Back to Journals » International Journal of Women's Health » Volume 12
Individual, Household, and Contextual Factors Influencing the Timing of the First Antenatal Care Attendance in Northwest Ethiopia: A Two-Level Binary Logistic Regression Analysis
Authors Emiru AA , Alene GD, Debelew GT
Received 22 February 2020
Accepted for publication 9 June 2020
Published 18 June 2020 Volume 2020:12 Pages 463—471
DOI https://doi.org/10.2147/IJWH.S250832
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Amanu Aragaw Emiru,1 Getu Degu Alene,2 Gurmesa Tura Debelew3
1Department of Reproductive Health and Population Studies, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia; 2Department of Epidemiology and Biostatistics, College of Medicine and Health Sciences, Bahir Dar University, Bahir, Ethiopia; 3Department of Population and Family Health, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Amanu Aragaw Emiru
Department of Reproductive Health and Population Studies, College of Medicine and Health Sciences, Bahir Dar University, P.O. Box: 79, Bahir Dar, Ethiopia
Tel +251 918780295
Email [email protected]
Background: Early antenatal visit is critical for the health and well-being of mothers and babies. However, various individual, family level, and contextual factors influence the timely initiation of antenatal care.
Objective: The aim of this study was to examine individual, household, and community-level factors associated with the timing of first ANC visit among mothers who gave birth in the last twelve months before the survey.
Methods: A community-based cross-sectional study was conducted in June 2018. A multistage cluster sampling technique was applied, and a sample of 898 women was considered. Data were collected using a questionnaire and checklist. The analysis was made using SPSS. A multilevel logistic regression with random effects at the kebele level was developed to assess the predictors of late initiation of antenatal care. Odds ratio with 95% confidence intervals was used to measure association while the intra-class correlation coefficient and the median odds ratio were used to measure variations.
Results: Overall, 78.4% (95% CI: 75.6, 80.9) of women started their first ANC in 4 months of gestation or later and significant heterogeneity was observed between clusters. At level 1, women with intended pregnancy (aOR=0.31; 95% CI: 0.12, 0.79), and being knowledgeable about the timing (aOR=0.43; 95% CI: 0.25, 0.75) and pregnancy-related complications (aOR=0.16; 95% CI: 0.10, 0.26) were less likely to delay their first ANC visit. Conversely, the odds of late ANC visit was higher among women with no formal education (aOR=4.08, 95% CI: 2.20, 7.55). Distance to the health facility (aOR=1.04; 95% CI, 1.01– 1.08) was the only level-2 significant predictor.
Conclusion: The study revealed that late ANC initiation was rampant. Several factors operating at different levels were associated with late ANC visits; yet, the role of individual-level factors was relatively stronger. Hence, awareness creation is essential to the underprivileged community using the available communication networks.
Keywords: antenatal care, timing, delay, late, multilevel
Introduction
In September 2015, the United Nations Member States adopted the 2030 Agenda for Sustainable Development; and pledged to reduce maternal mortality ratio to less than 70 per 100,000 live births by 2030.1 However, the burden of maternal mortality in low-resource settings remains unacceptably high.2 In 2017, for example, approximately 295,000 maternal deaths occurred worldwide, and two-third were from Sub-Saharan Africa countries where Ethiopia is found.3 The maternal mortality ratio of 412 deaths per 100,000 live births in Ethiopia,4 is among the highest in the world.
