Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Independent determinants of disease-related quality of life in COPD – scope for nonpharmacologic interventions?
Authors Brien SB, Stuart B, Dickens AP , Kendrick T, Jordan RE , Adab P , Thomas M
Received 30 September 2017
Accepted for publication 10 November 2017
Published 9 January 2018 Volume 2018:13 Pages 247—256
DOI https://doi.org/10.2147/COPD.S152955
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Sarah B Brien,1 Beth Stuart,1 Andrew P Dickens,2 Tony Kendrick,1 Rachel E Jordan,2 Paymane Adab,2 Mike Thomas1
1Primary Care and Population Sciences, Faculty of Medicine, University of Southampton, Southampton, Hampshire, 2Institute of Applied Health Research, College of Medical and Dental Sciences, University of Birmingham, Birmingham, Warwickshire, UK
Purpose: Quality-of-life (QoL) scores in chronic obstructive pulmonary disease (COPD) have a weak relationship with physiologic impairment. We investigated factors associated with poor QoL, focusing on psychological measures potentially amenable to intervention.
Patients and methods: We utilized a pre-existing Birmingham (UK) COPD cohort to assess factors associated with QoL impairment (COPD Assessment Test [CAT] scores). Univariate and multivariate regression models were constructed from three categories of variables: demographic, lung function/COPD-related symptoms, and psychosocial/behavioral factors.
Results: Analyses were based on self-report questionnaire data from 735 participants. The multivariate model of variables independently associated with CAT included depression, dysfunctional breathing symptoms (Nijmegen score), and illness perception, in addition to COPD symptoms (wheeze, cough), exercise capacity, breathlessness, exacerbations, and deprivation; this model explained 72% of CAT score variation. In a dominance analysis assessing the relative contribution of variables, similar contributions were made by breathlessness (20.2%), illness perception (19.8%), dysfunctional breathing symptoms (17.5%), and depression (12.5%) with other variables contributing <5%.
Conclusion: Psychological factors significantly contribute to disease-specific QoL impairment in COPD, and potentially explain the mismatch between objective physiologic impairment and patients’ experience of their disease. Interventions targeting psychological factors, illness perception, and dysfunctional breathing should be assessed.
Keywords: chronic obstructive pulmonary disease, quality of life, health status, survey, psychological, dysfunctional breathing, breathlessness, illness perception, depression
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality and a global public health problem.1 As a complex, multifaceted disease, it affects patients in many ways and results in significant quality-of-life (QoL) impairment.2 However, QoL varies greatly between individuals, and is only weakly associated with physiologic factors such as percentage predicted forced expiratory volume in 1 second (FEV1).3 Anxiety and depression are common, although frequently unrecognized and untreated,4 and are associated with poor COPD outcomes.5–7 Previous research suggests that a variety of disease-related and patient-related factors may be associated with QoL impairment in COPD.3 In addition to biologic factors (such as lung function and inflammation) and demographic/socioeconomic factors, there is evidence that QoL is affected by comorbidities, particularly psychological conditions,8–11 and by psychological constructs such as illness perception.12 The relative importance of these different factors is currently unclear.
Understanding the determinants of QoL impairment in COPD may highlight modifiable factors that could be targeted to minimize disease impact and to help patients to cope better with the consequences of having an incurable long-term condition. In particular, psychological and behavioral interventions may be appropriate for selected patients. Nonpharmacologic interventions are acceptable to many patients, particularly those with significantly impaired QoL and those with “disproportionate” QoL impairment in relation to their lung function impairment.13 The importance of a “personalized medicine” strategy for managing airways disease has recently been emphasized, aiming to target appropriate treatments, both pharmacologic and nonpharmacologic, on potentially modifiable factors in well-characterized individual patients.14 We hypothesized that a range of psychological, social, perceptual, and behavioral factors, measured using validated patient-reported outcome measures, would be independently associated with QoL in patients with COPD.
Methods
Study design
We report a cross-sectional analysis of data from the Birmingham COPD cohort study.15 The current analysis investigated factors independently influencing disease-specific QoL (assessed by the COPD Assessment Test [CAT])16 and generic health-related (HR) QoL score using the 5 level EuroQoL questionnaire (EQ-5D 5L),17 and estimated the magnitude of contribution of different contributory factors, with a particular focus on clarifying the relative contribution of psychosocial and behavioral factors.
