Back to Journals » Medical Devices: Evidence and Research » Volume 15
Incremental Healthcare Cost Implications of Retreatment Following Ureteroscopy or Percutaneous Nephrolithotomy for Upper Urinary Tract Stones: A Population-Based Study of Commercially-Insured US Adults
Authors Johnston SS, Chen BPH, Rai P, Grange P, Dwarakanathan HR, Amos T, Johnson BH , Ghosh SK, Buchholz N
Received 10 August 2022
Accepted for publication 28 October 2022
Published 10 November 2022 Volume 2022:15 Pages 371—384
DOI https://doi.org/10.2147/MDER.S384823
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Stephen S Johnston,1 Brian Po-Han Chen,2 Pragya Rai,1 Philippe Grange,3 Harikumaran R Dwarakanathan,4 Tony Amos,5 Barbara H Johnson,1 Sudip K Ghosh,2 Noor Buchholz6
1MedTech Epidemiology and Real-World Data Sciences, Johnson & Johnson, New Brunswick, NJ, USA; 2Health Economics and Market Access, Ethicon, Raritan, NJ, USA; 3Medical Affairs, Johnson & Johnson, Cincinnati, OH, USA; 4MuSigma, Bengaluru, Karnataka, India; 5Real World and Integrated Evidence Strategy, LCI, Johnson & Johnson, New Brunswick, NJ, USA; 6U-Merge Ltd. (Urology for Emerging Countries), London, UK
Correspondence: Stephen S Johnston, Real-World Data Analytics and Research, Epidemiology - MedTech Epidemiology and Real-World Data Sciences, Johnson & Johnson, 410 George Street, New Brunswick, NJ, 08901, USA, Tel +1-443-254-2222, Email [email protected]
Purpose: This study describes the incremental healthcare costs associated with retreatment among adults undergoing ureteroscopy (URS) or percutaneous nephrolithotomy (PCNL) for upper urinary tract stones (UUTS).
Patients and Methods: The IBM® MarketScan® Commercial Database was used to identify adults aged 18– 64 years with UUTS treated with URS or PCNL between January 2010 and December 2019. Patients had 12 months of continuous insurance coverage before (baseline) and after (follow-up) the first (index) procedure. The primary outcome was total all-cause healthcare costs measured over the 365-day follow-up period, not inclusive of index costs. Generalized linear models were used to estimate the incremental costs associated with retreatment within 90 (early) or 91– 365 days post-index (later) relative no retreatment. The models adjusted for demographics, comorbidities, stone(s) location, treatment setting, procedural characteristics (eg, 1-step vs 2-step PCNL) and index year.
Results: Approximately 23% (27,402/119,800) of URS patients were retreated (82% had early retreatments). The adjusted mean total cost was $10,478 (95% CI: $10,281—$10,675) for patients with no retreatment, $25,476 (95% CI: $24,947—$26,004) for early retreatment ($14,998 incremental increase, p< 0.01), and $32,868 [95% CI: $31,887—$33,850] for later retreatment ($22,391 incremental increase, p< 0.01). Approximately 36% (1957/5516) of PCNL patients were retreated (78% had early retreatments). The adjusted mean total cost was $13,446 (95% CI: $12,659—$14,273) for patients with no retreatment, $37,036 [95% CI: $34,926—$39,145]) for early retreatment ($23,570 incremental increase, p< 0.01), and $35,359 (95% CI: $32,234—$38,484) for later retreatment ($21,893 incremental increase, p< 0.01).
Conclusion: Retreatment during the first year following URS or PCNL was needed in 23% and 36% of patients, respectively, and was associated with an economic burden of up to $23,500 per patient. The high rate of retreatment and associated costs demonstrate there is an unmet need to improve mid- to long-term results in URS and PCNL.
