Back to Journals » Nature and Science of Sleep » Volume 14
Independent Association Between Oxygen Desaturation Index and Cardiovascular Disease in Non-Sleepy Sleep-Disordered Breathing Subtype: A Chinese Community-Based Study
Authors Wang L, Ou Q, Shan G , Lao M, Pei G , Xu Y, Huang J, Tan J, Chen W, Lu B
Received 27 April 2022
Accepted for publication 29 July 2022
Published 11 August 2022 Volume 2022:14 Pages 1397—1406
DOI https://doi.org/10.2147/NSS.S370471
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Longlong Wang,1,2 Qiong Ou,1,2 Guangliang Shan,3 Miaochan Lao,2 Guo Pei,2 Yanxia Xu,2 Jinhuan Huang,4 Jiaoying Tan,1,2 Weiping Chen,1,2 Bing Lu1,2
1The Second School of Clinical Medicine, Southern Medical University, Guangzhou, People’s Republic of China; 2Sleep Center, Department of Pulmonary and Critical Care Medicine, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangdong Provincial Geriatrics Institute, Guangzhou, People’s Republic of China; 3Department of Epidemiology & Biostatistics, Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences/School of Basic Medicine, Peking Union Medical College, Beijing, People’s Republic of China; 4Department of Pulmonary and Critical Care Medicine, People’s Hospital of Chenghai, Shantou, People’s Republic of China
Correspondence: Qiong Ou, Sleep Center, Department of Pulmonary and Critical Care Medicine, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangdong Provincial Geriatrics Institute, Guangzhou, 510080, People’s Republic of China, Tel +86 13609717251, Email [email protected]
Purpose: Non-sleepy sleep-disordered breathing (SDB) is increasingly recognized as an important clinical subtype. The association between non-sleepy SDB and cardiovascular disease (CVD) is not well understood. Our objectives were to investigate the relationship between non-sleepy SDB and CVD and determine which nocturnal hypoxia parameter most strongly reflects this association in a large community population.
Patients and Methods: Cross-sectional data from 3626 randomly-selected Chinese community-dwelling participants who underwent overnight type IV sleep monitoring were analyzed. Parameters of nocturnal hypoxemia were extracted from sleep monitoring devices, including mean nocturnal oxygen saturation, lowest oxygen saturation, oxygen desaturation index (ODI), and time with oxygen saturation < 90%. An ODI ≥ 7.0 events/h was considered to signify SDB. An Epworth Sleepiness Scale score of 10 or less indicated no sleepiness.
Results: The SDB rate was 30.7% (1114/3626), of which 96.5% (1075/1114) were considered the non-sleepy SDB subtype. ODI, typical nocturnal intermittent hypoxia indicator for SDB, was independently related to CVD, regardless of whether excessive daytime sleepiness was present. After adjusting for confounders, ODI most strongly reflected the association between non-sleepy SDB and CVD (OR:1.023; 95% CI:1.003– 1.043). We observed a nonlinear association between ODI and the prevalence of CVD, where the likelihood of CVD increased with ODI≥ 10 events/h and a markedly increasing trend was observed with ODI ≥ 20 events/h (reference ODI = 7.0 events/h). Metabolic parameters, Pittsburgh Sleep Quality Index, and inflammatory marker did not mediate the association between ODI and CVD in the non-sleepy SDB subtype.
Conclusion: In the Chinese community-dwelling population, non-sleepy SDB was highly prevalent. ODI, an easily extracted indicator from a type IV sleep monitor, most strongly reflected the association between non-sleepy SDB and CVD.
Keywords: oxygen desaturation index, cardiovascular disease, non-sleepy, sleep-disordered breathing, community-based general population
Introduction
Sleep-disordered breathing (SDB) is a common disturbance characterized by recurrent episodes of apnea/hypopnea during sleep. Considering an apnea-hypopnea index (AHI) threshold value of ≥5 events/h, it is estimated that 936 million adults aged 30–69 years suffer from SDB.1 China has the highest number of individuals affected by SDB.1 SDB is associated with increased risk of cardiovascular disease, insulin resistance, and diabetes mellitus.2–4 The most widely recognized manifestation of SDB and the primary target for treatment is excessive daytime sleepiness (EDS). Nevertheless, in individuals with cardiovascular conditions including hypertension or in the general population, this complaint is not prevalent and is present in as few as 15–50% of patients with SDB.5–7 In contrast, non-sleepy SDB may be the dominant subtype, making it more difficult to suspect SDB and less likely to bring patients to medical attention.
