Back to Journals » International Journal of General Medicine » Volume 15
Incidence and Predictors of Ventilator-Associated Pneumonia Among Adult Intubated Patients in Bahir Dar Specialized Hospitals, 2021: A Retrospective Follow-Up Study
Authors Belay CM, Zewale TA , Amlak BT, Abebe TG , Hailu G
Received 28 June 2022
Accepted for publication 19 October 2022
Published 11 November 2022 Volume 2022:15 Pages 8173—8182
DOI https://doi.org/10.2147/IJGM.S380301
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Chernet Manaye Belay,1 Taye Abuhay Zewale,2 Baye Tsegaye Amlak,3 Tiruayehu Getinet Abebe,4 Getachew Hailu2
1Department of Nursing, Tibebe Ghion Specialized Hospital, Bahir Dar University, Bahir Dar, Ethiopia; 2Department of Epidemiology and Biostatistics, Bahir Dar University, Bahir Dar, Ethiopia; 3Department of Nursing, Debre Markos University, Debre Markos, Ethiopia; 4Department of Public Health, Debre Tabor University, Debre Tabor, Ethiopia
Correspondence: Baye Tsegaye Amlak, Department of Nursing, Debre Markos University, Debre Markos, Ethiopia, Tel +251 948702095, Email [email protected] Chernet Manaye Belay, Department of Nursing, Tibebe Ghionspecialized Hospital, Bahir Dar University, Bahir Dar, Ethiopia, Tel +251 923557454, Email [email protected]
Introduction: Ventilator-associated pneumonia refers to pneumonia that happens at least 48 hours after endotracheal intubation. It is associated with high economic costs, longer attributable lengths of stay in the hospital, and high mortality. Therefore, this study aims to determine the incidence and predictors of ventilator-associated pneumonia among adult intensive care unit admitted patients at Bahir Dar Specialized Hospitals.
Methods: A retrospective follow-up study was conducted among 312 adult intensive care unit admitted patients. A data extraction checklist was used to collect the data. The collected data were coded, cleaned, and entered into EpiData version 3.1 and exported to SPSS version 22 and STATA version 14 for analysis. Descriptive analysis was done by using tables, text and percentages. Bivariable and multivariable log binomial analyses were conducted to identify predictors of ventilator-associated pneumonia. Variables having p-value < 0.05 were considered statistically significant.
Results: The study found that 27.9% (95% CI: 23%– 33%) of patients developed ventilator-associated pneumonia and the incidence rate of VAP was 45.7 per 1000 ventilator days. Patient’s stay more than or equal to 14 days (ARR: 13, 95% CI: 9.3– 31) and 7– 13 days on MV (ARR: 7.2, 95% CI: 6.2– 11), blood transfusion (ARR: 2.8, 95% CI: 1.1– 6.9), low GCS (ARR: 2.5, 95% CI: 1.3– 5.1), use of corticosteroid (ARR: 2.1, 95% CI: 1.1– 4.1), and supine head position (ARR: 8.1, 95% CI: 1.7– 40) were identified as independent predictors of ventilator associated pneumonia.
Conclusion: Nearly one-fourth of the participants developed ventilator-associated pneumonia. Duration of ventilation, blood transfusion, corticosteroid use, supine head position, and low Glasgow coma scale were significant predictors of ventilator-associated pneumonia.