Many of the maternal deaths can be prevented by expanding access to essential maternal health packages from pre-pregnancy to delivery, and during the postnatal period. As part of the continuum of reproductive health care, antenatal care (ANC) provides an opportunity for health promotion, disease prevention, and early diagnosis and treatment of illnesses.2,5 In 2016, the World Health Organization (WHO) modified the minimum number of ANC visits from four to at least eight visits,2 with the first visit to be made within the first 12 weeks of gestation. In the Ethiopian context, the Federal Ministry of Health recommends the first ANC visit to be undertaken within 12 weeks but not later than 16 weeks of pregnancy.6
Early ANC registration maximizes the window of opportunity for health care providers to counsel mothers to opt for institutional delivery.2 It also improves the likelihood of identifying pregnancy-related complications, such as pre-eclampsia, gestational diabetes, sexually transmitted infections (example, Human Immuno-Virus, and syphilis), or anemia. Early identification of pregnancy-related complications, in turn, creates opportunities for improved management of such problems, leading to better maternal and neonatal health outcomes.7,8
Given that the organogenesis of the fetus occurs during the first trimester of pregnancy,2 early attendance of ANC provides a better hemoglobin concentration through timely provision of iron and folic acid supplements, nutritional counseling, prevention, and early treatment of malaria and hookworm.8,9 Indeed, the effect of folic acid in reducing the risks of neural tube defects will be effective when it is provided during early pregnancy or if possible before pregnancy begins.9
Since the last two decades Ethiopia has developed a number of programs to carry out initiatives for safe motherhood. In 2003, for example, the country launched the Health Extension Program to address maternal and child health problems, to achieve improvement in communicable diseases, hygiene and sanitation, and healthcare-seeking behavior of people.10 Since then, more than 38,000 community-based health cadres, named Health Extension Workers (HEWs), have been trained and deployed in rural communities of the country to improve access to and utilization of health care particularly for children and mothers.10,11 The HEWs are trained on how to provide care to pregnant women before and during pregnancy, at birth and post-partum periods.10,12
However, despite the improvements gained in maternal service accessibility, still, the time pregnant women receive their first ANC is a well-recognized challenge in the provision of quality ANC service in Ethiopia.13 Still, too many women tend to wait to start ANC until the second or even the third trimester with the pregnancy,4,14 already compromised or at risk from HIV,15 hepatitis B virus,15,16 malaria,15,16 syphilis,15 anemia,15 and asymptomatic genitourinary tract infections.15 In Ethiopia, 26% of pregnant women started their ANC visits during the fourth to the fifth month of pregnancy. The median duration of pregnancy at the first visit was 4.7 months. Urban women made their first ANC visit earlier (4.0 months) than rural women (4.9 months).4 Therefore, to improve the rate of early ANC visit factors influencing women’s service utilization need to be identified.17
It has been evidenced that maternal health care utilization is not simply a matter of access; a range of factors operating on the individual, household, and community levels13,18 can influence the quality of maternal health services. As such, a better understanding of factors associated with the facility structure and neighborhood ecology could help to design context-based intervention strategies. However, the previous studies in Ethiopia so far have emphasized the influences of individual characteristics while little attention has been given to the community-related factors and service delivery environment.
Therefore, in this study, we aimed to bridge the gaps by accounting for individual- and community-level factors associated with late initiation of antenatal care by using multilevel modeling.
Methods
Study Design and Setting
This was a community-based cross-sectional study linked with health facility data. The study was carried out in five districts of West Gojjam Zone, Northwest Ethiopia. Administratively the zone had 13 rural districts and 2 town administrations with a projected population of 2,611,925 people with women of reproductive age (15–49) making 23.58% of the population.19
The zone had 6 governmental hospitals, 103 health centers, and 374 health posts during the time of the survey. Also, it had 115 private health facilities (1 general hospital and 114 clinics). All maternal and reproductive health services including family planning, antenatal care, labor and delivery, postnatal, and abortion services were provided free of charge in public health facilities.19
Study Population and Sampling
The study-involved women of reproductive age (15–49 years) who gave birth during the last 12 months preceding the study. This study was part of a large study done on the continuum of maternal health care with multiple objectives, and the detail of sample size calculation and sampling procedure is described elsewhere.20 Of the different sample sizes computed, the largest sample size (1294 women) was obtained by considering the following assumptions; 95% confidence level, 4% margin of error, 16.5% proportion of PNC utilization,12 design effect of 2, and 10% non-response rate. However, in the current study, we were interested in the timing of the first antenatal visit among women during their last pregnancy. Therefore, the sample was restricted to the 898 women who made at least one antenatal care visit.