Keywords: economic analysis, follow-up, kidney stone, post-procedure, urolithiasis
Introduction
Urinary system stone disease (USSD), or urolithiasis is increasingly common in both developed and developing countries, with country-specific prevalence ranging between 2% and 14%.1 An estimated 13% of American men and 7% of women will experience USSD during their lifetimes.2,3 Incidence of both asymptomatic and confirmed symptomatic stones has been increasing in the United States (US) for at least three decades.3–5 While individuals with USSD experience pain and decreased quality of life,6,7 often lose work time,8 and bear their share of costs for any associated medical care, the treatment of USSD also exerts a substantial burden on the US healthcare system. Direct costs of nephrolithiasis in an employed US population were estimated at $4.5 billion in 2004, with the inclusion of lost workdays elevating the total cost to $5.3 billion that year.9
Although most smaller stones (eg, <4 mm10) will pass spontaneously within one to three weeks, others may require a medical or surgical intervention for stone removal. The American Urological Association (AUA) provides separate clinical guidelines for medical and surgical stone management,11,12 with the information on stone size and location obtained from diagnostic imaging informing the treatment choice. Over time, open surgical lithotomy has essentially been supplanted by non-invasive or minimally invasive endourological approaches: extracorporeal shockwave lithotripsy (SWL), ureteroscopy (URS)/retrograde intrarenal surgery (RIRS), and percutaneous nephrolithotomy (PCNL).10,13,14
Although each of these procedures has demonstrated adequate safety and efficacy for inclusion in the AUA kidney stone guidelines, the possibilities of residual stone fragments, stone reformation, or formation of bilateral stones necessitating retreatment after an initial procedure are nontrivial. Though varying widely by individual patient risk factors, studies have reported stone recurrence rates of <11–14% at 1 year, 20%–35% at 5 years, and 31–52% at 10 years.15–17 Recent retrospective studies have estimated the risks of retreatment to range widely for SWL, URS, and PCNL (8–45% depending on the initial procedure, duration of follow-up, and definition of retreatment).8,18 These additional surgeries place obvious burdens on the affected patient. Although some instances of retreatment may not be preventable (eg, formation of bilateral stones), others represent potentially avoidable, but as yet unquantified, costs to the healthcare system.
The current study used one of the largest US real-world healthcare databases to describe the incremental healthcare costs associated with retreatment among commercially insured US adults who underwent URS or PCNL, specifically focusing on upper urinary tract stones (UUTS). These data may be used to support economic evaluation of future technologies that decrease the need for retreatment. No statistical comparisons were made between URS and PCNL.
Materials and Methods
Study Design and Data Source
This retrospective cohort study used data from the IBM® MarketScan® Commercial Database. The Commercial database houses administrative insurance claims data for a geographically diverse population of approximately 43.6 million active US employees and their dependents aged 64 or younger. This database captures data on patient demographics and health plan enrollment, along with detailed longitudinal data on diagnoses, procedures, the use and costs of physician office and other outpatient visits, hospital stays, and prescription drugs. This study was exempt from Institutional Review Board oversight because it used secondary data comprising only de-identified patient records, as dictated by Title 45 Code of Federal Regulations (45 CFR 46, 101(b)(4)).
Study Population
Adults ages 18 to 64 years who had been diagnosed with UUTS and underwent URS or PCNL between 01-January-2010 and 31-December-2019 were eligible for inclusion in the study population. The PCNL and URS cohorts were established and analyzed separately. Within each cohort, the date of the first cohort-specific procedure (URS or PCNL) defined the index date. For example, a patient who underwent URS and then PCNL would enter into the URS cohort at the time of URS, and the PCNL cohort at the time of PCNL – with each cohort time period being analyzed independently; therefore, a given patient could potentially contribute to both cohorts. Current Procedural Terminology (CPT) codes “50080” and “50081” indicated a PCNL procedure while CPT codes “52352”, “52353”, or “52356” indicated a URS procedure (including RIRS). Patients were required to have continuous medical and outpatient pharmacy insurance coverage during the 12 months before and 12 months after the index date with these intervals defining the baseline and follow-up periods, respectively. Physician-diagnosed UUTS was defined by the presence of an indicative diagnosis code from the International Classification of Diseases, Ninth or Tenth Revision, Clinical Modification (ICD-9-CM “592.0”, “592.1”, “592.9”; ICD-10-CM “N20.0”, “N20.1”, “N20.2”, “N20.9”). Patients with evidence of either stones in the lower urinary tract or kidney or bladder tumors in the baseline period were excluded.