Subjects and setting
The Birmingham COPD cohort study is described fully elsewhere,18 but briefly consists of three patient groups recruited from 71 primary care practices in the West Midlands, UK during the period May 2012–June 2014: 1) patients with diagnosed COPD on general practitioner registers; 2) newly identified COPD patients from a linked case-finding study;15 and 3) participants from the case-finding study with chronic respiratory symptoms but without airflow obstruction. Cohort participants were characterized at baseline with a series of questionnaires and objective measurements (including the Medical Research Council [MRC] breathlessness scale,19 assessments of lung function, muscle strength, and exercise capacity as sit/stand repetitions with Borg breathlessness scores20 pre- and post-exercise). Cohort participants were invited to complete review questionnaires at 6-monthly intervals for 3 years including items regarding health, lifestyle, health-related quality of life (HRQoL), exacerbations, health care usage, and medical conditions; health resource use information was also collected. At the time of this analysis, the full cohort consisted of 2,188 patients. Ethical approval was provided by the National Research Ethics Service Committee, West Midlands, Solihull, UK (ref: 11/WM/0304). All participants provided written informed consent for this study.
For the purposes of the current analysis, an additional questionnaire set was administered at one time point per patient, assessing symptoms of dysfunctional breathing (Nijmegen questionnaire),21 depression (PHQ-9),22 anxiety (GAD-7),23 illness perceptions (Brief Illness Perception Questionnaire, IPQ),24 and agoraphobic avoidance.25 Questionnaires were posted to participants with an explanatory letter and a return envelope, with one reminder sent 2 weeks after the initial mailing.
Patients were included in our analysis if they 1) had an existing COPD diagnosis or were identified from the case-finding trial and 2) met the spirometric criteria for COPD, based on UK guideline definitions (FEV1/FVC [forced vital capacity] <0.7) at the baseline assessment.
Statistical methods
Descriptive statistics are reported on all variables. Univariate associations between disease-specific QoL (CAT score) and other variables were analyzed using linear regression. Initially we fitted univariate regression models to determine which variables were significantly associated with CAT at the 5% level. These variables were taken forward into multivariate regression models to determine which were independently predictive in mutually adjusted analyses. We considered variables within three categories: 1) demographic characteristics (age, sex, body mass index [BMI], socioeconomic status [Index of Multiple Deprivation {IMD}, as quintiles],26 employment status, comorbidity); 2) COPD-related factors (FEV1% predicted, physical activity, chronic cough/phlegm, chronic wheeze, breathlessness, exacerbations, hospitalizations); and 3) psychosocial and behavioral factors (anxiety, depression, dysfunctional breathing symptoms, illness perception, agoraphobic avoidance).
Those variables that were independently predictive of CAT score at the 5% significance level within each of these categories were taken forward in a final regression model to determine which variables were independently predictive overall, and to explore whether psychological measures had an association with CAT score independent of patient characteristics and COPD-related symptoms. In the multivariate models, only cases without missing data in any field were included and none of the missing data were imputed. Although this does result in a reduction in the sample size, as the purpose of this study was to explore the relationship between variables and to determine which were most highly predictive of HRQoL, it was important that participants contributed data on all variables. A multiple imputation model would have required some assumption of the likely distribution of missing values and might have introduced bias into our exploratory analysis by imposing a likely relationship between variables and between the variables and HRQoL.
The R-squared value was used in order to quantify the extent to which the variables explained the variation in CAT score. To determine the contribution that each predictor made to the overall variance, and therefore their relative importance, a dominance analysis was undertaken.27 Dominance analysis examines the change in R-squared from adding a variable to all possible subset regression models and then averaging across all possible models. In this way, it is possible to obtain a general dominance weight and thereby partition the R-squared value among the predictors. All variables that were significant in their respective categories were included in the dominance analysis.
A further analysis was conducted using the same methodology with generic HR QoL score EQ-5D 5L rather than the disease-specific CAT score as the outcome variable.
Analyses were carried out in Stata v14 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP).