A strong association between SDB and cardiovascular disease (CVD) has been established.8 However, the relationship between the non-sleepy SDB subtype and CVD remains unclear; because SDB has been identified as a heterogeneous disorder, the severity determined using AHI does not reflect the myriad of symptoms (eg daytime sleepiness owing to various reasons9), clinical outcomes, and response to therapy.10–13 In addition, several large clinical trials have shown that there is no positive effect of CPAP therapy in secondary prevention of cardiovascular events14–16 in patients with non-sleepy SDB. On the one hand, this suggests that primary prevention of cardiovascular events in SDB patients may be critical, as reversing an impaired vascular flow may be more difficult than preventing it. On the other hand, this may reflect the fact that previous studies included predominantly non-sleepy participants, as recent evidence suggests that EDS is a phenotype of poor cardiovascular outcomes in SDB.11,17 This makes it necessary to further explore the intrinsic relationship between non-sleepy SDB and CVD.
To treat or not to treat non-sleepy SDB has been a topic of controversy, even considering that studies have shown that treatment of non-sleepy SDB can improve depressive mood and quality of life.18,19 Previous studies have shown early cardiovascular abnormalities in non-sleepy SDB may be observed. Kohler et al20 found that minimally symptomatic SDB was associated with impaired endothelial function and increased arterial stiffness. Ayers et al21 revealed that the level of circulating cell-derived microparticles—considered a marker of cardiovascular risk—was elevated in participants with minimally symptomatic SDB compared to that in control participants without SDB. This leads us to believe that the timing of initiation of CPAP therapy for non-sleepy SDB may be critical; initiation of therapy after appearance of a comorbid CVD would be too late to provide cardiovascular protection. Therefore, the early identification of non-sleepy SDB may be particularly significant in the general population for cardiovascular risk prediction. In addition, it is important to explore which indicator best reflects the risk of CVD in non-sleepy SDB, as this will provide useful information for implementing primary prevention of CVD in patients with non-sleepy SDB.
Studies have demonstrated that SDB severity defined by the apnea-hypopnea index (AHI) has poor predictive power of SDB-related adverse outcomes.22,23 Intermittent hypoxemia has been recognized as a critical factor mediating cardiovascular risk in patients with SDB.24 For example, Kendzerska et al25 reported that “time with oxygen saturation of <90%” was considered an independent predictor of composite cardiovascular outcome in a clinical historical cohort. However, there is a lack of consensus regarding which measurements of nocturnal hypoxemia are the most sensitive and reliable predictors of CVD,23 especially for patients with non-sleepy SDB in community settings. The metrics of nocturnal hypoxemia can be easily extracted from a type IV sleep monitor or consumer-grade devices for sleep monitoring, which is suitable for screening SDB in the community-based general population, potentially providing predictors of cardiovascular risk.
The ambiguous relationship between non-sleepy SDB and CVD adds further mystery to the unclear role of CPAP in the secondary prevention of cardiovascular events in non-sleepy SDB. In addition, as non-sleepy SDB is less likely to attract medical attention, exploration of the role of CPAP in the primary prevention of cardiovascular events becomes difficult. Exploring an appropriate screening tool that can both identify SDB and provide markers of potential CVD risk, especially in a large-scale community, may open a convenient avenue for primary prevention of cardiovascular events in individuals with non-sleepy SDB. Therefore, the purpose of this study is to investigate the relationship between non-sleepy SDB and CVD and to determine which nocturnal hypoxia parameter, extracted from a type IV sleep monitor, most strongly reflects this association in a large community population.