Variables and Measurement
Outcome
The outcome variable was the timing of the first ANC visit (early vs delay). The variable was coded “1” if the woman started her first ANC visit at or after 16 weeks of pregnancy, and “0” if started before 16 weeks.
Independent Variables
The explanatory variables were organized into two hierarchical levels: Characteristics of the women and household factors were considered as individual-level (level-1) predictors whilst characteristics of the community and facilities were taken as group level (level-2) predictors.
The individual-level variables considered in this study were women’s age at last birth, education of women and husbands, maternal and paternal occupation, household wealth index, parity, number of living children, birth order, and intention of last pregnancy. Besides, the following community-level factors were considered: residence, health facility density, and average distance to the average health facility.
Data Collection
The data were collected using a structured pretested questionnaire through a house-to-house visit. The tool was initially prepared in English and later translated to Amharic, the official working language in the region. Twenty data collectors and supervisors, organized in five teams, collected the data. The data collectors and supervisors received two days of intensive training. Further, the readiness of health facilities to support the provision of antenatal care has been evaluated using the World Health Organization’s criteria.21 Then, the result of each facilities’ readiness score was linked to the individual woman in the corresponding household survey.
Data Processing and Analysis
The collected data were checked visually, coded, and entered into EPI info version 7 and exported to SPSS version 25 for analysis. Then, the data were screened for errors, missing values, and outliers. After the screening, descriptive statistics were applied to calculate the frequency distribution and proportions for categorical variables. For the normally distributed continuous variables, mean with standard deviations was also computed.
Due to the multistage cluster sampling, individuals living in the same kebele (the smallest administrative unit in Ethiopia) were expected to share similar characteristics than those from other kebeles. Hence, some of the inherent assumptions underlying the traditional regression modeling, including the assumption of independence among women within the same kebele and that of equal variance across kebeles would not be valid.22
Therefore, by considering the hierarchical structure of our data and the dichotomous nature of the variable of interest, a two-level random intercept logistic regression has been performed under two different sets of models. In the first model (null model), no independent variables were included to determine whether our data justified the decision to assess random effects at level 2 (ie at kebele level) or not. The second model is a full model that included both the individual- and community-level variables.
The bivariate and multivariable analysis techniques were applied to check the association of selected independent variables with the timing of ANC visit. Accordingly, the independent variables to be included in the multivariable model were selected when the p-value was <0.2 in the bivariate analysis. The following equation was used to explain the multilevel model:-
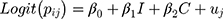
where Pij is the probability of late initiation of the first ANC for women ith in the kebele jth. The coefficients β0 and β’s are the regression parameters of the models referring to random intercept and slopes corresponding to the explanatory variables, respectively. The letters “I” and “C” refer to level 1 and level 2 variables, respectively; and uj represents the random effect at level 2 representing the effect of jth kebele on the outcome variable.
The results of fixed effects (measures of association) are presented as odds ratios (ORs) and 95% CIs, while the random effects (measures of variation) were reported as variance, intra-class correlation coefficient (ICC), and median odds ratio (MOR).23 The ICC is calculated as:
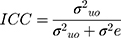
Where:  and
and  are cluster (kebele) and individual-level variances, respectively. In the logistic regression, the distribution of level-1 residual variance is standardized and fixed with mean 0 and variance π2/3 ≈ 3.29.24 The median odds ratio (MOR) was calculated to provide a clearer interpretation of cluster-level variance. The MOR is defined as the median value of a set of odds ratios between the clusters at the highest and the lowest risks when randomly picking out two clusters,25 which is the Increased risk (in median) that one would have if moving to a cluster with a higher risk of late ANC visit. MOR was computed as follows:
are cluster (kebele) and individual-level variances, respectively. In the logistic regression, the distribution of level-1 residual variance is standardized and fixed with mean 0 and variance π2/3 ≈ 3.29.24 The median odds ratio (MOR) was calculated to provide a clearer interpretation of cluster-level variance. The MOR is defined as the median value of a set of odds ratios between the clusters at the highest and the lowest risks when randomly picking out two clusters,25 which is the Increased risk (in median) that one would have if moving to a cluster with a higher risk of late ANC visit. MOR was computed as follows:
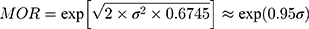
where  is the cluster-level variance and 0.6745 the 75th centile of the cumulative distribution function of the normal distribution with mean 0 and variance 1.
