Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Indices of iron homeostasis correlate with airway obstruction in an NHANES III cohort
Authors Ghio AJ, Hilborn ED
Received 31 March 2017
Accepted for publication 19 June 2017
Published 18 July 2017 Volume 2017:12 Pages 2075—2084
DOI https://doi.org/10.2147/COPD.S138457
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Andrew J Ghio, Elizabeth D Hilborn
Environmental Public Health Division, National Health and Environmental Effects Research Laboratory, Chapel Hill, NC, USA
Abstract: Cigarette smoking results in the accumulation of iron both systemically and locally, in the lung thereby causing imbalance in iron homeostasis. This disruption in iron homeostasis can be associated with oxidative stress and consequent tissue injury. Therefore, in this study, we tested the association between iron homeostasis and airway obstruction by examining a large cohort of smokers and non-smokers for relationships between 1) serum ferritin and iron concentrations and transferrin saturation and 2) forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), and their ratio (FEV1/FVC). Data from the National Health and Examination Survey III were analyzed. The study population included persons aged 20 years and above with their following data recorded: race, gender, serum ferritin and iron concentrations, and transferrin saturation; the final sample number was 7,251. In the total population, Pearson correlation coefficients between 1) serum ferritin and iron concentrations and transferrin saturation and 2) FVC and FEV1 were significantly positive; whereas those between 1) serum ferritin concentrations and transferrin saturation and 2) FEV1/FVC were significantly negative. With separate analyses, serum ferritin concentrations demonstrated positive associations with FVC and FEV1 but an inverse relationship with FEV1/FVC in smokers and non-smokers. Serum ferritin levels increased with worsening airway obstruction among smokers, and its highest concentrations were found among those with the lowest values of FEV1/FVC ratio (<60%). Comparable to cigarette smokers, serum ferritin concentrations among non-smokers were greatest in those with the lowest FEV1/FVC ratio. Furthermore, elevated levels of serum iron and saturation of transferrin also corresponded with decreased FEV1/FVC ratio among non-smokers. Thus, we conclude that indices of iron homeostasis are associated with airway obstruction in both smokers and non-smokers.
Keywords: iron, ferritins, respiratory function tests, chronic obstructive pulmonary disease, spirometry, vital capacity, forced expiratory volume
Introduction
Smoking a single cigarette exposes the human respiratory tract to high levels of particulate matter (PM) (between 15,000 and 40,000 μg PM).1 PM is deposited in the human lung at a high rate.2 Furthermore, incomplete oxidation of tobacco leaves produces oxygen-containing functional groups (eg, carboxylates, esters, and phenolic hydroxides) at the surface of the retained cigarette smoke particles.2 Following dissociation of proton at physiological pH level, the aforementioned functional groups introduce a negatively charged solid–liquid interface into the lung tissue. Furthermore, Fe3+ has a high affinity toward oxygen-donor ligands due to its electropositivity, and thus, it forms complexes with the PM deposited from cigarette smoke.3 Subsequently, these complexes accumulate on the surface of the lungs of smokers.4 However, elevated iron concentrations are observed not only in the lower respiratory tract but systemically as well.4,5 Reflecting this disruption in the homeostasis of iron and its accumulation, serum concentrations of ferritin, a metal storage protein, and iron concentrations increase in cigarette smokers.5 Similarly, saturation of transferrin, an iron transport protein, is elevated in the serum of smokers.5 The disruption in iron homeostasis in smokers can be associated with oxidative stress, which triggers a cascade of biochemical events culminating in inflammation, fibrosis, and cancer, both locally in the lungs and systemically.
COPD most frequently refers to the combination of chronic bronchitis and emphysema, a pair of commonly co-existing lung diseases in which the airways become functionally narrowed. The vast majority of COPD in the United States is the result of cigarette smoking. A fundamental characteristic of COPD is the physiological limitation of the expiratory flow of air from the lungs, which is irreversible. One of the best indicators of airflow obstruction is the ratio of forced expiratory volume in 1 s (FEV1) to forced vital capacity (FVC).6 The natural course of COPD is characterized by a gradual worsening of obstruction (ie, FEV1/FVC ratio decreases) over years with exacerbations of airflow obstruction caused by infections and air pollution.
