Back to Journals » Clinical Ophthalmology » Volume 11
Incidence of outer retinal tubulation in eyes with choroidal neovascularization under intravitreal anti-vascular endothelial growth factor therapy in a Japanese population
Authors Takagi S, Mandai M, Miyamoto N, Nishida A, Hirami Y, Uyama H, Yamamoto M, Takahashi M, Tomita G , Kurimoto Y
Received 9 February 2017
Accepted for publication 1 June 2017
Published 28 June 2017 Volume 2017:11 Pages 1219—1225
DOI https://doi.org/10.2147/OPTH.S134338
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Seiji Takagi,1–3 Michiko Mandai,1,4 Noriko Miyamoto,1,2 Akihiro Nishida,1,2 Yasuhiko Hirami,1,2 Hirofumi Uyama,1,2 Midori Yamamoto,1,2 Masayo Takahashi,1,2,4 Goji Tomita,3 Yasuo Kurimoto1,2
1Department of Ophthalmology, Kobe City Medical Center General Hospital, 2Department of Translational Research, Division of Ophthalmology, Institute of Biomedical Research and Innovation, Kobe, Hyogo, 3Department of Ophthalmology, Toho University Ohashi Medical Center, Meguro-ku, Tokyo, 4RIKEN Center for Developmental Biology, Kobe, Hyogo, Japan
Purpose: The purpose of this study was to investigate the occurrence of outer retinal tubulation (ORT) among patients with different types of choroidal neovascularization (CNV) over time.
Materials and methods: In this retrospective chart review, disease type was classified as typical age-related macular degeneration (t-AMD), polypoidal choroidal vasculopathy (PCV), retinal angiomatous proliferation (RAP), or myopic CNV (mCNV). Spectral domain-optical coherence tomography (SD-OCT) images were evaluated for the appearance of ORT and subretinal fibrosis and fluid. Furthermore, the association of the presence of ORT with clinical data and OCT findings was investigated.
Results: Among the 136 eyes studied, the overall rates of occurrence of ORT were 7.8%, 18.8%, and 31.6% after 12, 24, and 36 months from baseline, respectively. Among patients with t-AMD, RAP, and mCNV, the occurrence of ORT increased soon after the initial visit. In contrast, among patients with PCV, the occurrence of ORT increased slowly over time. Patients with and without ORT – ORT(+) and ORT(-) groups, respectively – differed significantly in terms of sex ratio and presence of intraretinal fluid at the initial visit and presence of subretinal fibrosis at 3 years from baseline. The ORT(+) group exhibited lower visual acuity (VA; 0.67±0.43) than that of the ORT(-) group (0.41±0.36; P<0.001).
Conclusion: The occurrence of ORT tended to increase more slowly among eyes diagnosed with PCV than among eyes with other types of CNV.
Keywords: optical coherence tomography, retinal degeneration, subretinal fibrosis
Introduction
Outer retinal tubulation (ORT) is a branching tubular structure change observed in choroidal neovascularization (CNV) secondary to age-related macular degeneration (AMD),1,2 retinitis pigmentosa, and various other degenerative conditions.3,4 ORT – which is not detectable solely by biomicroscopy – was first described by Zweifel et al,1 using optical coherence tomography (OCT). ORT has now come to be more commonly recognized with spectral domain-optical coherence tomography (SD-OCT), which has a higher resolution than biomicroscopy and is used clinically worldwide.
ORT is indicated by circular or oval highly reflective boundaries in the outer nuclear layer, often with a highly reflective material inside.1 It is important to distinguish ORT from subretinal fluid (SRF) on OCT images, because SRF – observed mainly in the inner plexiform layer on OCT images – requires treatment, whereas ORT – which is not an exudative change – does not.2,5,6 Recently, Litts et al7 reported that the hyperreflective ORT border observed on SD-OCT images corresponds to a combination of the external limiting membrane (ELM) within degenerating inner segments and mitochondria. Moreover, the authors reported the ORT to be composed of degenerate photoreceptors (almost exclusively cones) and Müller cells.8
The incidence of ORT among patients with AMD is continuously increasing, despite treatment with anti-vascular endothelial growth factors (VEGFs).2,6,9 However, the occurrence of ORT over time in each disease type is not clear, particularly in terms of its incidence among patients with polypoidal choroidal vasculopathy (PCV), a condition that is highly prevalent among the Japanese and other Asian populations. The aims of this study were to investigate the prevalence of ORT in each type of CNV among Japanese patients undergoing anti-VEGF therapy and to investigate the relationship of ORT development with clinical background factors and OCT findings.