Keywords: ventilator-associated pneumonia, predictors, incidence, intensive-care unit, adult patients, Ethiopia
Introduction
Ventilator-associated pneumonia (VAP) refers to pneumonia that happens at least 48 hours after endotracheal intubation or tracheostomy with no evidence of pneumonia at the time of intubation or at the time of admission or at the time of tracheostomy.1–3 It is a major nosocomial infection among intubated intensive care unit (ICU) patients, which requires purposeful study to reduce its morbidity and mortality. Based on the onset, it is classified as early-onset and late-onset. Early-onset VAP occurs in ventilated patients within the first four days (≤4 days) of mechanical ventilation (MV), which is usually caused by antibiotic-sensitive bacteria. Late-onset VAP refers to VAP that developed in mechanically ventilated patients from the fifth day (≥5 days) of MV and it is caused by multidrug-resistant (MDR) pathogens.4 Good knowledge of VAP incidence and its predictors is an important way to decrease its consequences and morbidity.5
According to 2016 clinical practice guidelines by the Infectious Diseases Society of America and American Thoracic Society, VAP is diagnosed when there is a new or changing lung infiltrates on chest x-ray and at least two of the following clinical feature: fever (≥38 °C), increased white blood cell count (≥12*109 WBC/mL), and purulent tracheobronchial secretions.1
Globally, the prevalence of VAP is 15.6%.6 The presence of VAP was associated with an increased risk of hospital morbidity and it remains the most frequent infection among patients hospitalized in the ICU.7
The crude mortality rate of VAP ranged from 16% to 94% compared to 0.2% to 51% in non-VAP patients, and the ICU length of stay in VAP patients ranged from 8 to 24 days compared to 2.5 to 13 days in non-VAP patients. VAP was associated with increased ICU length of stay (LOS) by 10 days and higher mortality than patients without VAP. Patients with VAP develop many complications like severe sepsis, septic shock, acute respiratory distress syndrome (ARDS), atelectasis, and infection with MDR organisms, which in turn increase cost, morbidity, and mortality.8–10
It is associated with high economic costs, longer attributable lengths of stay in the hospital, and high mortality, especially when lung infection is caused by high-risk pathogens.11–13 Studies assessing the economic impact of VAP in America found that patients with VAP had higher mean costs for hospitalization, nursing service, antibiotics, anesthesia, ventilator support, respiratory therapy, and chest x-rays, which increased the cost by 40% or higher,14 and the total cost for VAP patients was about 3-fold higher than for non-VAP patients, in which this cost was probably associated with prolonged hospitalization of VAP patients.15
Various studies in developing countries have shown that the implementation of simple, and cost-effective measures like hand washing, proper handling of respiratory tract secretions, oral hygiene with chlorhexidine, head of bed elevation greater than 30°, daily sedation break and assessment for extubation, peptic ulcer prophylaxis, deep vein thrombosis prophylaxis and the use of gloves by health workers can result in a significant reduction in the incidence of VAP.8,16–18
Therefore, this study aimed to determine the incidence and predictors of VAP to implement more effective preventive measures of VAP and thereby reduce the morbidity related to VAP.
Materials and Methods
Study Design
A retrospective follow-up study was conducted to determine the incidence and predictors of VAP.
Study Area and Study Period
This study was conducted at Tibebe Ghion Specialized Hospital (TGSH) and Felege Hiwot Comprehensive Specialized Hospital (FHCSH) among patients admitted to adult intensive care units from September to October 2021. Those hospitals are located in Bahir Dar city, 575 kilometers from Addis Ababa.
TGSH started serving people in 2018, and it is one of the teaching hospitals found in Amhara regional state, Bahir Dar; which gives a full range of clinical services of specialty and subspecialty care. This facility provides adult and pediatric ICU services with nine beds for adult ICU, six mechanical ventilators, nine patient monitors and 2 beds for pediatric ICU.
FHCSH provides health care services for more than 10 million people coming from different surrounding districts. The adult ICU is one of the 13 wards in FHCSH where critically ill patients were admitted for intubation and critical follow up having twelve beds with 6 mechanical ventilators and 12 monitors.
Source Population
All patients aged 15 and up who were on a mechanical ventilator for at least 48 hours of duration.
Study Population
All patients aged 15 and up who were on MV for at least 48 hours between April 2019 and September 2021.
Inclusion Criteria
All patients from the age of 15 years and above intubated and on mechanical ventilator for at least 48 hours.
Exclusion Criteria
Patients with pneumonia before MV or within 48 hours of MV.
Sample Size Determination
The sample-size of this study was determined by using 24.3%,19 from a study conducted at Addis Ababa university, and the target sample size was 312 patients, calculated by using a single population proportion formula:
N = (Z α/2)2 p (1-p) / d2
Where N = sample size
Z = the standard normal deviate
P = prevalence of the previous study characteristic 95% confidence interval
d = degree of precision or accuracy 5% degree of precision
α = significance level 5% Significance level
N = (1.96)2 (0.243 * 0.757) / (0.05)2`
N = 282.66 ≈ 283
N = 283 + 10% non response rate
N = 312 participants
Sample size in this study also tried to be determined by the second objective of the study using different predictor variables of VAP as shown on (Table 1).
 |
Table 1 Sample Size Determination by Using or/RR of Predictor Variables for VAP in TGSH and FHCSH, Bahir Dar, Ethiopia, 2021 |
So, 312 became the final sample size because it is largest of all.