Disruption in iron homeostasis with the subsequent accumulation of this metal has been proposed to contribute to COPD.7,8 If metal-associated biological effects (eg, oxidative stress) contribute to lung injury following smoking, an accumulation of iron following cigarette smoking should correlate with physiological indices of damage. Therefore, in this study, we evaluated the association between iron homeostasis and airway obstruction by examining a large cohort of both smokers and non-smokers for relationships between 1) serum concentrations of ferritin and iron and transferrin saturation and 2) FVC, FEV1, and their ratio (FEV1/FVC).
Materials and methods
Study population
Data from the National Health and Nutrition Examination Survey III (NHANES III, conducted 1988 to 1994) were analyzed. The study population included persons aged 20 years and above with their following data recorded: race, gender, serum ferritin and iron concentrations, serum transferrin saturation, and serum C-reactive protein. Of the 13,941 persons initially selected, 2,944 were excluded as they reported a respiratory infection at either the time of or within 3 weeks prior to the interview. Individuals were categorized as either “smoker” or “non-smoker”. A smoker was defined as a person who reported smoking cigarettes for at least 1 year duration at the time of interview. A non-smoker was defined as a person who reported smoking less than 100 cigarettes during their lifetime, and whose serum cotinine concentration was less than 1.0 ng/mL. Records of 3,746 persons who did not fit the definitions of “smoker” and “non-smoker” were eliminated from the database for a final sample size of 7,251 individuals.
Blood indices and pulmonary function tests
Measurements of blood endpoints and pulmonary function indices are provided in detail.9
Data analysis
Analyses were performed using SAS and WesVar statistical software (SAS Institute, Inc., Cary, NC, USA and Westat, Rockville, MD, USA, respectively) enabling weighting and adjustment for the survey sampling methodology in estimating variances during the final analysis. Data analysis was performed to explore variable distributions and correlations. Geometric means and standard errors (SE) of FVC, FEV1, FEV1/FVC ratio, serum concentrations of ferritin and iron, transferrin saturation, and serum levels of C-reactive protein are reported. Age categories of 10 year increments were created; results are described by the first year of age in each category. Pearson product-moment correlation coefficients were calculated. Tests were two-sided. Significance was set at P<0.05.
Results
Demographic characteristics of the study population, smoking status, and FEV1/FVC values are provided in Table 1. There were 2,549 (35%) smokers and 4,702 (65%) non-smokers. Forty-nine percent of the cohort was between 20 and 39 years of age and only 13% was above the age 70 years.
  | Table 1 Characterization of the study population |
In the study population, serum ferritin and iron concentrations, transferrin saturation, and C-reactive protein levels had means (± SE) of 73.8±1.7 ng/mL (166±4 pmol/L), 80.4±0.6 μg/dL (14.4±0.1 μmol/L), 22.9%±0.2%, and 0.31±0.01 mg/dL (30±1 nmol/L), respectively. The log-transformed values of serum ferritin and iron concentrations and transferrin saturation more closely approximated a normal distribution than the original values. The distribution of serum C-reactive protein levels was highly skewed with greater than 50% of the subjects having values below the limit of detection. For correlation analysis, both absolute and log-transformed values of serum ferritin, iron, transferrin saturation, and C-reactive protein were used. The mean (±SE) for the FVC, FEV1, and FEV1/FVC ratio were 3.582±0.029 L, 2.834±0.025 L, and 0.790%±0.002%, respectively. FEV1, FVC, and FEV1/FVC ratio were normally distributed.
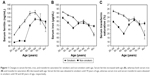
Absolute values of serum ferritin and iron concentrations and transferrin saturation for smokers and non-smokers were plotted against age (Figure 1). The concentration of serum ferritin increased with age, whereas the concentration of serum iron generally decreased. Relative to non-smokers, serum ferritin concentration was found to be increased among smokers in the age group of 70 years, after which it declined; serum concentrations among non-smokers were significantly higher than that of smokers in the age group of 80 years. Similarly, serum iron concentrations and serum transferrin were elevated among smokers until the age of 50 and 60 years, respectively, at which times, serum concentrations in non-smokers were comparable, although all serum concentrations of iron were higher among non-smokers after the age of 70 years.
Pearson correlations between age, indices of iron homeostasis, serum C-reactive protein levels, and pulmonary function parameters reveal significant correlations among all in the study population, among smokers and among non-smokers (Tables 2–4). Age was correlated with all endpoints of iron homeostasis and pulmonary function except ln serum transferrin saturation among non-smokers. Serum ferritin concentrations were positively associated with age, whereas serum iron concentrations and serum transferrin saturation were negatively associated with age. All pulmonary function parameters decreased with age. Serum iron concentrations and transferrin saturation showed stronger positive correlations with both FVC and FEV1 than that of serum ferritin concentrations; the same pattern was evident with FEV1, but the relationship with serum ferritin did not reach significance in non-smokers. In contrast, serum ferritin had the greatest correlation with FEV1/FVC but was negative. Ln serum C reactive protein levels correlated negatively with FVC, FEV1, and FEV1/FVC ratio among smokers and negatively with FVC and FEV1 among non-smokers.