Baseline Characteristics
Data from the baseline period were used to describe patient demographics including age in years as of the index date, sex, insurance type, and geographic region. Baseline data were also used to determine the presence of each of 31 conditions in the Elixhauser Comorbidity Index,19 evidence of prior urinary tract infection, use of pain medication, the setting of care (inpatient hospital/outpatient hospital/ambulatory surgery center) and year (2010 through 2019) of the index procedure, the location of the index stone (kidney and/or ureter) and whether or not the patient had undergone a UUTS procedure prior to the index procedure. For PCNL patients, data on stone size (>2cm vs ≤2cm, based on CPT code), 1-step vs 2-step (percutaneous access performed prior to the day of the nephrolithotomy) procedure, days between percutaneous access and nephrolithotomy (for 2-step procedures only), and type of provider (radiology only, urology only, or both) involved in the index procedure were also summarized.
Retreatment and Costs
Retreatment was defined by the presence of an ICD or CPT procedure code for SWL (CPT “50590”; ICD-9 “98.51”; ICD-10 “0TF3XZZ” or “0TF4XZZ”), URS, and/or PCNL with an accompanying anesthesia code (SWL excepted) during the follow-up period. To establish the total incremental cost associated with retreatment, the primary outcome was total all-cause healthcare costs measured over the 365-day follow-up period, not inclusive of index costs. Costs included patient out-of-pocket expenses in addition to all health plan payments on fully-adjudicated claims for inpatient and outpatient facility-based care, professional services, laboratory/imaging, and prescription medications filled at outpatient pharmacies.
Statistical Analyses
Data were analyzed separately for each cohort. Generalized linear models (GLMs) with a log link and gamma error distribution were used to quantify the adjusted incremental cost impact of retreatment.20 For the purposes of the models, patients were further divided into three mutually exclusive retreatment status groups: (1) those with no retreatment; (2) those with early (days 1–90 post-index) retreatment; and (3) those with later (days 91–365 post-index) retreatment. Patients with retreatment in both the early and later periods were categorized into the early retreatment group. A secondary set of models divided patients into two groups: (1) those with no retreatment; (2) those with any retreatment within 365 days post-index. These models adjusted for the baseline demographic characteristics, individual conditions from the Elixhauser comorbidity index, the location of the stone(s), the setting of care, and year of the index procedure. The PCNL cohort models also included stone size, 1-step vs 2-step procedure, days between percutaneous access and nephrolithotomy, and type of provider. A two-sided critical value of 0.05 was used to determine statistical significance. Statistical analyses were performed using StataSE 16 (StataCorp, College Station, Texas, US).
Results
Table 1 shows the sample size attrition associated with the application of each study inclusion and exclusion criterion, separately for the URS and PCNL cohorts. Beginning with 380,885 and 22,991 patients in the URS and PCNL cohorts, respectively, the final corresponding numbers of patients meeting all patient selection criteria were 119,800 and 5516.
 |
Table 1 Patient Selection |
URS Cohort
Of the 119,800 patients in the URS cohort, the mean (SD) age of all URS patients was 47.9 (11.1) years and 54% of patients were male (Table 2). Most URS patients presented with stones in both the kidney and ureter (52%; Table 3). Approximately 70% of the index URS procedures were performed in the outpatient hospital setting.
 |
Table 2 Baseline Demographic Characteristics in the URS Cohort, Overall and by First Year Retreatment Status |
 |
Table 3 Baseline Clinical Characteristics in the URS Cohort, Overall and by First Year Retreatment Status |
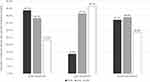
Overall, 27,402 (22.9%) had evidence of stone-related retreatment during the one-year follow-up period (22,439 with early retreatment, 4963 with later retreatment) (Figure 1). The most used modality of retreatment was URS (17,213 patients, 63% of retreated patients), followed by SWL (10,081 patients, 37%), with retreatment via PCNL being rare (716 patients, 3%). Patients with vs without retreatment were generally similar with respect to demographics but tended to have slightly higher prevalence of most selected comorbidities examined for study.