Materials and Methods
Study Participants
This was a prospective, multi-site, cross-sectional cohort study based on a Chinese community population. Participants were recruited from the general population in the community setting between April 9 and May 18, 2021. A detailed description of the recruited participants has been given in a recently published study by He et al.26 Specifically, a multi-stage, stratified cluster sampling scheme was used to select a representative population. First, we chose cities (Shantou and Meizhou) in the Guangdong Province in southern China and then districts (Chenghai, Jinping, and Meijiang) or counties (Nan’ao and Jiaoling) in these cities; next, villages were selected from the counties and communities from urban streets or districts; finally, residents of the selected villages and communities were invited to participate in the survey with the support of the local government. This study was designed and implemented in accordance with a previously published study entitled “Data Resource Profile: The China National Health Survey (CNHS).”27 The inclusion criteria were as follows: 1) community residents aged ≥18 years living at the study sites for ≥6 months; 2) those that voluntarily participated in the study and provided informed consent; and 3) those capable of cooperating with investigators to complete all assessments, including the structured questionnaire, sleep monitoring, physical examination, and fasting blood draw. Participants with cognitive dysfunction, mobility disabilities, or severe organic disease were excluded. A total of 3829 individuals completed effective sleep monitoring. The present study was approved by the Ethics Committee of Guangdong Provincial People’s Hospital, approval number GDREC2020221H(R1). All participants provided written informed consent. The study was compliant with the Declaration of Helsinki. In addition, the present study has been registered on the Chinese Clinical Trial Registry of the International Clinical Trials Registry Platform of the World Health Organization, ChiCTR2200061419 (https://www.chictr.org.cn/showprojen.aspx?proj=172540).
Overnight Sleep Study
The sleep study was performed using type IV wearable intelligent sleep monitor (WISM) (CloudCare Healthcare Co., Ltd., Chengdu, China). The device has been described in detail in our previous study.28
Briefly, the measurement of pulse oximetric saturation was performed using a photoelectric reflex sensor according to the absorption characteristics of hemoglobin to infrared and red light (Figure S1). Based on the physical activity signals, artifact recognition, and built-in automatic algorithm, the effective monitoring time and the number of oxygen saturation drops (≥ 3% or ≥ 4%) were recorded and analyzed. A report was then generated in an automated fashion. The palmar thenar major muscles were the recommended monitoring sites. Veins, scars, spots, and locations with thick hair are required to be avoided. The device can monitor continuously for seven hours throughout the night, and after disinfection and charging, it can be recycled. Monitoring parameters included 3% or 4% ODI, nocturnal mean oxygen saturation (MeanSpO2), lowest nocturnal oxygen saturation (MinSpO2), and time spent with oxygen saturation below 90% (T90). The sleep monitoring system has been validated by comparison against polysomnography at the Sleep Center of Guangdong Provincial People’s Hospital (Figure S2). The ODI represents the number ≥ 4% oxygen saturation drops divided by the effective monitoring time in hours. When the ODI reaches 7.0 events/h—the optimal cut-off value, it has a sensitivity, specificity, and accuracy of 86%, 91%, and 95%, respectively, to predict SDB defined by an AHI ≥5 events/h.28 Therefore, in the present study, an ODI ≥7.0 events/h was considered to indicate the presence of SDB.
Assessment of Excessive Daytime Sleepiness
The Epworth Sleepiness Scale (ESS) was used to evaluate subjective excessive daytime sleepiness (EDS).29 A score of >10 indicated the presence of EDS.30 An ESS score ≤10 and an ODI ≥7.0 events/h indicated non-sleepy SDB.
Anthropometric Measurements
The details of height, weight, and blood pressure measurements were described in a previously published article.27 Body mass index (BMI) was calculated as weight divided by height squared. BMI ≥ 25 kg/m2 was defined as obese. Two neck and waist circumference measurements were performed by trained technicians. Measurements were taken at the superior border of the cricothyroid cartilage for neck circumference, and at the level of 1 cm above the umbilicus for waist circumference.
Blood Parameters
For each participant, blood samples were collected after 8 h overnight fasting to evaluate related indicators, including blood lipid profile parameters (total cholesterol [CHO], triglycerides [TG], low-density lipoprotein cholesterol [LDL-C], and high-density lipoprotein cholesterol [HDL-C]), fasting glucose, and high-sensitivity C-reactive protein (hsCRP). Details on collection, transportation, processing, storage, and analysis of blood specimens were described in a previously published article.27
Definition of Outcome Variable and Comorbidities
Hypertension was defined as the use of antihypertensive medication and/or either systolic/diastolic blood pressure ≥140/90 mmHg.31 Diabetes was defined as fasting glucose ≥7 mmol/L or diabetes medication use (oral antihyperglycemic agents and/or insulin).32 CVD was defined by a diagnosis of hypertension or having a self-reported history of coronary artery disease, heart failure, or stroke.