Sampling Technique and Procedure
There were 723 intubated patients admitted to FHCSH (372), and TGSH (351), ICU departments from April 2019 to September 2021. By preparing a sampling frame using the medical registration numbers of patients for both hospitals, 312 (161 from FHCSH and 151 from TGSH) participants’ cards were drawn by a proportional allocation formula. Study participants were selected randomly by Microsoft Excel computer-generated simple random sampling technique.
Variables
Dependent Variable
Ventilator-associated pneumonia (Yes/No).
Independent Variables
There were different predictor variables like socio-demographic factors (age and sex) and admission diagnosis-related factors (low GCS, ARDS, neurosurgery, burn, cardiac diseases, diabetes mellitus, AIDS, trauma, and sepsis). In addition, intervention-related factors (duration on mechanical ventilator support, duration on intensive care unit stay, tracheostomy, reintubation, tube thoracostomy, nasogastric feeding, use of corticosteroid, supine head position, use of histamine blockers, blood transfusion, use of continuous intravenous sedatives, and prior use of broad-spectrum antibiotics) that predict the incidence of ventilator-associated pneumonia.
Operational Definitions
Ventilator-associated pneumonia: was diagnosed with the presence of a new or progressive chest x-ray infiltrate plus at least two of the following clinical symptoms: fever >38 °C with no other recognized causes, tachycardia, leukocytosis or leucopenia, new-onset purulent tracheal secretion, increased oxygen requirements in patients on a mechanical ventilator for at least of 48 hours.20
Patient use of continuous intravenous sedation: administration of continuous infusions of sedative drugs like diazepam, propofol, and ketamine.
Prior antibiotic administration: intravenous antibiotic administration for longer than 24 hours during any portion of the patient’s hospitalization before and during MV.
Low GCS: patients having less than nine GCS during admission to the ICU.
Corticosteroid use: use of corticosteroid drugs like, hydrocortisone, prednisolone, and dexamethasone for greater than 2 days during intubation.
Data Collection Tools and Procedure
Data were extracted from the patient’s registration book and select medical records of patients who had been intubated for at least 48 hours using a semi-structured data extraction checklist. Then the charts of the selected patients were reviewed in detail. The extraction checklists contained socio-demographic characteristics, patient admission diagnosis-related conditions, and ICU intervention conditions. The data were extracted by two BSc nurses and supervised by the investigator.
Data Processing and Analysis
Data were entered into EpiData version 3.1 and exported to SPSS version 22 and STATA version 14 for descriptive and log binomial regression, respectively. The descriptive outputs were presented by median, inter quartile range, and percent. Bi-variable log-binomial regression analysis was done to have an insight and select candidate predictors for multi-variable log-binomial regression analysis. The variables from bi-variable log-binomial regression with a p-value <0.25 were entered into a multivariable log-binomial regression analysis model to identify independent predictors of VAP. All p-values lower than 0.05 were considered statistically significant. The final regression model fitness was tested by the Hosmer and Lemeshow goodness of fit test and found to be good fitness with a p-value of 0.894.
Data Quality Control
One-day training was given for the data collectors on how to collect data, and the collected data was checked for its completeness and accuracy on the same day of collection. A pretest was done on five intubated ICU patient cards in FHCSH, and based on the pretest findings; there was some modification of data extraction checklists. Epi data was used for data entry to prevent data entry errors.
Ethical Considerations
This study was approved by the Institutional Review Board of Bahir Dar University, College of Medicine and Health Sciences, and ethical clearance was obtained from the board. Ethical clearance was submitted to TGSH chief clinical director and FHCSH medical director. Then the written permission was obtained from both hospitals’ clinical directors. To ensure confidentiality of the patients’ information the names and addresses of the patients were not recorded during the data collection. No one other than the investigator had access to the collected data. The investigator used the collected data only to answer the stated objectives. This study was conducted in accordance with the Declaration of Helsinki.
Result
Incidence of Ventilator-Associated Pneumonia (VAP)
From 312 study participants 87 (27.9%, 95% CI: 23%–33%) patients developed VAP during their intensive care unit stay and the incidence rate of VAP was 45.7 per 1000 ventilator days. The total ventilator days were found to be 1901 days; the median ventilator-days were 5 days with a minimum of 2 days and a maximum of 40 days. Based on onset, 13 (14.9%) patients had early onset VAP and the remaining 74 (85.1%) had late onset VAP.