Higher serum ferritin concentrations were observed among smokers with airway obstruction. There were significant differences in serum ferritin concentrations between smokers with airway obstruction with FEV1/FVC ≥75%, FEV1/FVC between 60% and 74%, and those with FEV1/FVC <60% (Figure 2A). The greatest concentrations of this iron-storage protein were among those with the lowest values of FEV1/FVC (<60%). In contrast, there were no significant differences in either serum iron concentration or transferrin saturation among smokers with FEV1/FVC >75%, between 60 and 74%, and <60% (Figure 2B and C, respectively). However, all three indices of systemic iron homeostasis (ie, serum ferritin, serum iron, and transferrin saturation) showed significant differences among non-smokers with FEV1/FVC ≥75%, between 60 and 74%, and <60% (Figure 2A–C). Similar to the cigarette smokers, serum ferritin concentrations were greatest among non-smokers with the lowest values of FEV1/FVC (ie, the worst airway obstruction). Elevated concentrations of serum iron in non-smokers were found with decreasing FEV1/FVC. Finally, serum transferrin saturation among non-smokers increased with worsening airway obstruction.
The effect of inflammation on airway obstruction was gauged using serum concentrations of C-reactive protein. Among smokers, those individuals with the greatest airway obstruction (FEV1/FVC <60%) demonstrated a higher level of C-reactive protein than those with FEV1/FVC between 60 and 74% or >75% (Figure 3). There was no significantly different relationship between C-reactive protein and FEV1/FVC among non-smokers (Figure 3).
Discussion
In an NHANES III cohort, serum indices of iron homeostasis differed by age and were dissimilar between smokers and non-smokers. Serum ferritin concentrations have been repeatedly demonstrated to increase with age comparable to other measures of total body stores of iron;10,11 the exception to this is the first six months of life when iron stores are utilized and depleted by the newborn child.12 Similar to age, race can impact serum ferritin concentrations with individuals of black race consistently have elevated values relative to Caucasians.13 However, the factor which has the greatest impact on serum ferritin concentrations and stores of iron is gender, with males having significantly greater values than females throughout their adult lives.14 This investigation again demonstrated an association between cigarette smoking and serum ferritin with elevated concentrations among current smokers.5 The relationship between serum ferritin and smoking supports the concept that cigarette smoking disrupts iron homeostasis and is associated with metal accumulation. Among smokers, levels of iron increase both systemically and locally in the lung (eg, concentrations in both alveolar macrophages and lavage fluid).15–18 The elevated levels of serum ferritin in smokers reflect increased concentrations of total body iron. In this investigation, serum iron concentrations and transferrin saturation decreased with age but were elevated among smokers until 50 and 60 years of age, respectively.
Results support a negative relationship between FEV1/FVC ratio and serum ferritin among the entire study population, smokers, and non-smokers and between FEV1/FVC and transferrin saturation among the entire population and non-smokers. This is comparable to prior investigation which demonstrated that serum ferritin concentration negatively correlated with the FEV1/FVC ratio reflecting a positive association of the metal storage protein with airway obstruction.19 Studies have also demonstrated that FVC and FEV1 can correlate positively with serum ferritin and iron concentrations and transferrin saturation.20–22 The disruption in iron homeostasis with cigarette smoking can be associated with oxidative stress, and this can initiate pathways resulting in COPD. However, indices of iron homeostasis were also associated with COPD in non-smokers. Etiologies of irreversible airway obstruction in non-smokers can include occupational exposures to particles (eg, miners, tunnel workers, and concrete workers and air pollution).23,24 The basic mechanism of the biological effect of such particles is the same as that of cigarette smoke particles, that is, they also disrupt iron homeostasis resulting in an accumulation of iron with an oxidative stress and injury ensuing.25 Accordingly, it is anticipated that FEV1/FVC ratio will also decrease with particle exposures other than those associated with cigarette smoke and contribute to airway obstruction in non-smokers. FEV1/FVC in non-smokers decreased not only with elevations in serum ferritin but also with increased levels of serum iron and transferrin saturation. This further supports a role of disruption in iron homeostasis among those with obstruction.