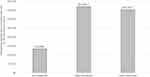
Figure 2 presents the multivariable-adjusted mean per-patient total cost for the 365-day follow-up period for URS patients with no retreatment as well as patients with early and later retreatment. The adjusted mean total cost was $10,478 (95% CI: $10,281—$10,675) for patients with no retreatment, 2.4 times higher in patients with early retreatment ($25,476 [95% CI: $24,947—$26,004]), and 3.1 times higher in patients with later retreatment ($32,868 [95% CI: $31,887—$33,850]). Retreatment increased the adjusted mean costs per patient by $14,998 (95% CI: $14,507—$15,488) and $22,391 (95% CI: $21,445—$23,336), respectively, for patients with early and later retreatments (all p<0.01). In the secondary analyses, any retreatment during follow-up was associated with an incremental increase of $16,369 (95% CI: $15,905—$16,832).
PCNL Cohort
Of the 5516 patients in the PCNL cohort, the mean (SD) age of all PCNL patients was 50.6 (11.4) years and 45% of patients were male (Table 4). Nearly 80% of PCNL patients had stones located in the kidney and approximately 20% had stones in both the kidney and ureter. Most stones (70%) were greater than 2 cm in size (Table 5). Approximately 65% of the index PCNL procedures were performed in the outpatient hospital setting. The percutaneous access procedure most often involved both a radiologist and urologist (53%) and was performed on the same day as the index procedure in 78% of patients.
 |
Table 4 Baseline Demographic Characteristics in the PCNL Cohort, Overall and by First Year Retreatment Status |
 |
Table 5 Baseline Clinical Characteristics in the PCNL Cohort, Overall and by First Year Retreatment Status |
Overall, 1957 (35.5%) had evidence of stone-related retreatment during the one-year follow-up period (1527 with early retreatment, 430 with later retreatment) (Figure 3). The most used modality of retreatment was URS (760 patients, 39% of retreated patients), followed by PCNL (726 patients, 37%), and SWL (557 patients, 29%). PCNL was proportionally more common among patients with early retreatment (43.7%) as compared with those with later retreatment (13.5%) (Figure 3). As with the URS cohort, patients in the PCNL cohort with vs without retreatment were generally similar with respect to demographics but tended to have slightly higher prevalence of most selected comorbidities examined for study.
Figure 4 presents the multivariable-adjusted mean per-patient total healthcare cost for the 365-day follow-up period for PCNL patients with no retreatment as well as patients with early and later retreatment. The adjusted mean total cost was $13,446 (95% CI: $12,659—$14,273) for patients with no retreatment, 2.8 times higher in patients with early retreatment ($37,036 [95% CI: $34,926—$39,145]), and 2.6 times higher in patients with later retreatment ($35,359 [95% CI: $32,234—$38,484]). Retreatment increased the adjusted mean costs per patient by $23,570 (95% CI: $21,411—$25,728) and $21,893 893 (95% CI: $18,770—$25,015), respectively, for patients with early and later retreatments (all p<0.01). In the secondary analyses, any retreatment during follow-up was associated with an incremental increase of $23,196 (95% CI: $21,272—$25,121). Additional model results are provided in Supplemental Tables 1 and 2.