Statistical Analyses
Data were described as median (interquartile range) for continuous variables or frequencies (percentages) for categorical variables. The Mann–Whitney U-test or chi-square test was used to compare variables between groups. To determine the effect of EDS on the ODI and CVD relationship, logistic regressions were used. To further clarify whether EDS is a mediator in the ODI and CVD relationship, we used the R package “Mediation” for mediating effect analysis.33 To determine which indicator of nocturnal hypoxemia is more likely to predict CVD in patients with non-sleepy SDB, we again conducted logistic regression using ODI, minSpO2, meanSpO2, T90, and percentage of sleep time with SpO2 <90% (T90%), as potential predictors and adjusted for other related confounding factors. When ODI was identified as a potential predictor, we modeled possible non-linearity of the association between ODI and likelihood of CVD with restricted cubic splines in individuals with non-sleepy.
Also, we investigated the interaction effect between the ODI and sex, age (<60 vs ≥60 years), BMI (<25 vs ≥25 kg/m2), or diabetes in patients with non-sleepy SDB. A mediation analysis was performed using the following variables with the potential association for ODI and CVD in patients with non-sleepy SDB: TG, LDL-C, HDL-C, CHO, Pittsburgh Sleep Quality Index (PSQI), and hsCRP. Statistical tests were two-sided, and P <0.05 was considered statistically significant. Statistical analyses were conducted using SPSS (version 23.0; Armonk, NY, USAI) and R (version 4.1.2).
Results
Figure S3 shows the flowchart of study enrollment. Table 1 summarizes the clinical characteristics of study participants with and without EDS. A total of 97.0% of the participants did not report EDS. Non-sleepy participants were younger, with lower BMI, neck circumference, and waist circumference than participants with EDS. However, they had similar ODI, minSpO2, mean SpO2, and T90. In participants who did not report EDS, there was a lower prevalence of diabetes and CVD.
 |
Table 1 Characteristics of the Studied Population According to the Presence of EDS |
In logistic regression models, ODI was significantly related to CVD (odds ratio [OR]=1.052; 95% confidence interval [CI]: 1.042–1.064 for all study participants; OR=1.036, 95% CI: 1.019–1.053 for individuals with SDB) in the unadjusted model (Model 1). This association was attenuated but remained significant after adjusting for EDS and other confounders (Models 3 and 4). In the fully adjusted model, ODI was independently associated with higher odds of CVD (OR=1.017; 95% CI: 1.004–1.030 for all study participants; OR=1.024, 95% CI: 1.005–1.044 for individuals with SDB) regardless of the presence or absence of EDS, and no significant interaction was observed between EDS and ODI (P for interaction>0.05). In contrast, EDS was not significantly associated with CVD in the different models. The above results are presented in Table 2 and Table S1. In addition, in our study, EDS did not mediate the association between ODI and CVD after adjusting for confounders (Figure S4).
 |
Table 2 Logistic Regression of Association Between ODI, EDS, and CVD in All Study Participants |
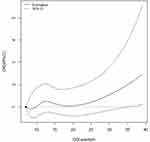
ODI, minSpO2, meanSpO2, T90, and T90%, as nocturnal hypoxia indicators of SDB extracted from the type IV sleep monitor, were included in the logistic model to detect the sensitive predictors of CVD among patients with non-sleepy SDB. In unadjusted models, ODI and meanSpO2 were both significantly associated with CVD (OR: 1.034, 95% CI: 1.017–1.052 and OR: 0.900, 95% CI: 0.845–0.959, respectively). However, in partial and fully adjusted models (Models 2 and 3), only ODI was found to be significantly correlated with CVD (OR: 1.024, 95% CI: 1.005–1.043 and OR: 1.023, 95% CI: 1.003–1.043, respectively). The results are shown in Table 3. We observed a nonlinear association between ODI and the prevalence of CVD, where the likelihood of CVD increased with ODI≥10 events/h and a markedly increasing trend was observed with ODI ≥20 events/h (reference ODI = 7.0 events/h) (Figure 1).
