Back to Journals » Patient Related Outcome Measures » Volume 12
Indications, Outcome and Risk Factors of Cesarean Delivery Among Pregnant Women Utilizing Delivery Services at Selected Public Health Institutions, Oromia Region, South West Ethiopia
Authors G/Mariam B, Tilahun T , Merdassa E, Tesema D
Received 7 February 2021
Accepted for publication 3 June 2021
Published 7 July 2021 Volume 2021:12 Pages 227—236
DOI https://doi.org/10.2147/PROM.S304672
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Lynne Nemeth
Belete G/Mariam,1 Temesgen Tilahun,2 Elias Merdassa,3 Desalew Tesema1
1Zonal Health Office, Oromia, Ethiopia; 2College of Medical and Health Science, Wollega University, Oromia, Ethiopia; 3Mettu Health Science College, Oromia, Ethiopia
Correspondence: Desalew Tesema Tel +251911019375
Email [email protected]
Background: Approximately 10% of deliveries are considered as high risk, which may require cesarean section. Besides, a rise in cesarean section delivery is a real public health concern; cesareans are costly and carry 8– 12 and 8 times higher feto-maternal morbidity and mortality, respectively, as compared to vaginal delivery. Like in other countries where unnecessary cesarean delivery is performed, it is also rising in our country, posing potential risk to the mothers and their newborns.
Objective: To assess the indications and outcome of cesarean section delivery among pregnant women utilizing delivery services in selected hospitals.
Methods: A case–control study design was used among 488 randomly selected pregnant women attending delivery services in Bedelle and Mettu-Kharl Hospitals. Data were collected by interviewer-administered questionnaire and entered into EPI-data version 3.1 and exported to SPSS version 20 for cleaning and analyses. Binary logistic regression analysis was used to control for possible confounders. Association was declared at 95% CI and P-value < 0.05 to assess the association between dependent and independent variables. Variables with P-values < 0.05 at bivariate analysis were entered to final logistic regression model.
Results: Nearly 30% and 24.6% of fetuses had been exposed to unfavorable outcome among those delivered following cesarean and vaginal delivery, respectively. The mean age of study participants was 25.79 (SD 6.76) for mothers who underwent cesarean delivery and 24.76 (SD 4.956) for their counterparts. Unfavorable maternal outcome was experienced by 20.5% and 14.7% of pregnant women who gave birth by cesarean and vaginal delivery, respectively. Those not having antenatal care follow-up were five times more likely to encounter unfavorable outcome than attendees (AOR 5.22, 95% CI 1.85– 14.69), while mothers of newborns with low 5th minute Apgar score were 3 times (AOR 2.96, 95% CI 1.07, 8.16), multi-parity 7 times (AOR 7.22, 95% CI 1.45, 36.05) and rural residence were 1.29 times (AOR 1.29, 95% CI 5.09, 12.88) more likely to develop unfavorable feto-maternal outcome.
Conclusion: Vaginal delivery results in more favorable feto-maternal outcomes than does cesarean delivery.