Indices of iron homeostasis are thought to be associated with airway obstruction as they reflect total body iron, especially serum ferritin concentrations.26–29 Molecular evolution selected iron to perform a wide range of biological functions, and it is an essential nutrient utilized in almost every aspect of normal cell function. Those same chemical properties which allow iron to serve as a catalyst in reactions of molecular oxygen make it potentially injurious to cells through the generation of oxidative stress. A delicate balance of iron results in every living system with available concentrations being only great enough to meet homeostatic requirements. With elevations in concentrations of available iron following exposures to cigarette smoke and other particles, oxidative stress and injury are possible. The injury can include inflammation. Obstruction is included among the inflammatory responses of the airways to cigarette smoke and other particles.30 Free radical generation catalyzed by increased concentrations of available iron is proposed to be ultimately responsible for tissue injuries such as COPD after exposure to particles.
There are alternative explanations for the relationship between indices of iron homeostasis and FEV1/FVC ratio. Obstructive lung disease can be associated with an acute inflammation and changes in the levels of acute phase reactants, which include serum ferritin and iron concentrations.31–35 Elevation in serum C-reactive protein concentration, reflecting inflammation, is associated with the exacerbation and mortality due to obstructive lung disease.35–37 It can be proposed that the association between serum ferritin concentrations and FEV1/FVC ratio simply reflects the inflammatory response in obstructive lung disease. However, non-smokers with decreased FEV1/FVC ratio demonstrated elevated serum iron concentrations and transferrin saturation which are not consistent with inflammation but can rather reflect increased metal availability.38 This is comparable to previous findings in which there was no relationship between serum C-reactive protein levels and decline in lung function (in a population of individuals 9 years of age and older).39 A second alternative explanation of these results is that both smoking and non-smoking individuals with pre-existing alterations in iron homeostasis may be at increased risk for airway obstruction (ie, the accumulation of metal precedes the obstruction and is independent of it). However, there is no evidence suggesting that such genetic factors could affect obstructive pulmonary disease (eg, airway obstruction is not a prominent feature of hemochromatosis).
The major limitation of this study is the inability to conduct a multivariate regression to determine contributions to FEV1/FVC ratio (including serum iron and ferritin, transferrin saturation, C reactive protein, smoking, race, gender, and age as independent variables). Such a regression is precluded as the variables are not truly independent (eg, serum ferritin increases with smoking, race, gender, and age). In addition, the primacy of the variables and the relationships between the variables determining the order of addition into such a multivariate regression are uncertain (eg, aging is of great significance in determining FEV1/FVC ratio but can possibly reflect the integrated effects of iron accumulation).
Conclusion
We conclude that iron homeostasis is associated with airway obstruction in both smokers and non-smokers with elevation in serum ferritin concentration correlating with lower FEV1/FVC. It is proposed that metal accumulation in cigarette smokers triggers a cascade of biochemical events culminating in inflammatory injury including airway obstruction.40,41 Retention of these particles in lung tissue, with continued iron accumulation, is likely to account for progression of injury and declines in FEV1/FVC despite smoking cessation.42 This same accumulated metal associated with cigarette smoking will increase the risk of other diseases recognized as co-morbidities of obstructive airway disease (eg, coronary artery disease, cerebrovascular disease, peripheral vascular disease, diabetes, neoplasms, and infections).43 Our results are consistent with a documented impact of iron homeostasis on respiratory disease and human mortality.22,44,45 Exposure to particles in non-smokers likely impacts an equivalent metal accumulation to initiate the same pathways of injury. Further investigation into therapies addressing depletion of iron stores may be warranted in the treatment of patients with obstructive lung disease.8,46
Acknowledgments
We thank Edward Hudgens of US Environmental Protection Agency, Office of Research and Development for contract management and Robert Clickner and Rebecca Jeffries of Westat, Rockville Maryland for analytic assistance (contract # 68-D-02-062, WA 3-06).
This report has been reviewed by the National Health and Environmental Effects Research Laboratory, United States Environmental Protection Agency and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the Agency nor does mention of trade names or commercial products constitute endorsement or recommendation for use.
Disclosure
The authors report no conflicts of interest in this work.