 |
Table 3 Odds Ratios and 95% Confidence Intervals of CVD Among Patients with Non-Sleepy SDB, According to Sleep Parameters Extracted from Type IV Sleep Monitoring |
In patients with non-sleepy SDB, subgroup analyses by sex and BMI showed that ODI was significantly associated with CVD in men and patients with a BMI ≥25 (OR: 1.029, 95% CI: 1.002–1.056; OR: 1.036, 95% CI: 1.007–1.065, respectively). Nevertheless, no significant interaction effects were observed between ODI and sex, age, BMI, or diabetes (all P interactions >0.05, Table 4).
 |
Table 4 Associations Between ODI and CVD Among Patients with Non-Sleepy SDB, Stratified by Sex, Age, BMI, and Diabetes |
Figure S5 displays the results of the mediation analyses. Among patients with non-sleepy SDB, metabolic parameters (TG, CHO, LDL-C, and HDL-C), PSQI, and the inflammatory biomarker, hsCRP, did not mediate the association between ODI and CVD.
Discussion
To our knowledge, this is the first report to determine the association between non-sleepy SDB and CVD using type IV wearable sleep monitoring in a randomly-selected community-dwelling population. Our data suggest that non-sleepy SDB is very prevalent in the community general population. ODI, typical nocturnal intermittent hypoxia indicator for SDB, was independently related to CVD, regardless of whether excessive daytime sleepiness was present. Moreover, of all SDB-related hypoxemia parameters, ODI may provide the strongest reflection of the association between non-sleepy SDB and CVD.
Most previous epidemiological studies have established the close relationship between EDS and CVD.34–38 Mazzotti et al11 used latent class analysis in 1207 participants with moderate-to-severe SDB and identified four symptom subtypes: disturbed sleep, minimally symptomatic, excessively sleepy, and moderately sleepy; the excessively sleepy subtype was the only subtype associated with increased risk of incident CVD. This evidence suggests that active management is only needed in SDB patients with EDS. Our study showed that ODI is independently associated with CVD, whether EDS exists or not. This is consistent with the results from the Wisconsin sleep cohort.39 Thus, as a significant clinical subtype, non-sleepy SDB is likely to present a potential health risk, particularly with respect to CVD. Of note, our study is not a repetition of most previous studies that only included patients with moderate-to-severe SDB or those with one or more SDB-related symptoms. In contrast, our sample was from the general population, most patients were asymptomatic or had unrecognized symptoms, and SDB severity was not classified, so our results are also more applicable to community-based general populations.
The putative mechanisms behind CVD risk are not completely understood, but they include SDB-associated intermittent hypoxia.24,40 Previous studies have shown that the metrics of nocturnal hypoxemia, such as T90%, are stronger predictors of CVD and all-cause mortality than the AHI.41–43 Indices of hypoxemia have also been demonstrated as predictors of incident atrial fibrillation44 and mortality in heart failure patients.41 However, in addition to the inconsistent findings regarding which indicators of nocturnal hypoxemia are more effective in predicting CVD, few studies have focused on patients with non-sleepy SDB from the general population. Our study showed that ODI is related to higher odds of having CVD. Other metrics of nocturnal hypoxemia, although often reported in sleep studies, have not been found to be good predictors of CVD in patients with non-sleepy SDB. In fact, except for ODI, other metrics of nocturnal hypoxemia, such as minSpO2 and T90, are not specific to SDB patients, but they may reflect underlying respiratory diseases.
The mechanism of CVD induced by intermittent hypoxia remains unclear in patients with SDB, especially in patients without EDS. Potential mechanisms include endothelial dysfunction,45 inflammation,46 and oxidative stress.47 One previous study did demonstrate that the independent association of nocturnal intermittent hypoxia with dyslipidemia predisposes patients with SDB to a higher risk of CVD.48 However, whether dyslipidemia mediates the causal association between ODI and CVD remains unclear. Our mediation effect analysis showed that none of the blood lipid profiles were mediators in the causal pathway between ODI and CVD. Many studies have suggested that inflammation is critical in the pathogenesis of CVD in SDB. CRP, as an inflammatory factor, is considered to be a mediator and marker of atherosclerotic thrombosis. However, no significant indirect effect was detected between ODI and CVD in our study. Similarly, sleep quality, measured by the PSQI, was also found not to be a mediator. Our findings suggest that additional pathophysiological mechanisms or markers linking intermittent hypoxia to CVD should be explored to elucidate potential mediators, especially in patients with non-sleepy SDB.