Keywords: cesarean section delivery, Bedelle, Mettu-Kharl Hospital
Background of the Study
In order to replace a generation, pregnancy and delivery are normal physiological phenomena that occur in women. The majority of pregnant women give birth by spontaneous vaginal delivery; however, approximately 10% of deliveries are considered as high risk, which may require cesarean section (CS). Cesarean section is a surgical intervention which is carried out to ensure safety of mother and child when vaginal delivery is not possible (emergency CS) or when the responsible doctors consider that the danger to the mother and baby of vaginal delivery outweighs the risks of CS (planned CS).1–3
In recent years, the CS rate has risen to a record level of 46% in China and 25% or above in many Asian and European countries, Latin America and USA.4 Nowadays, it is estimated about 20 million CS deliveries occur each year in the world. Hence, this makes it the most frequent abdominal surgery performed in adults.5 The number of women giving birth by CS is rapidly growing in a continuous manner in both the developed and developing countries,6 with an estimated prevalence rate of 33%; prevalence ranges from 4% in Africa to 29% in Latin America and Caribbean countries.4,7
The progressively increasing global rate of CS has become one of the most debated issues in maternity care units.4 There is no agreement about what the ideal CS rate should be; however, the World Health Organization (WHO) states that rates of CS below 5% seem to be associated with the existence of gaps in obstetric care units exposing mothers and their newborns to poor health outcomes, whereas rates over 15% do not appear to improve either maternal or infant health.5,8,9 In developing countries, especially in sub-Saharan African countries (SSAC) where the maternal and neonatal mortality rate is high, maternal and infant mortality corresponding with the increasing rate of CS delivery is associated with the quality of obstetric services during pregnancy and childbirth.7,10 There is also a greater risk of neonatal respiratory distress with CS than with vaginal delivery, regardless of gestational age (GA). The type of anesthesia used and the nursing care provided are also among important determinants of the outcome of CS mode of delivery.11
Concerning the indications for performing CS, no standard classification method exists, and they can be numerous or related. Despite these challenges, isolating the most common indications for CS mode of delivery is a key to target preventive approaches. In particular, recognizing indications that are associated with maternal or fetal deaths can help lower mortality, though accessing records of clinical indications in rural resource-limited localities is difficult.12,13
In Ethiopia, maternal and neonatal morbidities and mortality rates are still high. Maternal and neonatal deaths in the country were reported as 470/100,000 and 37/1000 live births, respectively. Although the institutional delivery rate across the country is rising, efforts made so far towards reducing maternal and neonatal mortality rate haves not brought significant changes.10
Methods
Study Setting
The study was conducted in Bedelle and Mettu-Kharl Hospitals, which are found in the south west of Ethiopia, in Buno-Bedelle and Illubabor zones of Oromia regional state, respectively. These facilities are located in the capital administration towns of Illubabor and Buno-Bedelle zones at a distance of 600 km and 480 km from Addis Ababa, respectively. There are about 67 health centers, three functional hospitals and three hospitals under construction, with a total institutional delivery of 65%. The total population of the catchment area for Bedelle Hospital was 770,568 and that of Mettu-Kharl Hospital was 1.5 million. The total deliveries conducted in Bedelle Hospital in the year 2008/2016 were 1820, of which 408 (22.4%) deliveries were by CS, while 2739 deliveries took place in Mettu-Kharl Hospital, of which 600 (21.9%) were by CS. In general, both hospitals serve nearly 2.3 million population, and the total deliveries taking place regardless of the mode of delivery were 4559, of which CS delivery constituted 1008 (22.1%) per year.
Study Design and Period
Institutional based case–control study design was employed from June 02 to August 21, 2017.
Data Collection Instruments and Procedures
Data on feto-maternal cases after delivery were collected by eight midwives after receiving one day's training regarding on how to complete the data collection questionnaire during the patient follow-up period. English version questionnaires was used for interview, and direct observations/examinations were also employed by using observation checklist to gather the required information from study participants starting from 6 hrs after delivery when they become fully conscious and able to respond and during discharge time after consultation had been made with obstetricians and gynecologists including emergency surgeons working in the department. Besides, the clinical information was extracted by assessment of the neonates and the respective mothers. Mothers and neonates were followed for 42 days, using different alternatives. The data collectors visited the mothers and their neonates daily throughout their stay in the hospitals. Before discharge, the study subjects were asked to leave their phone number and respective Kebeles (Gare and Got), so that they could report whenever they face any postnatal danger signs and mothers with such problems could access and be provided with all the possible care easily. In line with this, the data collectors also contacted the mothers every 7 days using a cell phone and made a home visit for those in need of creating a link with health extension workers (HEWs) to request adequate information and provide possible home-based care or facilitate referral. Subsequently, complications and the condition of the mother and baby till discharge from the hospital were assessed. All relevant patient details pertaining to the study were noted on the check list and questionnaire. When death occurred, the date and cause of death were recorded and probable cause of death was assigned after agreement between midwives and physicians based on national and the international disease classification guidelines. Moreover, all participants and their babies were assessed for any morbidity conditions identified during the study period.
Data Entry and Analysis
Data were entered into EPI data version 3.1 and then transferred to SPSS 20 version for checking extreme values and handling prior to entering the major analysis. The outcome variable is delivery by CS. Bivariate logistic regression was carried out to identify individual variables associated with the outcome variable, and all associated variables that have P values <0.05 in binary logistic regression were taken to multivariate logistic regression. Finally, the multivariate logistic regression analysis was carried out to control for confounding variables related to the outcome of CS. The data quality was assured by providing one day's training regarding the objective of the study, confidentiality of information and techniques to conduct interviews.