Predictors of Ventilator-Associated Pneumonia
Socio-Demographic Characteristics
In this study a total of 312 patients were enrolled out of which 183 (58.7%) were male and 129 (41.3%) were female. The median age of patients was 35 years (inter-quartile range of 25–54 years).
Intervention Related Factors
The median lengths of patients on the mechanical ventilators were 6 days with an inter-quartile range of 3–10 days. The median lengths of stay of patients in the intensive care unit were 7 days and inter-quartile range of 4–14 days. Around three fourths (76%) of the participants had naso-gastric tube feeding while only 49 (16.2%) patients had reintubation (Table 2).
 |
Table 2 Intervention-Related Factors of VAP Among Patients Admitted to Adult Intensive Care Units of Felege Hiwot and Tibebe Ghion Hospitals, Bahir Dar, Ethiopia, 2021 |
Admission Diagnosis-Related Factors
From the total participants, 119 (38.5%) had low GCS, from these 47 (39.5%) developed VAP, and only 4 (1.3%) of the participants had burns, as shown in Table 3.
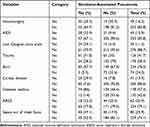 |
Table 3 Admission Diagnostic-Related Factors of VAP Among Patients Admitted to Adult Intensive Care Unit of Felege Hiwot and Tibebe Ghion Hospitals, Bahir Dar, Ethiopia, 2021 |
Bi-Variable and Multi-Variable Log Binomial Regression Analysis
The bi-variable log-binomial regression analysis identified 11 candidate predictors for the multivariable log-binomial regression model. To be liberal a p-value of 0.25 as a cut off value was used to enter in to multivariable log binomial regression. Finally, five variables including duration of patients on MV in days, steroid use, supine position, blood transfusion, and low GCS of patients were identified as predictors of VAP. Patients on MV support for more than or equal to 14 days have a 13-fold (ARR: 13, 95% CI: 9.3–31) increased risk of developing VAP, while patients on MV for 7–13 days have a 7-fold (ARR: 7.2, 95% CI: 6.2–11) increased risk of VAP than patients stay less than 7 days on MV. The patients who used corticosteroid drugs had 2.1 (ARR: 2.1, 95% CI: 1.1 – 4.1) times higher risk of developing VAP than who were not used corticosteroids. The risk of developing VAP was 8.1(ARR: 8.1, 95 % CI: 1.7 - 40) times higher among patients on supine position than semi recumbent position. Patients who were transfused blood were 2.78 (ARR: 2.8, 95 % CI: 1.1 - 6.9) times higher risk for VAP than who were not transfused. Patients with low GCS were 2.5(ARR: 2.5, 95% CI: 1.3 - 5.1) times at risk for VAP than patients who had higher GCS(Table 4).
 |
Table 4 Bi-Variable and Multivariable Analysis of Predictors of VAP Among Patients Admitted at FHCSH and TGSH Adult Intensive Care Units, Bahir Dar, Ethiopia, 2021 |
Discussion
The aim of this study is to determine the incidence and identify determinants of VAP among adult intensive care unit admitted patients at Tibebe Ghion and Felege Hiwot Specialized Hospitals. Despite MV being an essential feature of modern intensive care unit service, it is associated with a substantial risk of VAP. In this study, 27.9% (95% CI: 23%–33%) of intubated patients developed VAP. Duration ventilation, blood transfusion, corticosteroid use, supine head position, and low GCS were identified as significant predictors of VAP.
This study found that the cumulative incidence of VAP was 27.9% (95% CI: 23%−33%) and the incidence rate was 45.7 per 1000 ventilator days, It agrees with studies from Istanbul 28%,7 and in India 27.71%,21 but is lower than a study conducted in Egypt, 57.5%.22 This may be due to sociodemographic variation, and small sample size in the Egyptian study. In studies conducted in Canada and India, the incidence of VAP was 17.5%23 and 18%24 respectively, which were lower than this study's findings. This difference may be due to differences in geographical location of health facilities, VAP diagnosis criteria, as in Pondicherry, India they used both clinical and microbiological diagnosis criteria, whereas; this study only used clinical diagnosis criteria.
Patients who received blood transfusions (ARR = 2.8) were significantly predisposed for the development of VAP and it proved to be an independent risk factor, which differs from a study conducted in Turkey (95% CI: 0.4–2.6),25 this difference may be due to a variation of study designs, in Turkey the study design was case-controlled whereas the study design in this study was a retrospective follow-up study design.