This study has some strengths, including the large, community-based study population and the focus on the often-overlooked non-sleepy SDB subtype. However, it does have several limitations. Firstly, due to its cross-sectional design, the study failed to assess the relationship between non-sleepy SDB and incident CVD. Thus, a long-term longitudinal follow-up of the present cohort will be required to further validate our observations. Secondly, the assessment of EDS was subjective. Nevertheless, expensive and burdensome objective measures such as maintenance of wakefulness testing or multiple sleep latency are not considered appropriate screening measures for EDS in the general population.49 Thirdly, the diagnoses of coronary artery disease, heart failure, or stroke were also obtained via self-report. However, these disease diagnoses were not arbitrary, and a medical certificate was required to confirm the diagnosis. Finally, the Type IV wearable sleep monitoring may not be precise for the assessment of SDB, even if it has been validated by an in-lab polysomnographic sleep study. Therefore, the obtained results may be potentially biased. However, a large study sample tends to decrease the risk of bias.
Conclusions
In conclusion, our study demonstrated that non-sleepy SDB is prevalent in the Chinese general population and that it is independently correlated with CVD. This suggests that in the general population, primary health care providers and health care policy makers should place importance on the identification of patients with the non-sleepy SDB subtype. ODI, an easily extracted indicator from a type IV sleep monitor, most strongly reflected the association between non-sleepy SDB and CVD.
Abbreviations
AHI, apnea-hypopnea index; BMI, body mass index; CHO, total cholesterol; CI, confidence interval; CVD, cardiovascular disease; EDS, excessive daytime sleepiness; ESS, Epworth Sleepiness Scale; HDL-C, high-density lipoprotein cholesterol; hsCRP, high-sensitivity C-reactive protein; LDL-C, low-density lipoprotein cholesterol; MeanSpO2, mean oxygen saturation; MinSpO2, lowest nocturnal oxygen saturation; ODI, oxygen desaturation index; OR, odds ratio; PSQI, Pittsburgh Sleep Quality Index; SDB, sleep-disordered breathing; T90%, percentage of sleep time with SpO2 <90%; TG, triglycerides.
Data Sharing Statement
The study data are available from the corresponding author upon reasonable request.
Acknowledgments
We thank all of the individuals who participated in this study.
Funding
This research was supported by the National Natural Science Foundation of China (Grant No. 82170098, 81870077) to Qiong Ou and CAMS Innovation Fund for Medical Sciences (CIFMS, Grant No. 2020-I2M-2-009) to Guangliang Shan.
Disclosure
The authors report no conflicts of interest.
References
1. Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687–698. doi:10.1016/S2213-2600(19)30198-5
2. Michalek-Zrabkowska M, Macek P, Martynowicz H, et al. Obstructive sleep apnea as a risk factor of insulin resistance in nondiabetic adults. Life. 2021;11(1):50. doi:10.3390/life11010050
3. Xu PH, Hui CKM, Lui MMS, et al. Incident type 2 diabetes in osa and effect of cpap treatment: a retrospective clinic cohort study. Chest. 2019;156(4):743–753. doi:10.1016/j.chest.2019.04.130
4. Yeghiazarians Y, Jneid H, Tietjens JR, et al. Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;144(3):e56–e67. doi:10.1161/CIR.0000000000000988
5. Gottlieb DJ, Punjabi NM. Diagnosis and management of obstructive sleep apnea: a review. JAMA. 2020;323(14):1389–1400. doi:10.1001/jama.2020.3514
6. Martynowicz H, Skomro R, Gać P, et al. The influence of hypertension on daytime sleepiness in obstructive sleep apnea. J Am Soc Hypertens. 2017;11(5):295–302. doi:10.1016/j.jash.2017.03.004
7. Taranto Montemurro L. The enigma of severe obstructive sleep apnea without sleepiness. J Clin Hypertens. 2019;21(3):397–398. doi:10.1111/jch.13480
8. Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122(4):352–360. doi:10.1161/CIRCULATIONAHA.109.901801
9. Oksenberg A, Goizman V, Eitan E, et al. How sleepy patients differ from non-sleepy patients in mild obstructive sleep apnea? J Sleep Res. 2022;31(1):e13431. doi:10.1111/jsr.13431