Result
Socio-Demographic Characteristics
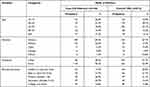
Out of 468 pregnant women who participated in the study, 156 (33.3%) underwent cesarean delivery and 312 (66.7%) of them gave birth by vaginal delivery. The mean age of study participants was 25.79 (SD ± 6.76) for mothers who underwent cesarean delivery and 24.76 (SD ± 4.956) for those mothers who gave birth by vaginal delivery. Regarding age group, the majority of the respondents, 42 (26.9%) and 119 (38.1%), were found in the age group of 15–19 years for cesarean delivery and 20–24 years for vaginal delivery, respectively. Concerning the respondents’ residence, for cesarean delivery 46 (29.5%) and 110 (70.5%) were from urban and rural areas, respectively, and for vaginal delivery 147 (47.1%) and 165 (52.9%) were from urban and rural areas, respectively. The majority of the respondents who underwent CS delivery, 79 (50.6%), had attended primary/secondary school, whereas 23 (14.7%), 34 (21.7%), 20 (12.8%) of CS respondents were unable to read and write, able to read and write, had attended college and above, respectively (Table 1).
Obstetrics Characteristics of Study Participants
Out of study participants at both hospitals, 57 (36.5%), 53 (33.9%) and 46 (29.5%) of women who gave birth by cesarean delivery and 131 (41.9%), 156 (50%) and 25 (8.1%) who gave birth by vaginal delivery had parity of one, two to four, and five and above, respectively. Regarding antenatal care (ANC) follow-up, 104 (66.7%) of mothers who underwent cesarean delivery and 263 (84.3%) of mothers who underwent vaginal delivery had ANC follow-up for their current pregnancy, while the remaining 52 (33.36%) and 49 (15.7%) of women who underwent CS and vaginal delivery did not have ANC follow-up, respectively. For the majority of mothers, the gestational age at labor was 37–41 weeks: 120 (76.9%) and 282 (90.4%) of women who underwent cesarean delivery and vaginal delivery, respectively. Out of all mothers for both modes of delivery, 318 (67.9%) were admitted at first stage and the rest 137 (29.3%) were admitted at second stage. From mothers who underwent cesarean delivery, 109 (69.8%) were emergency and 47 (32.2%) were elective type; from emergency cesarean delivery, 70 (64.2%) were followed by partograph, and 39 (35.8%) were not. Out of women who underwent cesarean delivery, 112 (71.8%) had spinal anesthesia, and the rest 44 (28.2%) had general anesthesia (Table 2).
Indication of Cesarean Section Delivery
The leading indications for cesarean birth were: NRFHR 39 (25%), cephalo-pelvic disproportion (CPD) (17.3%), previous CS 25 (16%), mal-presentation and position 21 (13.5%), failed induction 11 (7%) and others [antepartum hemorrhage (APH), PROM and severe preeclampsia] 33 (21.2%) as shown in Figure 1.
 |
Figure 1 Pie chart showing indication of cesarean delivery among pregnant women utilizing delivery service at Mettu-Kharl and Bedelle Hospitals (June 02–August 21, 2017). |
Fetal and Maternal Complications Seen Following Modes of Deliveries
Fetal complications following CS delivery were observed in 45 (28.8%), whereas complications following vaginal delivery were seen in 77 (24.6%). The leading fetal complications for CS delivery were neonatal sepsis 19 (42.2%), birth asphyxia 13 (28.8%), MAS 6 (13.3%), neonatal jaundice and death 3 (6%). Whereas, for vaginal delivery, the leading complications were neonatal sepsis 30 (38.4%), MAS 15 (19.2%), birth trauma 14 (17.9%), birth asphyxia 13 (16.6%) and death 4 (5%)(Figure 2).