Results
Eligible population
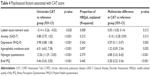
One thousand six hundred three cohort participants meeting entry criteria and with valid spirometry readings were posted the additional questionnaire sets, and 1,233 were returned (76.9%). Of these, 181 were excluded from analysis as they did not have obstructive spirometry (FEV1/FVC ratio <0.70), and a further 317 as they did not have a valid CAT score, leaving an analysis sample of 735 participants (consisting of 599 previously diagnosed COPD subjects and 136 identified through case finding). The case-found patients had milder disease, with better-preserved lung function, less breathlessness, chronic cough and wheeze, and a history of fewer exacerbations (Table 1).
A large variation in CAT score was observed (mean, SD CAT score 17.9, 8.3). Case-found participants reported less COPD impact compared to those with diagnosed COPD (14.0, 7.6 vs 18.7, 8.2, respectively).
Univariate and multivariate associations with COPD-related QoL
Demographic characteristics
Four patient characteristics were significantly associated with higher CAT score: higher level of deprivation (IMD status), being currently unemployed, younger age, and being a current smoker (Table 2). Although these associations were statistically significant at the 5% level, the R-squared values were low. The highest R-squared value was for deprivation and even that explained only 5.7% of the variation in CAT scores.
  | Table 2 Patient demographic characteristics associated with CAT score |
Lung function and COPD-related symptoms
The independent predictors in this category were chronic wheeze, chronic cough/phlegm, exercise capacity at baseline (sit/stand repetitions), MRC score, Borg breathlessness pre- and post-exercise scores, and having ≥2 exacerbations in the previous 12 months (Table 3). The MRC score was the strongest predictor, explaining 46% of the variation in CAT score in this category of factors. The other variables explained no more than 16% each, with lung function impairment (% predicted FEV1) independently explaining under 6% of CAT variation in this category group.
Psychosocial and behavioral factors
The PHQ-9 (measuring depression), Nijmegen questionnaire (measuring symptoms of dysfunctional breathing), and the brief IPQ (measuring illness perceptions) were all significantly associated with CAT in this group of factors, and explained 34%, 38%, and 45% of the variance in CAT, respectively. Anxiety (GAD-7) scores were not significantly independently associated and agoraphobic avoidance scores were only weakly associated (Table 4).
Full multivariate model and dominance analysis
A full multivariate model was constructed including all variables independently associated with CAT from each category (Table 5). This model only included people without missing data for any variable (n=476). In this model, depression (PHQ9), dysfunctional breathing symptoms (Nijmegen score), illness perception (IPQ), symptoms of both chronic wheeze and chronic phlegm/cough, exercise capacity (sit/stand repetitions), breathlessness (MRC score and Borg score post-exercise), having ≥2 exacerbations in the previous year, and deprivation (IMD quintile) were all significantly associated with CAT at the 5% level. This model explains 72.2% of the observed variation in CAT.
In the dominance analysis, the largest contributions to variation in CAT scores were made by functional breathlessness (MRC score, 20.2% of R-squared value), with illness perception (IPQ) providing only a slightly lower contribution (19.8%). Dysfunctional breathing symptoms (Nijmegen questionnaire, 17.5%) and depression (PHQ9, 12.5%) were the next most important contributors to the CAT variation, and other variables contributed 5% or less.
Analysis using generic HRQoL (EQ-5D 5L)
A further analysis was performed with generic QoL score (EQ-5D 5L) as the outcome measure (Table 6). Generally, the same variables emerged as important predictors, although measures of depression (PHQ-9) and anxiety (GAD-7) were more strongly associated with EQ-5D 5L than with CAT scores. This model predicted 60.4% of the variation in the EQ-5D 5L, with the largest contributions made by depression (PHQ-9, 23.1%), functional breathlessness (MRC score, 20.1%), illness perception (IPQ, 16.0%), anxiety (GAD-7, 14.0%), and symptoms of dysfunctional breathing (Nijmegen score, 13.3%). The other significant variables (exercise capacity, BMI, physical activity levels, breathlessness pre-exercise, smoking status, deprivation, chronic wheeze, and employment status) all made smaller contributions (5% or less).