Discussion
Although other researchers have estimated the overall economic burden of UUTS and USSD in the US, to our knowledge this is the first study to assess the direct economic consequences of retreatment for patients initially treated with URS or PCNL. Results from our study demonstrate that retreatment after either URS or PCNL confers a 2.4-fold to 3.1-fold increase in the mean total 1-year healthcare cost per patient, even after adjusting for potential confounders. Use of URS was more than 20 times more common than PCNL; however, regardless of which type of procedure was used initially, mean total costs increased significantly for patients with retreatment within the first 90 days post-procedure and for those with retreatment later in the first year after the index procedure.
The cost of retreatment has especially important implications given that retreatment was common in both cohorts (29.7% for URS and 35.5% for PCNL), higher than prior estimates of general stone recurrence rates, which range from <11%–14%, at 1 year. Though few studies have comprehensively examined risk factors associated for retreatment after URS or PCNL, previous studies have implicated residual stone fragments after an initial procedure in the need for retreatment.21,22 Emmott et al reported a study of 658 patients undergoing PCNL in a single institution from August 2008 through December 2013, with median follow-up of 396 days.21 Of these patients, 45% had fragments 1mm or larger (55% stone-free rate); among those with fragments >4mm, 28% required reintervention while among those with fragments ≤4 mm, 17% required reintervention. Iremashvili et al also reported that among 781 patients undergoing URS, patients with residual fragments >2mm were at increased risk of repeat surgery over a median follow-up of 4.2 years.22 In addition to residual stone fragments, early stone recurrence or development of bilateral stones in UUTS patients may also contribute to the need for retreatment; future research examining a larger, more multifactorial set risk factors for retreatment would be useful. Although we were unable to distinguish the specific circumstances necessitating each retreatment, it is unlikely that the incremental cost of retreatment would vary substantially depending on whether it is due to residual fragments, stone recurrence, or stones on the contralateral side. Application of our estimates to populations in which the proportional contributions of the various underlying causes of retreatment are known may provide an accurate aggregate estimate of potentially avoidable retreatment costs. Ultimately, the increasing incidence of UUTS in the US and globally suggests that the number of patients at risk for retreatment, regardless of cause, will also continue increasing.
Though we examined a different timeframe and outcome definition, our results are generally consistent with those of Scales et al (2014),8 who used the MarketScan database to describe the incremental healthcare costs associated with unplanned, high-acuity follow-up visits within 30 days after URS, PCNL, or SWL between 2003 and 2011. They reported that such visits were associated with healthcare costs ranging from $23,436 among patients who underwent URS to $47,618 among patients who underwent PCNL. Importantly, Scales et al did not consider follow-up hospital admissions in which PCNL occurred to constitute an unplanned visit, as these may have constituted a planned “second look procedure”. However, such visits nevertheless contribute to the overall burden of retreatment captured in the present study.
The pattern of retreatment was markedly different between the URS and PCNL cohorts, with URS patients being very unlikely to undergo retreatment with PCNL (only 716 of the total 119,800 patients), whereas PCNL had roughly equal numbers of patients undergoing retreatment with PCNL (726 patients) and URS (760 patients). Use of SWL for retreatment was similar between the URS and PCNL cohorts, constituting 36.8% and 28.5% of retreatments, respectively. Though we did not attempt to formally test for statistically significant differences in cost patterns across the PCNL and URS cohorts, the within-cohort patterns of costs associated with early vs later retreatment differed slightly, with early retreatment being associated with slightly higher total healthcare costs (though not statistically significantly) than later retreatment for the PCNL cohort, whereas the opposite trend was seen in the URS cohort. This may be partially explained by the circumstance that the modality of retreatment after PCNL was predominantly PCNL (43.7%) for those with early retreatment whereas it was SWL (46.7%) for those with later retreatment; in the URS cohort, however, the modalities differed comparatively less across the early vs later retreatment groups. Future research examining the association of retreatment modality with subsequent economic and clinical outcomes could be informative, especially between SWL and URS. However, in order to minimize the cost burden of retreatment, an opportunity exists to address current technological challenges to optimize the success of single procedure UUTS treatments.