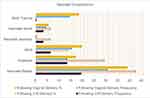 |
Figure 2 Neonatal complications seen following CS and vaginal deliveries among pregnant women utilizing delivery service at Mettu-Kharl and Bedelle Hospitals (June 02–August 21, 2017). |
Thirty-two (20.5%) of women who underwent CS delivery and 46 (14.7%) of those who gave birth by vaginal delivery developed maternal complication. Wound infection 16 (50%), respiratory tract infections 10 (31.3%), post-op fever 4 (12.5%) and others 2 (6.3%) were the commonest maternal complications developed following CS delivery. On the other hand, perineal tear 18 (39.1%), respiratory tract infections 10 (21.7%), wound infection 7 (15.2%), UTI 6 (13.04%) and others 7 (10.8%) were the maternal complications seen among those who underwent vaginal delivery (Table 3).
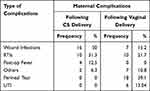 |
Table 3 Complications Seen Following CS and Vaginal Deliveries |
Fetal and Maternal Outcomes Following Modes of Deliveries
From the total of CS deliveries, 45 (28.8%) of fetuses had been exposed to unfavorable outcome, whereas 77 (24.7%) of fetuses born from mothers who underwent vaginal delivery had experienced unfavorable outcome. Thirty-two (20.5%) and 46 (14.7%) of pregnant women who gave birth by CS and vaginal delivery, respectively, had experienced unfavorable maternal outcome, as shown in Table 4.
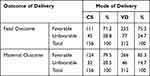 |
Table 4 Fetal and Maternal Outcome Among Pregnant Women Who Gave Birth by Cesarean and Vaginal Modes of Deliveries at Mettu-Kharl and Beddele Hospitals (June 02–August 21, 2017) |
Feto-Maternal Outcome in Terms of Mode of Deliveries
From the total deliveries during the study period, 55 (35.3%) developed unfavorable feto-maternal outcome by CS delivery and 81 (25.7%) were following vaginal delivery as depicted in Figure 3.
 |
Figure 3 Feto-maternal outcome in terms of mode of delivery among pregnant women who gave birth by CS and vaginal modes of deliveries at Mettu-Kharl and Bedelle Hospitals (June 02–August 21, 2017). |
Factors Associated with Unfavorable Feto-Maternal Outcome of Cesarean Section Mode of Delivery
Bivariate analysis on indication of CS delivery showed that not having ANC follow-up, having PROM, multi-parity, age 30 and above, labor duration of 24 hours and above, having an infant with low 5th minute Apgar score, being of rural residence and admission during second stage of labor had statistically significant association with unfavorable outcome with cesarean mode of delivery.
After controlling for confounders, the final model of the multivariate analysis revealed that women without ANC follow-up were 5 times (AOR5.22,95% CI 1.85, 14.69) more likely to develop unfavorable feto-maternal outcome following cesarean delivery than vaginal delivery as compared to those having ANC follow-up, and women of rural residence were 1.29 times (AOR 1.29,95% CI 5.09, 12.88) more likely develop unfavorable feto-maternal outcome following CS delivery than vaginal delivery as compared to those women of urban residency.
Mothers with parity of two and above were 7 times (AOR 7.22, 95% CI 1.45, 36.05) more likely to develop unfavorable feto-maternal outcome following cesarean delivery than vaginal delivery as compared with mothers with parity of one. And mothers having an infant with low Apgarscore at the 5th minute were 3 times (AOR 2.96, 95% CI 1.07, 8.16) more likely to develop unfavorable feto-maternal outcome following cesarean delivery than vaginal delivery as compared having normal Apgarscore at the 5th minute (Table 5).
Discussions
Unfavorable Feto-Maternal Outcome Following Cesarean Section Mode of Delivery
Although CS mode of delivery is one of the lifesaving procedures attributed to the decrease of maternal and neonatal morbidity and mortality rates and also one of the indications for the quality of maternal health services offered, it is associated with unfavorable feto-maternal outcomes. This study revealed a number of important socio-demographic, obstetric and delivery characteristics which are found to have a significant influence on maternal and fetal outcome of cesarean delivery. These include parity of two and above, mothers who did not have ANC follow-up for the recent pregnancy, having an infant with low Apgar score at the 5th minute and being of rural residence.