is the cluster-level variance and 0.6745 the 75th centile of the cumulative distribution function of the normal distribution with mean 0 and variance 1.
Moreover, multi-collinearity among the explanatory variables was checked using Variance Inflation Factors (VI Fs).
Ethics and Consent
This study was conducted in accordance with the Declaration of Helsinki. The study received ethical approval from the Ethical Review Board (IRB) of Bahir Dar University (protocol no: 087/18-04). A formal letter of permission was granted from the Amhara Regional Health Bureau and line offices. All the study participants were informed about the purpose of the study, their right to refuse and assurance of confidentiality. All participants gave written informed consent. Since our study did not have any invasive procedure; we did not take consent from parent or legal guardian. We rather took consent from the women themselves. The consent process was acceptable and approved by the IRB. The ethical guideline of Ethiopia also allows us to take consent from adolescent mothers if she is above age 15, but only in case of noninvasive procedures. Privacy and confidentiality were strictly maintained throughout the study.
Results
Background Characteristics
The mean age of the participants was 29.45 (standard deviation of ±5.61) years. Approximately 19% of pregnant women were within the age range of 15–24 years. Over 54% of women had no education; 46.1% fell in the poorest wealth category, and 638 (70.7%) of them were from rural areas.
The proportion of respondents who made their first ANC visit within the recommended time (before 16 weeks of gestation) was 194 (21.6%). The mean gestational age at first ANC visit was 5.25 months (SD ±1.42 months). The timing of first ANC attendance ranged from the 1st to 9th month during pregnancy.
The likelihood of having had an ANC checkup in the first 4 months increased with increasing levels of women’s education, from 11.0% for those who had never attended school to 58.3% for those with secondary and higher-level education. Urban women were almost three times (40.3%) more likely to initiate their first ANC visit at or after 4 months of gestation as compared to rural women (13.9%). Women aged 15–24 years (30.5%) had booked early for their first visits compared to other age groups. Likewise, women of first birth order (33.0%), and those women who live near to the health facility (23.0%) had a higher percentage of visits early in the course of pregnancy (Table 1).
Multilevel Analysis
As stated in the Methods section we estimated two random intercept models. Model 1was an empty model with no predicting variables and model 2 was a random intercept model (full model) with individual- and community-level variables included simultaneously.
As a first step, we examined whether our data support the decision to assess random effects at the cluster and individual levels. Hence, we started with an empty model to test the null hypothesis that there is no variation in the effects of timing of the first ANC visit between clusters, the results of which show significant variation (p=0.042) across clusters (kebeles). This suggests that adding between-cluster variance in the model was necessary to detect the effect of timing of the first ANC visit among pregnant women.
The results from the MOR (3.68) of the null model also confirmed that late ANC registration was attributed to community-level factors. Furthermore, the calculated intra-class correlation coefficient (ICC) value of 28.6% in the empty model indicated that the variability in the late ANC visit was accounted for by clusters, leaving the remaining 71.4% of the variability to be accounted for by characteristics of the women and households, or other unmeasured factors (Table 2). Therefore, our analysis was based on the random effect model that takes the effects of clustering into account.