10. Eckert DJ, White DP, Jordan AS, et al. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med. 2013;188(8):996–1004. doi:10.1164/rccm.201303-0448OC
11. Mazzotti DR, Keenan BT, Lim DC, et al. Symptom subtypes of obstructive sleep apnea predict incidence of cardiovascular outcomes. Am J Respir Crit Care Med. 2019;200(4):493–506. doi:10.1164/rccm.201808-1509OC
12. Ye L, Pien GW, Ratcliffe SJ, et al. The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J. 2014;44(6):1600–1607. doi:10.1183/09031936.00032314
13. Martynowicz H, Jodkowska A, Skomro R, et al. The estimation of excessive daytime sleepiness in post-stroke patients - a polysomnographic study. Respir Physiol Neurobiol. 2019;267:1–5. doi:10.1016/j.resp.2019.05.013
14. Sánchez-de-la-Torre M, Sánchez-de-la-Torre A, Bertran S, et al. Effect of obstructive sleep apnoea and its treatment with continuous positive airway pressure on the prevalence of cardiovascular events in patients with acute coronary syndrome (isaacc study): a randomised controlled trial. Lancet Respir Med. 2020;8(4):359–367. doi:10.1016/S2213-2600(19)30271-1
15. McEvoy RD, Antic NA, Heeley E, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375(10):919–931. doi:10.1056/NEJMoa1606599
16. Peker Y, Glantz H, Eulenburg C, et al. Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea. The riccadsa randomized controlled trial. Am J Respir Crit Care Med. 2016;194(5):613–620. doi:10.1164/rccm.201601-0088OC
17. Gottlieb DJ. Sleep apnea and cardiovascular disease. Curr Diab Rep. 2021;21(12):64. doi:10.1007/s11892-021-01426-z
18. Altintas N, Riha RL. Non-sleepy obstructive sleep apnoea: to treat or not to treat? Eur Respir Rev. 2019;28(154):190031. doi:10.1183/16000617.0031-2019
19. Balcan B, Thunström E, Strollo PJ
20. Kohler M, Craig S, Nicoll D, et al. Endothelial function and arterial stiffness in minimally symptomatic obstructive sleep apnea. Am J Respir Crit Care Med. 2008;178(9):984–988. doi:10.1164/rccm.200805-717OC
21. Ayers L, Ferry B, Craig S, et al. Circulating cell-derived microparticles in patients with minimally symptomatic obstructive sleep apnoea. Eur Respir J. 2009;33(3):574–580. doi:10.1183/09031936.00107408
22. Linz D, Loffler KA, Sanders P, et al. Low prognostic value of novel nocturnal metrics in patients with osa and high cardiovascular event risk: post hoc analyses of the save study. Chest. 2020;158(6):2621–2631. doi:10.1016/j.chest.2020.06.072
23. Azarbarzin A, Sands SA, Stone KL, et al. The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the osteoporotic fractures in men study and the sleep heart health study. Eur Heart J. 2019;40(14):1149–1157. doi:10.1093/eurheartj/ehy624
24. Dewan NA, Nieto FJ, Somers VK. Intermittent hypoxemia and osa: implications for comorbidities. Chest. 2015;147(1):266–274. doi:10.1378/chest.14-0500
25. Kendzerska T, Gershon AS, Hawker G, et al. Obstructive sleep apnea and risk of cardiovascular events and all-cause mortality: a decade-long historical cohort study. PLoS Med. 2014;11(2):e1001599. doi:10.1371/journal.pmed.1001599
26. He H, Pan L, Hu Y, et al. The diverse life-course cohort (dlcc): protocol of a large-scale prospective study in China. Eur J Epidemiol. 2022. doi:10.1007/s10654-022-00894-1
27. He H, Pan L, Pa L, et al. Data resource profile: the China national health survey (CNHS). Int J Epidemiol. 2018;47(6):1734–1735f. doi:10.1093/ije/dyy151
28. Xu Y, Ou Q, Cheng Y, et al. Comparative study of a wearable intelligent sleep monitor and polysomnography monitor for the diagnosis of obstructive sleep apnea. Sleep Breath. 2022. doi:10.1007/s11325-022-02599-x
29. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi:10.1093/sleep/14.6.540
30. Drager LF, Santos RB, Silva WA, et al. OSA, short sleep duration, and their interactions with sleepiness and cardiometabolic risk factors in adults: the ELSA-Brasil study. Chest. 2019;155(6):1190–1198. doi:10.1016/j.chest.2018.12.003
31. Tsutsui JM, Xie F, Cloutier D, et al. Real-time dobutamine stress myocardial perfusion echocardiography predicts outcome in the elderly. Eur Heart J. 2008;29(3):377–385. doi:10.1093/eurheartj/ehm445
32. Sui X, Hooker SP, Lee IM, et al. A prospective study of cardiorespiratory fitness and risk of type 2 diabetes in women. Diabetes Care. 2008;31(3):550–555. doi:10.2337/dc07-1870