Particular data and methodological limitations provide important context for interpreting results from this study. First, as noted above, we were unable to distinguish the specific cause of retreatment, some of which may be avoidable, while others by be unavoidable; however, the incremental costs of retreatment are unlikely to vary substantially by cause. We are also unaware of any very large databases with both healthcare cost data and clinical data that may be used to distinguish the specific cause of retreatment. Second, the study database lacks clinical information that may be of interest for future research, such as initial stone size, initial stone type (eg, struvite), and presence and size of residual fragments, among others. Areas for future research include examination of endoscopic combined intra-renal surgery, simultaneous bilateral procedures, and use of JJ stents in URS, all of which may affect the stone free rates and/or the risk of complications. Finally, these results reflect the experience of a commercially insured adult population in the US and may not generalize directly to patients outside of the US, uninsured patients, or individuals with other types of insurance coverage such as Medicare.
Conclusion
In this large, retrospective cohort study of patients undergoing URS or PCNL for UUTS, retreatment during the first year following URS or PCNL was needed in 23% and 36% of patients, respectively, and was associated with an economic burden of up to $23,500 per patient. The high rate of retreatment and associated costs demonstrate there is an unmet need to improve mid- to long-term results in URS and PCNL.
Abbreviations
AUA, American Urological Association; CPT, Current Procedural Terminology; GLM, Generalized linear models; ICD-10-CM/PCS, International Classification of Diseases, Tenth Revision, Clinical Modification/Procedure Classification System; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; PCNL, percutaneous nephrolithotomy; RIRS, retrograde intrarenal surgery; SWL, extracorporeal shockwave lithotripsy; URS, ureteroscopy; UUTS, upper urinary tract stones; US, United States.
Data Sharing Statement
The study data are commercially available under license to the MarketScan databases.
Ethics Approval and Informed Consent
This study was exempt from Institutional Review Board oversight because it used secondary data comprising only de-identified patient records, as dictated by Title 45 Code of Federal Regulations (45 CFR 46, 101(b)(4)).
Acknowledgments
The authors would like to thank Sally Wade (Wade Outcomes Research and Consulting, Salt Lake City) for medical writing assistance.
Author Contributions
All authors:
- Made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas.
- Have drafted or written, or substantially revised or critically reviewed the article.
- Have agreed on the journal to which the article will be submitted.
- Reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage.
- Agree to take responsibility and be accountable for the contents of the article.
Funding
This study was funded by Johnson & Johnson. As indicated in the Competing interests section below, several co-authors are employees of Johnson & Johnson.
Disclosure
Stephen S. Johnston, Brian Po-Han Chen, Philippe Grange, Tony Amos, Barbara H. Johnson, and Sudip K. Ghosh are employees and stockholders of Johnson & Johnson. Pragya Rai was a contract postdoctoral fellow at the time of this research. Harikumaran R. Dwarakanathan was employed by Mu Sigma at the time of this research; Mu Sigma was paid by Johnson & Johnson for data programming services. Noor Buchholz reports no conflicts of interest in this work.
References
1. Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol. 2010;12(2–3):e86–96.