Discussion
The stimulus for this study was the observation that there is a large discrepancy at an individual level between the objective, biologic severity of COPD and the impact of the disease on the patient, as assessed by functional impairment and effects on QoL. We aimed to assess and quantify the relative contributions of psychosocial and behavioral factors on QoL, in order to identify candidate targets for future interventions. In this cohort of community-based patients predominantly having physiologically mild-to-moderate COPD, we observed a wide variation in disease-related QoL scores, with a mean (SD) CAT score of 17.9 (8.3). The reference values for CAT scores suggest that a score of <10 indicates low impact, 10–20 moderate impact, and >20 high impact,28 showing that the patients in our cohort spanned a wide range of perceived QoL impairment from their COPD, ranging from low to very high impact. As in previous research, a weak relationship was observed between physiologically assessed lung function and QoL.29
We found, unsurprisingly, that a major independent contribution to impaired QoL came from functional, activity-related breathlessness, with the MRC breathlessness score explaining 20% of the variation in both disease-specific (CAT) and generic QoL scores (EQ-5D 5L). However, we also found that both pessimistic health beliefs (as measured by the validated IPQ) and depressed psychological state (assessed by the PHQ-9) have major independent impacts on patients’ experience of their COPD, explaining 20% and 12%, respectively, of the variation in CAT scores and high proportions (16% and 23%, respectively) of the variation in EQ-5D 5L. In addition, we found that dysfunctional breathing (measured by the Nijmegen Questionnaire) independently explained a large proportion of QoL variability (17% of CAT and 13% of EQ-5D 5L). All these factors are potentially amenable to intervention. Overall, the models we constructed explained over 70% of the variation in disease-specific QoL and over 60% of that in generic QoL.
Our findings are in keeping with other smaller studies suggesting that psychological factors and illness perceptions are important determinants of well-being, overshadowing the influence of “harder” factors such as lung function in COPD.3,8,12,30,31 Illness perception is a construct of the cognitive representations and beliefs that patients have about their illness, and has been found to be an important determinant of behavior and to be associated with a number of important outcomes, including treatment adherence and functional recovery.32 The Brief IPQ is a widely used and validated tool with good psychometric properties.33 There is limited research linking poor illness perception with disability and impaired QoL in COPD,34 and no interventional studies that we are aware of. There is emerging evidence that brief, straightforward psychoeducational interventions can help to modify negative illness beliefs and lead to improvements over a range of different health outcomes.35 In view of the findings we report in this study, there is a case for developing interventional studies based on strategies to improve illness perception in COPD.
There is consistent evidence that depression and anxiety are common comorbidities in patients with COPD and are associated with poor outcomes.3–10,36,37 There is, however, surprisingly little evidence to support the use of psychological interventions in managing COPD, or to clarify which interventions are most effective and acceptable.38 Although there is some preliminary evidence to support interventions such as relaxation, cognitive behavioral therapy, self-management, and antidepressant medication in COPD, the data are limited and mainly consisted of small studies.38 Qualitative evidence suggests that psychological interventions are acceptable to COPD patients with disproportionately impaired QoL in relation to lung function impairment, particularly interventions based on nonpharmacologic strategies.13 Our finding that a large proportion of QoL variation is explained by psychological factors supports the need for interventional studies.
A novel contribution of this study was to include a measure of dysfunctional breathing, the Nijmegen Questionnaire, which was found to be a major contributor to the variation in both generic and disease-specific QoL. Although this questionnaire has not been validated for use in COPD, it has been widely used in other airways diseases including asthma,39 with breathing retraining interventions shown to improve QoL scores.40 The significant independent association of Nijmegen Questionnaire score to QoL improvement in patients with COPD indicates that breathing retraining may also be a possible strategy to improve QoL in people with COPD.
A strength of this study was the availability of data from a large well-characterized UK COPD cohort, containing a relatively representative sample of patients with mild and moderate COPD treated in primary care. The large sample size, compared with much smaller previous studies (two studies had samples of <100),12,30 and the collection of data on a wide panel of disease-related factors allowed us to examine the relative contribution of different factors relating to QoL impairment in COPD. We were able to include a wide range of potential explanatory variables in the models, which were more inclusive than those in previous studies. Also, unlike previous studies that used only generic QoL tools,31 we used both generic and disease-specific instruments. Similar messages emerged from our study for disease-specific and generic QoL instruments.