 |
Table 2 Results of the Random Intercept Model (Measures of Variation) for Late ANC Initiation at Cluster Level by the Two-Level Logistic Regression Analysis, Northwest Ethiopia, June 2018 |
As presented in Table 3, the result from the multilevel analysis revealed notable inequalities in the late initiation of ANC in the study area. At the individual level, the educational status of the women, intendedness of the last pregnancy, and the levels of knowledge of women about the timing of first ANC visit and danger signs of pregnancy were statistically associated with late ANC commencement. The educational level of women was inversely associated with late initiation of ANC. Women with no formal education (AOR=4.08, 95% CI: 2.20, 7.55), and women who completed primary education (AOR=2.49, 95% CI: 1.44, 4.31) were more likely to delay their first ANC visit compared to those who attended secondary and higher education. However, women with intended pregnancy were 51% less likely to book late for their first ANC (AOR= 0.31; 95% CI: 0.12, 0.79) as compared to their counterparts of women with a planned pregnancy.
 |
Table 3 Multilevel Logistic Regression of the Timing of First ANC Visit Among Pregnant Women in West Gojjam Zone, Northwest Ethiopia, 2018 (n=898) |
Participants were also asked if they knew when ANC visits would be started and about the danger signs of pregnancy. Accordingly, we found a statistically significant decrease in the odds of late ANC registration when women were knowledgeable on the ANC registration and danger signs of pregnancy. In this regard, women who were knowledgeable on ANC timing (AOR= 0.43; 95% CI: 0.25, 0.75), and pregnancy-related complications (AOR= 0.16; 95% CI: 0.10, 0.26) were less likely to delay their ANC visit as compared to their counterparts.
For the most part, the cluster-level factors included in this study, however, were not significantly related to the timing of the first ANC registration. The one exception, here, is the average distance to the nearest health facility. A one-kilometer increase in the average distance to the nearest facility providing comprehensive ANC services was associated with a 4% increase in the odds of having late ANC visit.
Finally, after adjusting for the individual- and community-level factors in the full model, the results of random effect revealed that the between-cluster variation for the delay in the first ANC visit was decreased marginally from 1.316 to 1.185, which is about a 10% reduction in the unexplained variance between clusters. The data further showed that the value of MOR reduced from 3.68 to only 3.44 (Table 2).
Discussion
Our study examined the timing of the first antenatal care visit and inequalities in the initiation of ANC visit in a predominantly rural area of Ethiopia where access to a health facility was relatively deficient.
Early initiation and frequent ANC attendance improve the health of mothers and the growing fetus.2 The federal ministry of health of Ethiopia recommends all pregnant women to start their antenatal care in the first trimester but not later than four months of gestation.6 However, in this study, we found out that only 21.6% (95% CI: 19.0–24.4%) of the women began their first ANC visit at or after four months of pregnancy. The finding is in line with studies conducted in other parts of Ethiopia, where a significant proportion of pregnant women do not start ANC timely.26,27
The delay in ANC visit might be attributed to social gradients surrounding pregnancy and the birth process.28 Many Ethiopian women traditionally enjoy little independent decision making on most reproductive health matters; and hence health facility visit requires the approval of husbands, mothers-in-law, and other senior family members.29–31 Delayed in the initiation of ANC imply that still many pregnant women miss the opportunity to early receive various health promotion services and timely detection of pregnancy-related complications.
The fixed effect of the multilevel analysis revealed that women who attended primary or above level of education were less likely to delay their first ANC visit as compared to women without formal education. This finding is in agreement with the previous studies,13,27,32 in which the authors argued that education might have brought increased knowledge and awareness of health services in general and the benefits of early ANC visits in particular. It has also been evidenced that better education improves the self-worth and authority of women, their negotiating skills with husbands or other health deceives, leading to women’s ability to demand quality and timely maternal services.13,27
Evidence shows that well-informed women are more likely to make judicious choices about the proper utilization of ANC including its timing.13 In line with the previous researches,13,32,33 the result of our study also found a statistically significant decrease in the odds of late ANC registration among pregnant women who were aware of issues related to ANC, pregnancy risks, and danger signs of pregnancy compared to those who had insufficient knowledge. Since a large number of Ethiopian women considered pregnancy as a natural process, they are reluctant to visit facilities when they perceived no risk to their well-being and warrant ANC only when problems arise.18 In this regard, Dutamo and his colleagues34 stated that pregnancy in Ethiopia is often viewed as a normal life event socially contingent, rather than a medical condition requiring professional monitoring and supervision.