2. Chung KJ, Kim JH, Min GE, et al. Changing trends in the treatment of nephrolithiasis in the real world. J Endourol. 2019;33(3):248–253. doi:10.1089/end.2018.0667
3. Chen ZPM, Bird VY, Bird VY. Prevalence of kidney stones in the USA: the national health and nutrition evaluation survey. J Clin Urol. 2019;12(4):296–302. doi:10.1177/2051415818813820
4. Kittanamongkolchai W, Vaughan LE, Enders FT, et al. The changing incidence and presentation of urinary stones over 3 Decades. Mayo Clin Proc. 2018;93(3):291–299. doi:10.1016/j.mayocp.2017.11.018
5. Tundo G, Vollstedt A, Meeks W, Pais V. Beyond prevalence: annual cumulative incidence of kidney stones in the United States. J Urol Jun. 2021;205(6):1704–1709. doi:10.1097/JU.0000000000001629
6. Bryant M, Angell J, Tu H, Goodman M, Pattaras J, Ogan K. Health related quality of life for stone formers. J Urol. 2012;188(2):436–440. doi:10.1016/j.juro.2012.04.015
7. Bensalah K, Tuncel A, Gupta A, Raman JD, Pearle MS, Lotan Y. Determinants of quality of life for patients with kidney stones. J Urol. 2008;179(6):2238–43;discussion 2243. doi:10.1016/j.juro.2008.01.116
8. Scales CD Jr, Saigal CS, Hanley JM, Dick AW, Setodji CM, Litwin MS; NIDDK Urologic Diseases in America Project. The impact of unplanned postprocedure visits in the management of patients with urinary stones. Surgery. 2014;155(5):769–775. PMID: 24787103; PMCID: PMC4586158. doi:10.1016/j.surg.2013.12.013
9. Saigal CS, Timilsina AR, Timilsina AR, Urologic Diseases in America Project T. Direct and indirect costs of nephrolithiasis in an employed population: opportunity for disease management? Kidney Int. 2005;68(4):1808–1814. doi:10.1111/j.1523-1755.2005.00599.x
10. Khan SR, Pearle MS, Robertson WG, et al. Kidney stones. Nat Rev Dis Primers. 2016;2:16008. PMID: 27188687; PMCID: PMC5685519. doi:10.1038/nrdp.2016.8
11. Pearle MS, Goldfarb DS, Assimos DG, et al. Medical management of kidney stones: AUA guideline. J Urol. 2014;192(2):316–324. doi:10.1016/j.juro.2014.05.006
12. Assimos D, Krambeck A, Miller NL, et al. Surgical management of stones: American Urological association/endourological society guideline, PART I. J Urol. 2016;196(4):1153–1160. doi:10.1016/j.juro.2016.05.090
13. Fontenelle LF, Sarti TD. Kidney Stones: treatment and Prevention. Am Fam Physician. 2019;99(8):490–496.
14. Large T, Assmus MA, Valadon C, et al. A multi-institutional review of single-access percutaneous nephrolithotomy for complex staghorn stones. Eur Urol Focus. 2020;7:1170–1175. doi:10.1016/j.euf.2020.11.005
15. Wang K, Ge J, Han W, et al. Risk factors for kidney stone disease recurrence: a comprehensive meta-analysis. BMC Urol. 2022;22(1):62. PMID: 35439979; PMCID: PMC9017041. doi:10.1186/s12894-022-01017-4
16. Rule AD, Lieske JC, Li X, Melton LJ 3rd, Krambeck AE, Bergstralh EJ. The ROKS nomogram for predicting a second symptomatic stone episode. J Am Soc Nephrol. 2014;25(12):2878–2886. PMID: 25104803; PMCID: PMC4243346. doi:10.1681/ASN.2013091011
17. Uribarri J, Oh MS, Carroll HJ. The first kidney stone. Ann Intern Med. 1989;111(12):1006–1009. doi:10.7326/0003-4819-111-12-1006
18. Bowen DK, Song L, Faerber J, Kim J, Scales CD
19. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi:10.1097/00005650-199801000-00004
20. Greene WH. Econometric Analysis.
21. Emmott AS, Brotherhood HL, Paterson RF, Lange D, Chew BH. Complications, re-intervention rates, and natural history of residual stone fragments after percutaneous nephrolithotomy. J Endourol. 2018;32(1):28–32. doi:10.1089/end.2017.0618
22. Iremashvili V, Li S, Penniston KL, Best SL, Hedican SP, Nakada SY. Role of residual fragments on the risk of repeat surgery after flexible ureteroscopy and laser lithotripsy: single center study. J Urol. 2019;201(2):358–363. doi:10.1016/j.juro.2018.09.053
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.