A limitation of our study is that it is cross-sectional, describing associations between measured factors and QoL that cannot be assumed as causal, and there is no certainty that interventions targeting these factors will result in clinically important improvements in QoL. It does, however, provide a justification for future interventional studies targeted on improving illness perception, improving depression and correcting dysfunctional breathing in COPD patients, particularly in those with disproportionately impaired QoL in relation to lung function impairment.
Conclusion
COPD is a distressing and progressive condition that makes life miserable for many, and a holistic and multidimensional, personalized approach is needed.14 The clinical focus in COPD is generally directed toward biologic factors such as physiologic impairment and airways inflammation, with a predominant focus on pharmacologic interventions. However, along with smoking cessation, nonpharmacologic approaches are also very important in improving patient outcomes, with pulmonary rehabilitation now recognized as being a key element in overall disease management. This study shows that there are a number of factors associated with QoL impairment that could potentially be modified through suitable nonpharmacologic interventions focused on appropriately characterized patients, and supports the need for future interventional studies.
Acknowledgments
This paper presents independent research funded by the National Institute for Health Research School for Primary Care Research (NIHR SPCR, project ref: 239). The BLISS cohort is funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research (grant reference number RP-PG-0109-10061). The views expressed are those of the author(s) and not necessarily those of the NIHR, the NHS, or the Department of Health. The Birmingham COPD Cohort study is part of the Birmingham Lung Improvement Studies: BLISS.
Author contributions
The original conception of the study came from SBB and MT, with input from all authors. Overall study management was by SBB. The BLISS cohort is conceived and managed by PA, REJ, and APD, who managed data acquisition and management. TK provided expertise in psychological morbidity and BS was the study statistician. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
MT declares personal fees from GSK, Novartis, BI, and Aerocrine, outside the submitted work. The authors report no other conflicts of interest in this work.
References
Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017. Global Strategy for the Diagnosis, Management and Prevention of COPD. Available from: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/. Accessed April 25, 2017. | ||
Jones PW. Health status measurement in chronic obstructive pulmonary disease. Thorax. 2001;56(11):880–887. | ||
Tsiligianni I, Kocks J, Tzanakis N, Siafakas N, van der Molen T. Factors that influence disease-specific quality of life or health status in patients with COPD: a systematic review and meta-analysis of Pearson correlations. Prim Care Respir J. 2011;20(3):257–268. | ||
Kunik ME, Roundy K, Veazey C, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127(4):1205–1211. | ||
Cleland JA, Lee AJ, Hall S. Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Fam Pract. 2007;24(3):217–223. | ||
Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status and quality of life. Arch Intern Med. 2007;167(1):60–67. | ||
Eisner MD, Blanc PD, Yelin EH, et al. Influence of anxiety on health outcomes in COPD. Thorax. 2010;65(3):229–234. | ||
Burgel PR, Escamilla R, Perez T, et al; INITIATIVES BPCO Scientific Committee. Impact of comorbidities on COPD-specific health-related quality of life. Respir Med. 2013;107(2):233–241. | ||
Blakemore A, Dickens C, Guthrie E, et al. Depression and anxiety predict health-related quality of life in chronic obstructive pulmonary disease: systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2014;9:501–512. | ||
Balcells E, Gea J, Ferrer J, et al; PAC-COPD Study Group. Factors affecting the relationship between psychological status and quality of life in COPD patients. Health Qual Life Outcomes. 2010;8:108. | ||
Moy ML, Reilly JJ, Ries AL, et al. National Emphysema Treatment Trial Research Group. Multivariate models of determinants of health-related quality of life in severe chronic obstructive pulmonary disease. J Rehabil Res Dev. 2009;46(5):643–654. | ||
Weldam SW, Lammers JW, Heijmans MJ, Schuurmans MJ. Perceived quality of life in chronic obstructive pulmonary disease patients: a cross-sectional study in primary care on the role of illness perceptions. BMC Fam Pract. 2014;15:140. | ||