This study also revealed that pregnancy intention was the other strong predictor of late ANC visit. Women with intended pregnancy were 69% less likely to book late for their first ANC as compared to their counterparts with an unplanned pregnancy. This was supported by other studies as well.32,35,36 In this aspect, Yohannes et al36 from Ethiopia identified that a large number of women with unintended pregnancy go through a period of denial as many of them were too young or too old. Further, Shrestha et al37 in Gambia found that pregnant women delayed their first ANC visit as late as in the third trimester, mainly because they chose to keep their pregnancy secret until neighbors notice it.
Empirically, distance is identified as a structural barrier preventing women from seeking maternal services.36 In this study, we also found that the average distance to the nearest health facility was the only second-level factor associated with the timing of antenatal care. A one-kilometer increase in the average distance to the nearest health facility providing ANC services was associated with a 4% increase in the odds of having late ANC visits, which is an indicator of service inequity for those mothers located on the margins of the society. In Ethiopia, health facilities are disproportionately distributed in favor of urban residents.38 As a result, it is not uncommon to see them transported along difficult roads using locally prepared stretchers, carried on the shoulder of persons. Also, a large proportion of rural residents believe that pregnancy is a natural process requiring no medical intervention.39
After adjusting for the individual- and community-level factors, the between-cluster variation for late ANC visit decreased marginally from 1.316 to 1.185, which is about a 10-% reduction in the unexplained variance between clusters. The data further showed that the value of MOR in the final model was reduced from 3.68 to 3.44. The figures suggest that there is still a considerable proportion of between-cluster variation that is not explained by the modeled predicting variables24 though the result turned statistically insignificant.
Despite the important findings evolved in the present study, the data suffered from some limitations that should be noted. First, as in other cross-sectional studies, the study design could not allow drawing causal inferences. Second, social desirability bias might also be a concern in cases that women feel they need to respond in a way expected of them. Third, we acknowledge recall bias as possible limitations as data from women were based on their memories. In relation to this, measurement of the gestational age might be inaccurate as we merely relied on women’s self-reported information of their last menstrual period. However, to minimize recall bias, the period in this study was limited to one year.
Therefore, further prospective cohort studies are required to ensure the reliability of the results and to represent the actual proportion of women concerning the timing of the first antenatal care visit.
Conclusions
Even if Ethiopian women have the right to access antenatal care free of charge in all public health facilities, the finding showed that the magnitude of delayed initiation of ANC was very high. This study brings out several determining factors for the timing of the first antenatal care visit concerning the individual-level characteristics, household-level factors, service delivery environment, and contextual-level factors.
Measures for enhancing early antenatal visit should focus on addressing hindrances in accessing care, particularly among geographically disadvantaged and non-educated women. Furthermore, the observed heterogeneity at the cluster-level can provide information for policymakers and program planners to look beyond individual factors when designing strategies to improve the health-seeking behavior of pregnant women.
Authors’ Information
AAE is an assistant professor and a Ph.D. candidate in the department of reproductive health and Population Studies, Bahir Dar University, Ethiopia; GDA is a Professor in the department of epidemiology and Biostatistics, Bahir Dar University, Ethiopia; and GTD is an associate professor in the Department of Population and Family Health, Jimma University, Ethiopia.
Abbreviations
ANC, antenatal care; AOR, adjusted odds ratio; COR, crude odds ratio; MOR, median odds ratio; WHO, World Health Organization.
Data Sharing Statement
The authors confirm that all the data supporting the findings of this study are available within the article.
Acknowledgments
The authors would like to thank Bahir Dar University for providing financial support. We would like to thank the Amhara regional health bureau, West Gojjam Zone Health Department, and district health offices for their unreserved supports. We also extend our acknowledgment to the data collectors, supervisors, and study participants.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest.