Materials and methods
Subjects
The ethics committee of Kobe City Medical Center General Hospital reviewed and approved this retrospective study (approval date, September 17, 2015; serial number, 15073). The committee waived the requirement for informed consent for this observational study involving the use of medical records. The confidentiality of patient data shall be maintained.
Patients receiving anti-VEGF therapy for treatment-naïve subfoveal CNV diagnosed between 2009 and 2012 and followed up for a minimum period of 3 years were enrolled. We defined time 0 as the time of initial visit. All patients were >50 years of age, in accordance with the criteria for anti-VEGF therapy in Japan. From 2009 to 2015, our routine treatment regimen for patients with CNV involved 3-monthly injections of anti-VEGF drugs (ranibizumab or aflibercept, 0.5 mg or 0.05 mL, respectively), followed by subsequent injections pro re nata or every 2 months, depending on the exudative condition. From 2009 to 2011, photodynamic therapy was administered in cases of occult CNV under the fovea, lesion size <5,000 μm in the greatest linear dimension and Snellen equivalent <20/40; from 2012 to 2016, patients who exhibited resistance to anti-VEGF therapy were also administered photodynamic therapy. The exclusion criteria for this study were poor OCT image quality and presence of other potentially confounding retinal pathologies, such as retinal vein occlusion, diabetic retinopathy, and retinal dystrophy.
At each visit, every patient underwent a comprehensive ocular examination, including evaluation of best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, dilated fundoscopy, and SD-OCT. SD-OCT images were acquired by high-density cross-line imaging using the Heidelberg Spectralis scanner (Heidelberg Engineering, Heidelberg, Germany). BCVA was evaluated using Landolt C charts; these values were then converted to the logarithm of the minimum angle of resolution equivalent. Data collected from medical charts included age, sex, and visual acuities at baseline and final visit.
Clinical analysis
We retrospectively reviewed the medical records of consecutive patients who had consulted two physicians (S.T. and N.M.). All patients had undergone fluorescein angiography (FA) and indocyanine green angiography (ICGA) at baseline and upon recurrence or worsening of the exudative condition.
Disease type was classified as typical age-related macular degeneration (t-AMD), PCV, retinal angiomatous proliferation (RAP), or myopic CNV (mCNV), with each disease defined as follows: PCV was diagnosed if eyes presented an orange nodule on the fundus or branching vascular networks and/or terminating polypoidal lesions upon ICGA; RAP was diagnosed if eyes presented a form of neovascular proliferation originating from deep retinal layers, expanding to create a retinal–choroidal anastomosis; t-AMD was diagnosed if eyes presented exudative neovascularization not consistent with PCV or RAP; and mCNV was diagnosed if eyes with high myopia (≥−5 D) exhibited subfoveal–juxtafoveal neovascularization.
On SD-OCT images, ORT was defined as a hyperreflective border located in the outer nuclear layer; the presence of this finding even in a single slice was considered as meeting the criteria for diagnosis. The presence of ORT was analyzed throughout the follow-up period, and onset of ORT was defined as the day on which ORT was recognized on an SD-OCT cross-scan. The presence and location of SRF was graded at each visit. Furthermore, we investigated the relationship between the presence of subretinal fibrosis and the development of ORT. Subretinal fibrosis was defined by a relatively homogeneous hyperreflective region that was detected by OCT and underwent no structural changes for >6 months, regardless of treatment.
Statistical analysis
We analyzed the statistical significance of differences in each of the baseline clinical background factors and OCT features at the initial visit between patients with and without ORT – designated as the ORT(+) and ORT(−) groups, respectively. Fisher’s exact test was used for comparison of proportions, and the Mann-Whitney U test was used for comparison of mean values. Statistical analyses were performed using SPSS version 21.0 (SPSS Science, Chicago, IL, USA), and a two-sided P-value <0.05 was considered as statistically significant.