33. Tingley D, Yamamoto T, Hirose K, et al. Mediation: R package for causal mediation analysis; 2014.
34. Newman AB, Spiekerman CF, Enright P, et al. Daytime sleepiness predicts mortality and cardiovascular disease in older adults. The cardiovascular health study research group. J Am Geriatr Soc. 2000;48(2):115–123. doi:10.1111/j.1532-5415.2000.tb03901.x
35. Qureshi AI, Giles WH, Croft JB, et al. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology. 1997;48(4):904–911. doi:10.1212/wnl.48.4.904
36. Elwood P, Hack M, Pickering J, et al. Sleep disturbance, stroke, and heart disease events: evidence from the Caerphilly cohort. J Epidemiol Community Health. 2006;60(1):69–73. doi:10.1136/jech.2005.039057
37. Kapur VK, Resnick HE, Gottlieb DJ. Sleep disordered breathing and hypertension: does self-reported sleepiness modify the association? Sleep. 2008;31(8):1127–1132.
38. Xie J, Sert Kuniyoshi FH, Covassin N, et al. Excessive daytime sleepiness independently predicts increased cardiovascular risk after myocardial infarction. J Am Heart Assoc. 2018;7(2):e007221. doi:10.1161/JAHA.117.007221
39. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071–1078.
40. Ma L, Zhang J, Liu Y. Roles and mechanisms of obstructive sleep apnea-hypopnea syndrome and chronic intermittent hypoxia in atherosclerosis: evidence and prospective. Oxid Med Cell Longev. 2016;2016:8215082. doi:10.1155/2016/8215082
41. Oldenburg O, Wellmann B, Buchholz A, et al. Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur Heart J. 2016;37(21):1695–1703. doi:10.1093/eurheartj/ehv624
42. Smagula SF, Stone KL, Redline S, et al. Actigraphy- and polysomnography-measured sleep disturbances, inflammation, and mortality among older men. Psychosom Med. 2016;78(6):686–696. doi:10.1097/PSY.0000000000000312
43. Jung HH, Lee JH, Baek HJ, et al. Nocturnal hypoxemia and periodic limb movement predict mortality in patients on maintenance hemodialysis. Clin J Am Soc Nephrol. 2010;5(9):1607–1613. doi:10.2215/CJN.08881209
44. Gami AS, Hodge DO, Herges RM, et al. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol. 2007;49(5):565–571. doi:10.1016/j.jacc.2006.08.060
45. Sert Kuniyoshi FH, Singh P, Gami AS, et al. Patients with obstructive sleep apnea exhibit impaired endothelial function after myocardial infarction. Chest. 2011;140(1):62–67. doi:10.1378/chest.10-1722
46. Jelic S, Lederer DJ, Adams T, et al. Vascular inflammation in obesity and sleep apnea. Circulation. 2010;121(8):1014–1021. doi:10.1161/CIRCULATIONAHA.109.900357
47. Lavie L, Lavie P. Molecular mechanisms of cardiovascular disease in osahs: the oxidative stress link. Eur Respir J. 2009;33(6):1467–1484. doi:10.1183/09031936.00086608
48. Trzepizur W, Le Vaillant M, Meslier N, et al. Independent association between nocturnal intermittent hypoxemia and metabolic dyslipidemia. Chest. 2013;143(6):1584–1589. doi:10.1378/chest.12-1652
49. Randerath W, Bassetti CL, Bonsignore MR, et al. Challenges and perspectives in obstructive sleep apnoea: report by an ad hoc working group of the sleep disordered breathing group of the European respiratory society and the European sleep research society. Eur Respir J. 2018;52(3):1702616. doi:10.1183/13993003.02616-2017
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.