References
National Research Council. Environmental Tobacco Smoke: Measuring Exposures and Assessing Health Effects. Washington, DC: National Academy Press; 1986. | ||
Baker RR. Smoke chemistry. In: Davis DL, Nielsen MT, editors. Tobacco-Production, Chemistry and Technology, Chapter 12. Oxford, UK: Blackwell Science; 2000:398–439. | ||
Finelli VN, Petering HG. Effects of metal-binding fractions of tobacco smoke on in vitro activity of enzymes. Arch Environ Health. 1972;25(2):97–100. | ||
Ghio AJ, Stonehuerner J, Quigley DR. Humic-like substances in cigarette condensate and lung tissue of smokers. Am J Physiol. 1994;266(4 Pt 1):L382–L388. | ||
Ghio AJ, Hilborn ED, Stonehuerner JG, et al. Particulate matter in cigarette smoke alters iron homeostasis to produce a biological effect. Am J Respir Crit Care Med. 2008;178(11):1130–1138. | ||
American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis. 1991;144(5):1202–1218. | ||
Kim WJ, Lee SD. Candidate genes for COPD: current evidence and research. Int J Chron Obstruct Pulmon Dis. 2015;10:2249–2255. | ||
Cloonan SM, Glass K, Laucho-Contreras ME, et al. Mitochondrial iron chelation ameliorates cigarette smoke-induced bronchitis and emphysema in mice. Nat Med. 2016;22(2):163–174. | ||
CDC. NHANES III (1988–1994) – Reference Manuals and Report. Available from: https://www.cdc.gov/nchs/nhanes/nh3rrm.htm. Accessed May 5, 2015. | ||
Loría A, Hershko C, Konijn AM. Serum ferritin in an elderly population. J Gerontol. 1979;34(4):521–524. | ||
Leggett BA, Brown NN, Bryant SJ, Duplock L, Powell LW, Halliday JW. Factors affecting the concentrations of ferritin in serum in a healthy Australian population. Clin Chem. 1990;36(7):1350–1355. | ||
Keen CL, Hurley LS. Developmental changes in concentrations of iron, copper, and zinc in mouse tissues. Mech Ageing Dev. 1980;13(2):161–176. | ||
Pan Y, Jackson RT. Insights into the ethnic differences in serum ferritin between black and white US adult men. Am J Hum Biol. 2008;20(4):406–416. | ||
Valberg LS, Sorbie J, Ludwig J, Pelletier O. Serum ferritin and the iron status of Canadians. Can Med Assoc J. 1976;114(5):417–421. | ||
Quan SG, Golde DW. Identification and localization of toxic elements in normal human lung macrophages. Proc Soc Exp Biol Med. 1981;167(2):175–181. | ||
Thompson AB, Bohling T, Heires A, Linder J, Rennard SI. Lower respiratory tract iron burden is increased in association with cigarette smoking. J Lab Clin Med. 1991;117(6):493–499. | ||
McGowan SE, Murray JJ, Parrish MG. Iron binding, internalization, and fate in human alveolar macrophages. J Lab Clin Med. 1986;108(6):587–595. | ||
McGowan SE, Henley SA. Iron and ferritin contents and distribution in human alveolar macrophages. J Lab Clin Med. 1988;111(6):611–617. | ||
Lee CH, Goag EK, Lee SH, et al. Association of serum ferritin levels with smoking and lung function in the Korean adult population: analysis of the fourth and fifth Korean National Health and Nutrition Examination Survey. Int J Chron Obstruct Pulmon Dis. 2016;11:3001–3006. | ||
Shibata Y, Inoue S, Igarashi A, et al. Elevated serum iron is a potent biomarker for spirometric resistance to cigarette smoke among Japanese males: the Takahata study. PLoS One. 2013;8(9):e74020. | ||
McKeever TM, Lewis SA, Smit HA, Burney P, Cassano PA, Britton J. A multivariate analysis of serum nutrient levels and lung function. Respir Res. 2008;9:67. | ||
Brigham EP, McCormack MC, Takemoto CM, Matsui EC. Iron status is associated with asthma and lung function in US women. PLoS One. 2015;10(2):e0117545. | ||
Balmes J, Becklake M, Blanc P, et al; Environmental and Occupational Health Assembly, American Thoracic Society. American Thoracic Society Statement: occupational contribution to the burden of airway disease. Am J Respir Crit Care Med. 2003;167(5):787–797. | ||
Assad NA, Balmes J, Mehta S, Cheema U, Sood A. Chronic obstructive pulmonary disease secondary to household air pollution. Semin Respir Crit Care Med. 2015;36(3):408–421. | ||