Results
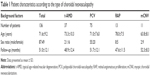
A total of 148 eyes of 148 patients were enrolled, of which 12 eyes were excluded because of poor image quality. Thus, this study finally included 136 eyes of 136 patients. The disease groups were t-AMD (37 eyes), PCV (75 eyes), RAP (13 eyes), and mCNV (11 eyes). The patient characteristics and treatments are summarized in Table 1. The mean patient age at baseline was 71.6±9.2 years, and the mean follow-up period was 51.0±12.1 months.
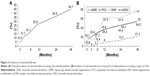
The frequency of ORT continuously increased under anti-VEGF treatment during the follow-up period. The overall rates of occurrence of ORT after 12, 24, and 36 months from baseline were 7.8%, 18.8%, and 31.6%, respectively (Figure 1).
ORT appeared after a mean follow-up period of 20.4±15.0 months. The occurrence of ORT in each type of CNV is shown in Figure 1A. Patients with t-AMD, RAP, and mCNV exhibited similar rates of occurrence of ORT, with the rates increasing soon after first examination and reaching ~20%, 40%, and 50% after 12, 24, and 36 months from baseline, respectively (Figure 1B). In contrast, patients with PCV exhibited almost no occurrence of ORT in the first 3 months; however, the rate of occurrence of ORT increased slowly over time, reaching 5.3%, 9.3%, and 21% after 12, 24, and 36 months from baseline, respectively (Figure 1B).
Relative to the PCV group, the t-AMD, RAP, and mCNV groups each exhibited significantly higher rates of occurrence of ORT at 12, 24, and 36 months from baseline (P<0.001, all).
Figure 2 shows representative cases of ORT, with the development of subretinal hyperreflective lesions in eyes with type-1 CNV with an overlying subretinal hyperreflective material (SHRM) of PCV in Figure 2A and a mixed lesion with type-1 and −2 CNV components of t-AMD in Figure 2B. In a patient with PCV, subretinal fibrosis had formed after scarring of the SHRM at 22 months after the first visit, with open ORT having developed at the same time. In a patient with t-AMD, subretinal fibrosis had formed as a result of CNV scarring – with or without retinal pigment epithelium (RPE) coverage – within 9 months after the initial visit, and ORT was observed 6 months later.
Therefore, we considered subretinal fibrosis as representing a well-demarcated, relatively homogeneous hyperrefractive region, regardless of size, exhibiting no regression for >6 months regardless of treatment, as shown in Figure 3. We evaluated the occurrence of subretinal fibrosis on the basis of this definition. The total rates of occurrence of subretinal fibrosis at 12, 24, and 36 months from baseline were 25.9%, 34.8%, and 44.7%, respectively (Figure 3A). The incidence of subretinal fibrosis, too, increased continuously over the follow-up period, even during anti-VEGF treatment. Similar to ORT, the occurrence of subretinal fibrosis in the t-AMD, RAP, and mCNV groups was observed early during the follow-up period, whereas in the PCV group, the incidence of subretinal fibrosis increased slowly over time (Figure 3B).
In cases where ORT was detected with subretinal fibrosis, ORT had developed after occurrence of the fibrotic scar in all cases and had occurred within 6 months after development of subretinal fibrosis in 52% of the cases.
The functional outcomes of the entire cohort and each disease group were as follows. The mean BCVAs at the baseline and last visit, respectively, were 0.50±0.41 and 0.58±0.48 in the entire cohort, 0.66±0.45 and 0.65±0.47 in the t-AMD group, 0.35±0.31 and 0.39±0.37 in the PCV group, 0.70±0.42 and 1.18±0.40 in the RAP group, and 0.71±0.39 and 0.86±0.51 in the mCNV group.
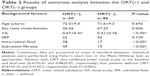
The ORT(+) and ORT(−) groups exhibited significant differences in sex ratio (P=0.006), VA (P<0.001) at 36 months from baseline, and presence of intraretinal fluid at the initial visit (P<0.001) and subretinal fibrosis (P<0.001); however, there was no significant difference in age or presence of SRF at the initial visit (P=0.729; Table 2).