Brien SB, Lewith GT, Thomas M. Patient coping strategies in COPD across disease severity and quality of life: a qualitative study. NPJ Prim Care Respir Med. 2016;26:16051. | ||
Agusti A, Bel E, Thomas M, et al. Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J. 2016;47(2):410–419. | ||
Jordan RE, Adab P, Sitch A, et al. Targeted case finding for chronic obstructive pulmonary disease versus routine practice in primary care (TargetCOPD): a cluster-randomised controlled trial. Lancet Respir Med. 2016;4(9):720–730. | ||
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Leidy NK. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. | ||
The EuroQol Group. EuroQol a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. | ||
Adab P, Fitzmaurice DA, Dickens AP, et al. Cohort Profile: the Birmingham Chronic Obstructive Pulmonary Disease (COPD) Cohort Study. Int J Epidemiol. 2017;46(1):23. | ||
Stenton C. The MRC breathlessness scale. Occ Med. 2008;58(3):226–227. | ||
Mador MJ, Rodis A, Magalang UJ. Reproducibility of Borg scale measurements of dyspnea during exercise in patients with COPD. Chest. 1995;107(6):1590–1597. | ||
van Dixhoorn J, Duivenvoorden HJ. Efficacy of Nijmegen questionnaire in recognition of the hyperventilation syndrome. J Psychosom Res. 1985;29(2):199–206. | ||
Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psych Ann. 2002;32(9):509–515. | ||
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Int Med. 2006;166(10):1092–1097. | ||
Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–637. | ||
National Improving Access to Psychological Therapies Programme Team. The IAPT Data Handbook v2.0.1 Appendices: D8.2, p 34. London, UK: National IAPT Programme Team, Department of Health; June 2011. | ||
UK Government Gov. UK Department for Communities and Local Government. English indices of deprivation 2015. Available from: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015. Accessed April 26, 2017. | ||
Budescu DV. Dominance analysis: a new approach to the problem of relative importance of predictors in multiple regression. Psychog Bull. 1993;114:542–551. | ||
COPD Assessment Test Healthcare Professionals User Guide. Available from: http://www.catestonline.org/images/UserGuides/CAT_HCP%20User%20Guide.pdf. Accessed April 26, 2017. | ||
Jones PW, Brusselle G, Dal Negro RW, et al. Properties of the COPD assessment test in a cross-sectional European study. Eur Respir J. 2011;38(1):29–35. | ||
Bentsen SB, Henriksen AH, Wentzel-Larsen T, Hanestad BR, Wahl AK. What determines subjective health status in patients with chronic obstructive pulmonary disease: importance of symptoms in subjective health status of COPD patients? Health Qual Life Outcomes. 2008;6:115. | ||
Vaske I, Kenn K, Keil DC, Rief W, Stenzel NM. Illness perceptions and coping with disease in chronic obstructive pulmonary disease: effects on health-related quality of life. J Health Psychol. 2017;22(12):1570–1581. | ||
Broadbent E, Wilkes C, Koschwanez H, Weinman J, Norton S, Petrie KJ. A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Psychol Health. 2015;30(11):1361–1385. | ||
The IPQ website [homepage on the Internet]. The illness perception questionnaire. Available from: http://www.uib.no/ipq/. Accessed April 26, 2017. | ||
Mewes R, Rief W, Kenn K, Ried J, Stenzel N. Psychological predictors for health-related quality of life and disability in persons with chronic obstructive pulmonary disease (COPD). Psychol Health. 2016;31(4):470–486. | ||
Broadbent E, Ellis CJ, Thomas J, Gamble G, Petrie KJ. Further development of an illness perception intervention for myocardial infarction patients: a randomized controlled trial. J Psychosom Res. 2009;67(1):17–23. | ||
Cully JA, Graham DP, Stanley MA, et al. Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics. 2006;47(4):312–319. | ||
Dahlén I, Janson C. Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest. 2002;122(5):1633–1637. | ||
Smith SM, Sonego S, Ketcheson L, Larson JL. A review of the effectiveness of psychological interventions used for anxiety and depression in chronic obstructive pulmonary disease. BMJ Open Respir Res. 2014;1(1):e000042. | ||
Thomas M, McKinley RK, Freeman E, Foy C. Prevalence of dysfunctional breathing in patients treated for asthma in primary care: cross sectional survey. BMJ. 2001;322(7294):1098–1100. | ||
Thomas M, McKinley RK, Mellor S, et al. Breathing exercises for asthma: a randomised controlled trial. Thorax. 2009;64(1):55–61. |
 © 2018 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2018 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.