Ghio AJ, Soukup JM, Dailey LA. Air pollution particles and iron homeostasis. Biochim Biophys Acta. 2016;1860(12):2816–2825. | ||
Cook JD. Clinical evaluation of iron deficiency. Semin Hematol. 1982;19(1):6–18. | ||
Cook JD, Skikne BS. Iron deficiency: definition and diagnosis. J Intern Med. 1989;226(5):349–355. | ||
Beutler E, Felitti V, Ho NJ, Gelbart T. Relationship of body iron stores to levels of serum ferritin, serum iron, unsaturated iron binding capacity and transferrin saturation in patients with iron storage disease. Acta Haematol. 2002;107(3):145–149. | ||
Mei Z, Cogswell ME, Parvanta I, et al. Hemoglobin and ferritin are currently the most efficient indicators of population response to iron interventions: an analysis of nine randomized controlled trials. J Nutr. 2005;135(8):1974–1980. | ||
Brüske I, Thiering E, Heinrich J, Huster KM, Nowak D. Respirable quartz dust exposure and airway obstruction: a systematic review and meta-analysis. Occup Environ Med. 2014;71(8):583–589. | ||
Baynes R, Bezwoda W, Bothwell T, Khan Q, Mansoor N. The non-immune inflammatory response: serial changes in plasma iron, iron-binding capacity, lactoferrin, ferritin and C-reactive protein. Scand J Clin Lab Invest. 1986;46(7):695–704. | ||
Beard JL, Murray-Kolb LE, Rosales FJ, Solomons NW, Angelilli ML. Interpretation of serum ferritin concentrations as indicators of total-body iron stores in survey populations: the role of biomarkers for the acute phase response. Am J Clin Nutr. 2006;84(6):1498–1505. | ||
Sheikh N, Dudas J, Ramadori G. Changes of gene expression of iron regulatory proteins during turpentine oil-induced acute-phase response in the rat. Lab Invest. 2007;87(7):713–725. | ||
Broekhuizen R, Wouters EF, Creutzberg EC, Schols AM. Raised CRP levels mark metabolic and functional impairment in advanced COPD. Thorax. 2006;61(1):17–22. | ||
Tkacova R, Kluchova Z, Joppa P, Petrasova D, Molcanyiova A. Systemic inflammation and systemic oxidative stress in patients with acute exacerbations of COPD. Respir Med. 2007;101(8):1670–1676. | ||
Sin DD, Man SF. Systemic inflammation and mortality in chronic obstructive pulmonary disease. Can J Physiol Pharmacol. 2007;85(1):141–147. | ||
Karadag F, Kirdar S, Karul AB, Ceylan E. The value of C-reactive protein as a marker of systemic inflammation in stable chronic obstructive pulmonary disease. Eur J Intern Med. 2008;19(2):104–108. | ||
Shenkin A. Trace elements and inflammatory response: implications for nutritional support. Nutrition. 1995;11(Suppl 1):100–105. | ||
Fogarty AW, Jones S, Britton JR, Lewis SA, McKeever TM. Systemic inflammation and decline in lung function in a general population: a prospective study. Thorax. 2007;62(6):515–520. | ||
Rahman I, MacNee W. Role of oxidants/antioxidants in smoking-induced lung diseases. Free Radic Biol Med. 1996;21(5):669–681. | ||
Pryor WA. Cigarette smoke radicals and the role of free radicals in chemical carcinogenicity. Environ Health Perspect. 1997;105(Suppl 4):875–882. | ||
Rutgers SR, Postma DS, ten Hacken NH, et al. Ongoing airway inflammation in patients with COPD who do not currently smoke. Thorax. 2000;55(1):12–18. | ||
Ford ES, Cogswell ME. Diabetes and serum ferritin concentration among U.S. adults. Diabetes Care. 1999;22(12):1978–1983. | ||
Kim KS, Son HG, Hong NS, Lee DH. Associations of serum ferritin and transferrin % saturation with all-cause, cancer, and cardiovascular disease mortality: Third National Health and Nutrition Examination Survey follow-up study. J Prev Med Public Health. 2012;45(3):196–203. | ||
Menke A, Muntner P, Fernández-Real JM, Guallar E. The association of biomarkers of iron status with mortality in US adults. Nutr Metab Cardiovasc Dis. 2012;22(9):734–740. | ||
Martinez JA, Guerra CC, Nery LE, Jardim JR. Iron stores and coagulation parameters in patients with hypoxemic polycythemia secondary to chronic obstructive pulmonary disease: the effect of phlebotomies. Sao Paulo Med J. 1997;115(12):1395–1402. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.