Discussion
Here, we have reported the prevalence of ORT in four types of CNV diseases among Japanese patients undergoing anti-VEGF therapy. The overall rate of occurrence of ORT had increased over a period of 3 years under anti-VEGF treatment. Moreover, the rate of occurrence of ORT could be linked to the occurrence of subretinal fibrosis.
Numerous studies have reported that ORT formation is correlated with the presence of subretinal fibrosis.1,2,5,6,10 In the present study, areas of subretinal fibrosis appeared to exhibit RPE impairment, as indicated by the disruption and/or loss of the homogenous hyperrefractive line in the outer retina in SD-OCT images. In fibrotic scars with RPE impairment, some photoreceptors might exhibit loss of lateral integration with degenerating neighboring cells.1 In some cases in the present study, subretinal fibrosis was observed to have developed during the process of ORT formation; in other cases, ORT development was delayed relative to that of subretinal fibrosis. In case of the latter, the free edges curved continuously until they formed new lateral connections, resulting in the formation of a completely closed tube (Figure 3).11 We found that ORT had developed after occurrence of the fibrotic scar in all cases and within 6 months after development of subretinal fibrosis in 52% of cases.
The rate of occurrence of ORT in the t-AMD, RAP, and mCNV groups increased from an early stage, reaching a plateau by the end of 3 years; in contrast, in the PCV group – which was the largest group in this study – the rate of occurrence of ORT increased slowly over time, reaching 20% in 3 years and still continuing to increase after 3 years.
To our knowledge, this is the first study to describe the occurrence of ORT over time among patients with PCV, a highly prevalent condition among the Japanese and other Asian population. PCV is typically an abnormal vascular network with polyps under the RPE, and a large part of the PCV might not accompany type-2 CNV.12,13 Type-2 CNV – which is not covered by the RPE – is often progressive, and the outer retina is easily injured, which might result in the formation of a fibrotic scar in the subretinal space and cause a decrease in the activity of the CNV under anti-VEGF therapy.14 This could indicate that, relative to other types of CNV diseases, the chances of formation of fibrotic scars in PCV would be lesser and/or delayed.
In the present study, the rate of occurrence of ORT increased progressively over the follow-up period under anti-VEGF treatment. Several studies have also reported that the prevalence of ORT increases under anti-VEGF treatment.2,9,10 A possible reason for this trend is that the treatment itself might promote the development of ORT. An increase in geographic atrophy under anti-VEGF treatment was also observed in a large cohort clinical study,15 which might indicate that anti-VEGF treatment increases the risk of RPE damage. Further investigation is needed to prevent poor visual outcomes because of ORT formation after anti-VEGF treatment.9,10
In the present study, upon comparing background factors related to occurrence of ORT between the ORT(+) and ORT(−) groups, we found significant intergroup differences in sex ratio and presence of intraretinal fluid. The proportion of women in the mCNV group was high (81.8%), and the overall incidence of ORT among women (36.0%) was markedly higher than that among men. The difference in the presence of intraretinal fluid between patients with and without ORT in the present study is consistent with the findings of previous studies on the clinical characteristics related to ORT formation.5,6 The presence of intraretinal fluid has also been reported to be a risk factor for the formation of fibrotic scars.12 The ORT(+) group in the present study exhibited significantly worse visual acuities relative to the ORT(−) group, both at initial and final examination. Additionally, while VA was preserved over time in the ORT(−) group, it worsened over time in the ORT(+) group. This worsening of VA is known to contribute to poor prognosis. These results are consistent with those of previous reports.2,6,10,11 However, whether ORT loses its function as a photoreceptor, per se, is not clear. The ORT is thought to be a photoreceptor on the basis of pathological findings;7 however, visual function at locations where ORT is detected on OCT images is not yet well established. Further investigations on the potential function of the ORT as a photoreceptor and its role in onset of visual impairment are required.
One of the limitations of a study of this nature is that the rate of occurrence of ORT varies according to its definition – that is, ORTs could be too small to identify in a single OCT image. In some cases, ORTs of ~40 μm width and height have been reported.1 Moreover, in case of completely round, hyperreflective regions – which was the definition of ORT in the present study – the ORT might not be delineated in an OCT slice; this has been reported in a previous study as one of the reasons for discrepancies in the rate of occurrence of ORT.2 In the present study, there were many small-sized ORTs, and it is likely that, in some cases, the ORT was not completely delineated. While the ratios of occurrence rates among the different groups would not change markedly, the rate of occurrence of ORT would vary depending on the definition of ORT. Furthermore, this study was limited by its retrospective nature and small sample size for some types of AMD. To further our understanding of ORT formation and its effect on long-term visual outcomes, larger and more prolonged longitudinal case studies are needed.