References
1. Desa U Transforming our world: the 2030 agenda for sustainable development. 2016.
2. World Health Organization. WHO Recommendation on Antenatal Care for Positive Pregnancy Experience. Geneva: WHO; 2016.
3. World Health Organization. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF. UNFPA, World Bank Group and the United Nations Population Division; 2019.
4. Central Statistical Agency (CSA) [Ethiopia] and ICF. 2016 Ethiopia Demographic and Health Survey Key Findings. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2017.
5. Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–e33. doi:10.1016/S2214-109X(14)70227-X
6. Ethiopian Federal Ministry of Health. Antenatal care module: 13. providing focused antenatal care. Available from: https://www.open.edu/openlearncreate/mod/oucontent/view.php?id=44&printable=1.
7. Heredia-Pi I, Servan-Mori E, Darney BG, Reyes-Morales H, Lozano R. Measuring the adequacy of antenatal health care: a national cross-sectional study in Mexico. Bull World Health Organ. 2016;94(6):452–461. doi:10.2471/BLT.15.168302
8. Sinyange N, Sitali L, Jacobs C, Musonda P, Michelo C. Factors associated with late antenatal care booking: population based observations from the 2007 Zambia demographic and health survey. Pan Afr Med J. 2016;25. doi:10.11604/pamj.2016.25.109.6873
9. Roth C, Magnus P, Schjølberg S, et al. Folic acid supplements in pregnancy and severe language delay in children. JAMA. 2011;306(14):1566–1573. doi:10.1001/jama.2011.1433
10. Federal Ministry of Health (FMOH).Health Sector Transformation Plan (HSTP): 2015/16–2019/20 (2008–2012 EFY) Addis Ababa, Ethiopia; October 2015. Available from: https://www.globalfinancingfacility.org/sites/gff_new/files/Ethiopia-health-system-transformation-plan.pdf.
11. Wang H, Tesfaye R, NV Ramana G, Chekagn CT. Ethiopia Health Extension Program: An Institutionalized Community Approach for Universal Health Coverage. The World Bank; 2016.
12. Medhanyie A, Spigt M, Kifle Y, et al. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res. 2012;12(1):352. doi:10.1186/1472-6963-12-352
13. Tesfaye G, Loxton D, Chojenta C, Semahegn A, Smith R. Delayed initiation of antenatal care and associated factors in Ethiopia: a systematic review and meta-analysis. Reprod Health. 2017;14(1):150. doi:10.1186/s12978-017-0412-4
14. Alemu Y, Aragaw A. Early initiations of first antenatal care visit and associated factor among mothers who gave birth in the last six months preceding birth in Bahir Dar Zuria Woreda North West Ethiopia. Reprod Health. 2018;15(1):203. doi:10.1186/s12978-018-0646-9
15. Deme C, Edao B, Jaya G, et al. Prevalence of hypertension, anemia, asymptomatic urinary tract infection, syphilis, HIV and hepatitis B virus infection among pregnant women attending an antenatal clinic at a rural hospital in Southern Ethiopia. Southeast Asian J Trop Med Public Health. 2016;47(5):1032–1039.
16. Helegbe GK, Aryee PA, Mohammed BS, et al. Seroprevalence of malaria and hepatitis B coinfection among pregnant women in tamale metropolis of Ghana: a cross-sectional study. Can J Infect Dis Med Microbiol. 2018;2018.
17. Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387(10017):462–474. doi:10.1016/S0140-6736(15)00838-7
18. Kea AZ, Tulloch O, Datiko DG, Theobald S, Kok MC. Exploring barriers to the use of formal maternal health services and priority areas for action in Sidama zone, southern Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):96. doi:10.1186/s12884-018-1721-5
19. ANRS Health Burea. The 2016/17 Fiscal Year Annual performance report of Amhara regional state health bureau. Bahir Dar July, 2017.