ANC and Unfavorable Feto-Maternal Outcome Following Cesarean Section Mode of Delivery
The finding of this study showed that mothers who had no ANC follow-up were 5 times more likely to develop unfavorable outcome following cesarean delivery than vaginal delivery as compared to those having ANC follow-up. This finding is similar to the study conducted in Negest Elene General Hospital and health facility in north Wollo zone, Ethiopia, which found that mothers without ANC follow-up were 2.5 and 3.4 times more likely to develop unfavorable outcome following cesarean delivery than vaginal delivery as compared to their counterparts.15,18 Another study conducted at Mettu Kharl and Mekelle showed that women who have ANC follow-up were 66% and 77% less likely to develop unfavorable feto-maternal outcome following cesarean delivery and vaginal delivery, respectively, as compared to those having no ANC follow-up.19,20 This variation may be due to differences in health-seeking behavior and awareness of the importance of ANC follow-up and due to the fact that mothers who did not attend ANC follow-up could not get advice, get early diagnosis and treatment and also early referral to the appropriate health facility though it is needed.
Apgar Score and Unfavorable Feto-Maternal Outcome Following Cesarean Section Mode of Delivery
This study revealed that a number of important socio-demographic, obstetric and delivery characteristics have a significant influence on maternal and fetal outcome of cesarean delivery. Mothers having an infant with an Apgar score of less than 7 at the 5th minute were five times time (AOR 5.55, 95% CI 1.36, 22.71) more likely to develop unfavorable feto-maternal outcome as compared to those with normal 5th minute Apgar score. This finding is similar to the study findings done on birth outcome after CS at Gondar University Teaching Hospital, which showed that low-Apgar score deliveries were 3.19 times more likely to develop unfavorable outcome.21 According to research done at Galamso hospital, 89.7% of the newborns’ Apgar score at the 5th minute were more than 7, while 10.3% were low at less than 7, with a P value of 0.027.22 And the findings of research done at Arba-Minch general hospital were that 78.2% had Apgar scores of more than 7 as compared to 3% with very low Apgar score at the 5th minute.17 This variation may due to low utilization of partograph to follow progress of a labor for early identification of fetal distress and may be type of anesthesia used.
Parity and Unfavorable Feto-Maternal Outcome Following Cesarean Section Mode of Delivery
Mothers who had parity of five and above had 80% (AOR 0.20, 95% CI 0.09, 0.40) lower odds of undergoing cesarean delivery than vaginal delivery as compared to mothers who had parity of one. Mothers having two and above parity were 8.75 times (95% CI 1.94, 39.03) more likely to develop unfavorable feto-maternal outcome as compared to mothers with parity of only one and less than one.
Residence and Unfavorable Feto-Maternal Outcome Following Cesarean Section Mode of Delivery
The findings of this research revealed that women from rural areas were 1.29 times (AOR 1.29, 95% CI 5.09, 12.88) more likely develop unfavorable feto-maternal outcome following CS delivery than vaginal delivery as compared to those women of urban residency. According to findings of research conducted in Chiro and Yirgalem Hospitals, mothers who came from rural areas were 4.011 and 3.36 times more likely to develop unfavorable outcome following cesarean delivery than vaginal delivery as compared to their counterparts, respectively.14,15 Another study conducted in Gelemso, Arba Minch and health facility in north Wollo zone rural mothers were 1.45 and 1.58 times more likely to develop unfavorable feto-maternal outcome following cesarean delivery than vaginal delivery as compared to urban dwellers.3,16,17 This variation may be due to rural women coming to hospital after prolonged duration and complicated labor and are less likely to utilize a health facility than their urban counterparts, and they are also less likely to attend ANC and be followed and attended by health staff skilled in delivery.
Limitations of the Study
This study did not include important variables like monthly income, occupation, religion and marital status.
Conclusion
Cesarean sections performed for appropriate medical or obstetric indications are life-saving for both the mother as well as the newborn. Despite this, 28.8% of fetuses and 20.5% of pregnant women who underwent cesarean delivery had unfavorable outcome. Overall unfavorable feto-maternal outcomes constitute 35.3% following cesarean delivery. Accessing antenatal care in early pregnancy, use of appropriate anesthesia, providing more information on risk and negative consequence of cesarean birth and benefits of vaginal delivery might lower unfavorable outcomes. Moreover, each case should be thoroughly evaluated to determine the possibility for vaginal delivery. The findings of this study can be used as a starting point to design an intervention that could fit the local situation to reduce unfavorable feto-maternal outcome.
