. Lancee WJ, Maunder RG, Goldbloom DS, Study S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiat Serv. 2008;59(1):91–95. doi:10.1176/ps.2008.59.1.91
7. Chong MY, Wang WC, Hsieh WC, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. 2004;185:127–133. doi:10.1192/bjp.185.2.127
8. Chan AOM, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med. 2004;54(3):190–196. doi:10.1093/occmed/kqh027
9. Kang LJ, Li Y, Hu SH, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):E14–E14. doi:10.1016/S2215-0366(20)30047-X
10. Shang L, Xu J, Cao B. Fangcang shelter hospitals in COVID-19 pandemic: the practice and its significance. Clin Microbiol Infect. 2020;26(8):976–978. doi:10.1016/j.cmi.2020.04.038
11. Chen SM, Zhang ZJ, Yang JT, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–1314. doi:10.1016/S0140-6736(20)30744-3
12. Xiao H, Zhang Y, Kong DS, Li SY, Yang NX. The effects of social support on sleep quality of medical staff treating patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monitor. 2020;26. doi:10.12659/MSM.923921
13. Lai JB, Ma SM, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3):e203976. doi:10.1001/jamanetworkopen.2020.3976
14. Kang LJ, Ma SM, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi:10.1016/j.bbi.2020.03.028
15. Katsarou A, Panagiotakos D, Zafeiropoulou A, et al. Validation of a greek version of pss-14; a global measure of perceived stress. Cent Eur J Public Health. 2012;20(2):104–109. doi:10.21101/cejph.a3698
16. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282(18):1737–1744. doi:10.1001/jama.282.18.1737
17. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
18. Bryant RA, Moulds ML, Guthrie RM. Acute stress disorder scale: a self-report measure of acute stress disorder. Psychol Assess. 2000;12(1):61–68. doi:10.1037/1040-3590.12.1.61
19. Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):242–250. doi:10.1159/000507639
20. Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Network Open. 2020;3(5):e2010185. doi:10.1001/jamanetworkopen.2020.10185
21. Ng QX, De Deyn M, Lim DY, Chan HW, Yeo WS. The wounded healer: a narrative review of the mental health effects of the COVID-19 pandemic on healthcare workers. Asian J Psychiatr. 2020;54:102258.
22. Smith MW, Smith PW, Kratochvil CJ, Schwedhelm S. The psychosocial challenges of caring for patients with ebola virus disease. Health Secur. 2017;15(1):104–109. doi:10.1089/hs.2016.0068
23. Wong TW, Yau JKY, Chan CLW, et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med. 2005;12(1):13–18. doi:10.1097/00063110-200502000-00005
24. Chan-Yeung M. Severe acute respiratory syndrome (SARS) and healthcare workers. Int J Occup Environ Health. 2004;10(4):421–427. doi:10.1179/oeh.2004.10.4.421
25. Parker G, Brotchie H. Gender differences in depression. Int Rev Psychiatry. 2010;22(5):429–436. doi:10.3109/09540261.2010.492391
26. Garcovich S, Bersani FS, Chiricozzi A, De Simone C. Mass quarantine measures in the time of COVID-19 pandemic: psychosocial implications for chronic skin conditions and a call for qualitative studies. J Eur Acad Dermatol Venereol. 2020;34(7):e293–e294. doi:10.1111/jdv.16535
27. Misiak B, Loniewski I, Marlicz W, et al. The HPA axis dysregulation in severe mental illness: can we shift the blame to gut microbiota? Prog Neuropsychopharmacol. 2020;102:109951. doi:10.1016/j.pnpbp.2020.109951
28. Keller J, Gomez R, Williams G, et al. HPA axis in major depression: cortisol, clinical symptomatology and genetic variation predict cognition. Mol Psychiatry. 2017;22(4):527–536. doi:10.1038/mp.2016.120
29. Heck AL, Handa RJ. Sex differences in the hypothalamic-pituitary-adrenal axis’ response to stress: an important role for gonadal hormones. Neuropsychopharmacol. 2019;44(1):45–58.
30. Powers SI, Laurent HK, Gunlicks-Stoessel M, Balaban S, Bent E. Depression and anxiety predict sex-specific cortisol responses to interpersonal stress. Psychoneuroendocrino. 2016;69:172–179. doi:10.1016/j.psyneuen.2016.04.007
31. Labrague LJ, McEnroe-Petitte DM, Papathanasiou IV, et al. Stress and coping strategies among nursing students: an international study. J Ment Health. 2018;27(5):402–408. doi:10.1080/09638237.2017.1417552
32. Shao R, He P, Ling B, et al. Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol. 2020;8(1):38. doi:10.1186/s40359-020-00402-8
33. Ruotsalainen JH, Verbeek JH, Marine A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev. 2015;4:CD002892.
34. Chen Y, Wang YW, Fang XY, Zhang Y, Song LS, Zhang C. Association of the HTR2C-759C/T polymorphism and antipsychotic-induced weight gain: a meta-analysis. Gen Psychiatry. 2020;33(3).
35. Lee J, Kim E, Wachholtz A. The effect of perceived stress on life satisfaction: the mediating effect of self-efficacy. Chongsonyonhak Yongu. 2016;23(10):29–47.
36. Ng QX, Chee KT, De Deyn MLZQ, Chua Z. Staying connected during the COVID-19 pandemic. Int J Soc Psychiatry. 2020;66(5):519–520.
37. Sun XJ, Wang LH, Yang FZ, et al. Correlation of hair risperidone concentration and serum level among patients with schizophrenia. Gen Psychiatry. 2019;32(1).
38. Sani G, Janiri D, Di Nicola M, Janiri L, Ferretti S, Chieffo D. Mental health during and after the COVID-19 emergency in Italy. Psychiatry Clin Neurosci. 2020;74(6):372. doi:10.1111/pcn.13004
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