Conclusion
In this study, we established the rate of occurrence of ORT over time for each type of CNV, including PCV, a condition that is rare among Europeans and Americans. The present results should be further confirmed, especially in Asian countries, including Japan, where the rate of occurrence of PCV among patients with AMD is high.13,14 A better understanding of photoreceptor changes – such as ORT – that occur in the presence of RPE dysfunction could lead to a better understanding of the retinal degenerative process.
Disclosure
The authors report no conflicts of interest in this work.
References
Zweifel SA, Engelbert M, Laud K, Margolis R, Spaide RF, Freund KB. Outer retinal tubulation: a novel optical coherence tomography finding. Arch Ophthalmol. 2009;127(12):1596–1602. | ||
Dirani A, Gianniou C, Marchionno LM, Decugis D, Mantel I. Incidence of outer retinal tubulation in ranibizumab-treated age-related macular degeneration. Retina. 2015;35(6):1166–1172. | ||
Iriyama A, Aihara Y, Yanagi Y. Outer retinal tubulation in inherited retinal degenerative disease. Retina. 2013;33(7):1462–1465. | ||
Goldberg NR, Greenberg JP, Laud K, Tsang S, Freund KB. Outer retinal tabulation in degenerative retinal disorders. Retina. 2013;33(9):1871–1876. | ||
Hua R, Liu L, Hu Y, Chen L. The occurrence and progression of outer retinal tubulation in Chinese patients after intravitreal injections of ranibizumab. Sci Rep. 2015;5:7661. | ||
Iaculli C, Barone A, Scudieri M, Giovanna Palumbo M, Delle Noci N. Outer retinal tubulation: characteristics in patients with neovascular age-related macular degeneration. Retina. 2015;35(10):1979–1984. | ||
Litts KM, Ach T, Hammack KM, et al. Quantitative analysis of outer retinal tubulation in age-related macular degeneration from spectral-domain optical coherence tomography and histology. Invest Ophthalmol Vis Sci. 2016;57(6):2647–2656. | ||
Litts KM, Messinger JD, Dellatorre K, Yannuzzi LA, Freund KB, Curcio CA. Freund clinicopathological correlation of outer retinal tubulation in age-related macular degeneration. JAMA Ophthalmol. 2015;133(5):609–612. | ||
Lee JY, Folgar FA, Maguire MG, et al; CATT Research Group. Outer retinal tubulation in the comparison of age-related macular degeneration treatments trials (CATT). Ophthalmology. 2014;121(12):2423–2431. | ||
Faria-Correia F, Barros-Pereira R, Queirós-Mendanha L, et al. Characterization of neovascular age-related macular degeneration patients with outer retinal tubulations. Ophthalmologica. 2013;229(3):147–151. | ||
Schaal KB, Freund KB, Litts KM, Zhang Y, Messinger JD, Curcio CA. Outer retinal tabulation in advanced age-related macular degeneration: optical coherence tomographic findings correspond to histology. Retina. 2015;35(7):1339–1350. | ||
Uyama M, Matsubara T, Fukushima I, et al. Idiopathic polypoidal choroidal vasculopathy in Japanese patients. Arch Ophthalmol. 1999;117(8):1035–1042. | ||
Uyama M, Wada M, Nagai Y, et al. Polypoidal choroidal vasculopathy: natural history. Am J Ophthalmol. 2002;133(5):639–648. | ||
Daniei E, Toth CA, Grunwald JE, et al; Comparison of Age-related Macular Degeneration Treatments Trials Research Group. Risk of scar in the comparison of age-related macular degeneration treatments trial. Ophthalmology. 2014;121(3):656–666. | ||
Grunwald JE, Daniel E, Huang J, et al; CATT Research Group. Risk of geographic atrophy in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2014;121(1):150–161. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.