Recommendation
Cesarean delivery should be considered for those mothers with absolute indication and who have no option other than cesarean delivery. The health institutions in collaboration with the concerned bodies can provide on-job and off-job trainings for health professionals (surgeons, obstetricians and gynecologists, the anesthesiologists and other concerned health staffs) so that they could capacitate themselves and follow the international and national guidelines which are recommended for choosing to perform cesarean delivery over vaginal delivery. Hence, strengthening ANC follow-up for all pregnant women at the grass root level and all health facilities has value as it is the main gate for the detection of risks associated to pregnancy and to develop complication readiness. Also, trial of vaginal birth after cesarean section (VBAC) should be encouraged in appropriate cases. Community awareness should be created by the HEWs at the grass root level so that communities can develop positive health-seeking behavior. Early referral linkage and appropriate management of cases should be facilitated at all levels of health institutions. Monthly audit of CS delivery and discussion by the concerned bodies is also crucial in reducing the risk of it.
Data Sharing Statement
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Verbal informed consent from the participants was acceptable and approved by the Wollega University Health Institutional Review Board (IRB). As per the Ethiopian National Research Ethics Review Guideline, study participants or legal guardians were provided with a written informed consent for their willingness to participate in this study. Then, the letter was given to the district health office and the health institutions as well. Additionally, a letter of permission to carry out the study was obtained from each administrative body. The purpose of the study was explained to each participant before the interview, and informed verbal consent was taken. The respondents were informed that the data collectors were trained only to collect information, and apart from this particular research the data would not be passed to anybody. Privacy of the respondents was maintained, and confidentiality of the information was respected (personal identification was not used in a way which might be a threat to the respondent). This study was conducted in accordance with the Declaration of Helsinki.
Author Contributions
BGM made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data. TT and EM approved the proposal and result; also participated in editing part of the paper. DT was involved in data analysis, editing, drafting the manuscript and revising it critically for important intellectual content. All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Shabnam S. Caesarean section delivery in India: causes and concerns; 2009; 1–20. Available From: https://iussp.org/sites/default/files/event_call_for_papers/CaesareansectiondeliveryinIndia_0.pdf.
2. RezaieSardari B. A survey on causes of cesarean sections performed at the University Hospitals of Niknafs and Ali-IbnAbiTalib of Rafsanjan, Iran, In The Second Trimester of 2014. JOHE. 2014;3(2).
3. Muhumed AA. Magnitude of maternal complications and associated factors among women who gave birth by cesarean section at general western [internet]. Haramaya University; 2016. Available from: http://213.55.85.90/bitstream/handle/123456789/3134/AminAhmedMuhumed.pdf.
4. Hafeez M, Yasin A, Badar N, et al. Prevalence and indications of caesarean section in a teaching hospital. JIMSA. 2014;27(1):92–93.
5. Soto-Vega E, Casco S, Chamizo K, et al. Rising trends of cesarean section worldwide: a systematic review. Obstet Gynecol Int J. 2015;3(2).
6. Gutema H, Shimye A. Caesarean section and associated factors at MizanAman General Hospital Southwest Ethiopia. J Gynecol Obstet. 2014;2(3):37–41. doi:10.11648/j.jgo.20140203.12
7. Unnikrishnan B, Prasad RB, Amarnath A, et al. Trends and indications for caesarean section in a tertiary care obstetric hospital in Coastal South India. AMJ. 2010;821–825. doi:10.4066/AMJ.2010.465
8. Kaur J, Singh S, Kaur K. Current trend of caesarean sections and vaginal births. Adv Appl Sci Res. 2013;4(4):196–202.
9. Elena S, Marta U, Fernando A, Begines L. The epidemic of the cesarean section in private hospital in Puebla, México. Obstet Gynecol Int J. 2015;2(November 2013):3–7.
10. Kindieyenit M, Gezahegn T, Adefires M, et al. Cesarean section rate, maternal and fetal outcome of birth following cesarean section at Finoteselam Hospital, Northwest Ethiopia: a descriptive retrospective data. Glob J Med Res. 2016;16(3).