20. Emiru AA, Alene GD, Debelew GT, Navaneetham K. The role of maternal health care services as predictors of time to modern contraceptive use after childbirth in Northwest Ethiopia: application of the shared frailty survival analysis. PLoS One. 2020;15(2):e0228678. doi:10.1371/journal.pone.0228678
21. World Health Organization. Service Availability and Readiness Assessment (SARA): An Annual Monitoring System for Service Delivery: Reference Manual. World Health Organization; 2013.
22. Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Sage; 2002.
23. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012
24. Tom A, Bosker TASRJ, Bosker RJ. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. Sage; 1999.
25. Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60(4):290–297. doi:10.1136/jech.2004.029454
26. Geta MB, Yallew WW. Early initiation of antenatal care and factors associated with early antenatal care initiation at health facilities in southern Ethiopia. Adv Public Health. 2017;2017.
27. Gebresilassie B, Belete T, Tilahun W, Berhane B, Gebresilassie S. Timing of first antenatal care attendance and associated factors among pregnant women in public health institutions of Axum town, Tigray, Ethiopia, 2017: a mixed design study. BMC Pregnancy Childbirth. 2019;19(1):340. doi:10.1186/s12884-019-2490-5
28. Finlayson K, Downe S, Daniels K. Why do women not use antenatal services in low-and middle-income countries? A meta-synthesis of qualitative studies. PLoS Med. 2013;10(1):e1001373. doi:10.1371/journal.pmed.1001373
29. Woldemicael G, Tenkorang EY. Women’s autonomy and maternal health-seeking behavior in Ethiopia. Matern Child Health J. 2010;14(6):988–998. doi:10.1007/s10995-009-0535-5
30. Biratu BT, Lindstrom DP. The influence of husbands’ approval on women’s use of prenatal care: results from Yirgalem and Jimma towns, south west Ethiopia. Ethiop J Health Dev. 2006;20(2):84–92.
31. Bogale B, Wondafrash M, Tilahun T, Girma E. Married women’s decision making power on modern contraceptive use in urban and rural southern Ethiopia. BMC Public Health. 2011;11(1):342. doi:10.1186/1471-2458-11-342
32. Ewunetie AA, Munea AM, Meselu BT, Simeneh MM, Meteku BT. DELAY on first antenatal care visit and its associated factors among pregnant women in public health facilities of Debre Markos town, North West Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):173. doi:10.1186/s12884-018-1748-7
33. Belayneh T, Adefris M, Andargie G. Previous early antenatal service utilization improves timely booking: cross-sectional study at university of Gondar hospital, northwest Ethiopia. J Pregnancy. 2014;2014.
34. Dutamo Z, Assefa N, Egata G. Maternal health care use among married women in Hossaina, Ethiopia. BMC Health Serv Res. 2015;15(1):365. doi:10.1186/s12913-015-1047-1
35. Gebremeskel F, Dibaba Y, Admassu B. Timing of first antenatal care attendance and associated factors among pregnant women in Arba Minch Town and Arba Minch District, Gamo Gofa Zone, South Ethiopia. J Environ Public Health. 2015;2015.
36. Wado YD, Afework MF, Hindin MJ. Unintended pregnancies and the use of maternal health services in southwestern Ethiopia. BMC Int Health Hum Rights. 2013;13(1):36. doi:10.1186/1472-698X-13-36
37. Shrestha SK, Travaglia J, Joshi C. A narrative synthesis of the published literature on antenatal care in low and middle income countries. Health Prospect. 2014;13(1):12–23. doi:10.3126/hprospect.v13i1.11341
38. Berhan Y, Berhan A. Commentary: reasons for persistently high maternal and perinatal mortalities in Ethiopia: part III–perspective of the “three delays” model. Ethiop J Health Sci. 2014;24:137–148. doi:10.4314/ejhs.v24i0.12S
39. Bobo FT, Yesuf EA, Woldie M. Inequities in utilization of reproductive and maternal health services in Ethiopia. Int J Equity Health. 2017;16(1):105. doi:10.1186/s12939-017-0602-2
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