11. Ayalewu M. Delivery in Twothree teaching hospitals, [Internet]. Addis Abeba; 2021. Available from: http://etd.aau.edu.et/bitstream/123456789/7703/1/AyalewMareye.pdf.
12. Getahun A. Outcome of cesarean section and the associated factors at Jugel Hospital, Harari Region, Eastern Ethiopia [Internet]. Haramaya Universty; 2015. Available from: https://www.google.com.et/url?sa=t&source=web&cd=1&ved=0ahUKEwiJ3aqXkeLSAhXIXiwKHWs7ApcQFggcMAA&url=http://213.55.85.90/bitstream/handle/123456789/2773/ALEMAYEHU%20GETAHUN.pdf?sequence=2&isAllowed=y&usg=AFQjCNF2ugZIMtrNW6pNauw7dqe7X_yw7Q.pdf.
13. Chu K, Cortier H, Maldonado F, et al. Cesarean section rates and indications in Sub-Saharan Africa: a multi-country study from Medecins SansFrontieres. PLoS One. 2012;7(9):5–10. doi:10.1371/journal.pone.0044484
14. Solomon W. Rate and associated factors of caesarean section at Chiro Zonal Hospital, West Harergae, Oromia Regional State, Eastern Ethiopia [Internet]. Haramaya University; 2016. Available from: http://213.55.85.90/bitstream/handle/123456789/3089/result_cover.pdf?sequence=1&isAllowed=y.pdf.
15. Eshete A, Birhanu D. Birth outcomes among laboring mothers in selected health facilities of North Wollo Zone, Northeast Ethiopia; 2021. Available from: http://file.scirp.org/pdf/Health_2013072408430316.pdf.
16. Tesfaye T, Hailu D. Magnitude of maternal complication and associated factors among mothers undergone cesarean section at Yirgalem General Hospital, SNNPR, Ethiopia; 2021. Available from: http://www.ijhsr.org/IJHSR_Vol.7_Issue.5_May2017/41.pdf.
17. Wae MB, Belayneh F. Magnitude of maternal complications and associated obstetric factors among women who gave birth by cesarean section at Arba-Minich General Hospital, Southern Ethiopia; 2021. Available from: http://www.academicjournals.org/journal/JPHE/article-full-text-pdf/05FFC4D63795.pdf.
18. Abdo RA, Endalemaw TB. Prevalence and associated factors of adverse birth outcomes among women attended maternity ward at Negest Elene Mohammed Memorial General Hospital in Hosanna Town, SNNPR, Ethiopia; 2021. Available from: https://www.omicsonline.org/openaccess/prevalence-and-associated-factors-of-adverse-birthoutcomes-among-women-attendedmaternity-ward-at-negest-elene-mohammed-memorial-2167-0420-1000324.pdf.
19. Seyom E, Abera M. Maternal and fetal outcome of pregnancy related Hypertension in Mettu Karl Referral Hospital, Ethiopia; 2021. Available from: https://pdfs.semanticscholar.org/04f1/89db460d14fcf4dade20c483c6bb7c777546.pdf.
20. Berhe H, Berhe H. Factors associated with patterns of birth outcome at public hospitals in Mekelle Town, Tigray Region, Ethiopia; 2013. Available from: http://www.jbino.com/docs/Issue02_04_2015.pdf.
21. Abdissa Z, Belayneh T, Awoke T et al. Birth outcome after caesarean section among mothers who delivered by caesarean section under general and spinal anesthesia at Gondar University Teaching Hospital North-West Ethiopia; 2021. Available from: https://www.omicsonline.org/birth-outcome-after-caesarean-section-among-mothers-who-delivered-by-caesarean-section-under-general-and-spinal-anesthesia-at-gondar-university-teaching-hospital-northwest-ethiopia-2155-6148.1000335.pdf.
22. Lemma C. Neonatal outcomes of operative deliveries at Gelemso General Hospital, Oromia Regional State, Eastern Ethiopia [Internet]. Haramaya University; 2016. Available from: http://213.55.85.90/bitstream/handle/123456789/3137/ChernetLemma.pdf.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.