In this study, low GCS was identified as an independent risk factor for the development of VAP, which is comparable with studies done in India (95% CI: 1.21 to 4.42), Addis Ababa University (p-value <0.001) and China (p-value < 0.001),19,24,26,27 but this finding is different from studies conducted at Mahatma Gandhi Medical College and Research Institute, India (95% CI: 0.41 to 2.27).5 The difference might be due to the sample size being too small in the Indian study with a total of 76 study participants as compared with this study.
Patients who had a longer stay on mechanical ventilator support had a significantly higher risk of developing VAP, which is consistent with studies from Egypt (95% CI: 4.8–22.9), India (95% CI: 0.25–0.67), Greece (p-value 0.001), and Turkey (p-value 0.001),10,28–30 but not in studies conducted at a tertiary care hospital in India.24 The reason for the difference could be due to the use of both the clinical and microbiological diagnosis criteria in the Indian study, whereas this study only used clinical diagnostic criteria.
In this study, supine head position of patients was an independent risk factor for the development of VAP, which is similar with other findings in North Bengal Medical College, India (95% CI: 0.46–0.82),29 while it was not significantly associated with VAP in studies conducted in a tertiary care hospital in India (95% CI: 0.09 to 3.94).24
In the current study finding, corticosteroid use was significantly associated with the development of VAP. This is similar to findings of studies conducted in Al-Azhar University, Egypt (95% CI: 1.1–9.2)22 and India (p-value: 0.013)31 but it was not in studies conducted in India (95% CI: 0.41–2.78)24,26 and Turkey (95% CI: 0.75–1.60).28 The reason for these differences might be due to differences in the methods of data analysis; logistic analysis was used in Indian and Turkey studies while the log binomial method of analysis was executed in this study.
Tracheostomy was not significantly associated with VAP, which is the same as Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.5 However, it has a significant association in studies conducted at Addis Ababa University,19 a tertiary care hospital in India24 and in Greece.30
The sex of patients was not a significant factor for VAP, which is similar with studies in Turkey28 and China.27
Diabetes mellitus was not an independent factor for VAP in congruence with reports done in Turkey, India25,28,31 and China,27 on the other hand it was an independent risk factor for VAP in a Turkish study, this difference may occur due to the small sample size in Turkey.
In this study, patients with tube thoracostomy (a chest tube) were not identified as a risk factor for VAP. This finding is similar to study reports done at Addis Ababa University (p-value: 0.345),19 but it is an independent risk factor in a study conducted in Greece.30
Sepsis, out of a chest focus, is not a significant factor for VAP, which is in line with study reports in France (p-value 0.85),32 but different from a study finding done in 20 European countries (95% CI: 9.5–19.9).33
Conclusion
Nearly one fourth of study participants developed VAP. The independent risk factors identified for the development of VAP were a longer duration of patients on a MV, corticosteroid use, supine position, blood transfusion, and low GCS. Knowledge of the important risk factors predisposing to VAP may prove to be useful in implementing simple and effective preventive measures including non-invasive ventilation, precaution during emergency intubation, minimizing a patient's stay on mechanical support and in an intensive care unit, avoidance of a supine position of patients, and minimize the use of histamine blockers and corticosteroids.
Abbreviations
FHCSH, Felege Hiwot Comprehensive Specialized Hospital; ICU, intensive care unit; MV, mechanical ventilation; TGSH, Tibebe Ghion Specialized Hospital; VAP, ventilator-associated pneumonia.
Data Sharing Statement
The data set used and analyzed during the current study is available from the corresponding author on reasonable request.
Ethics Approval and Participant Consent
Before conducting the study, the proposal was presented and defended. Ethical clearance was obtained from the Institutional Review Board (IRB) of Bahir Dar University. The IRB had reviewed the study protocol and approved it. Because the data gathered is secondary (patients’ medical card), informed consent of parents/legal guardians was not required and it was waived by the ethics committee of Bahir Dar University College of Medicine and Health Science Ethical Review Board. The data were not disclosed to any person other than the principal investigator. Confidentiality of the information was maintained throughout the study.
Consent for Publication
The study does not include images or videos relating to an individual’s recorded data, but concerning other collected and used data in the study, there is no doubt on consent of publication, since it is secondary data.
Acknowledgments
First of all, we would like to thank Bahir Dar University for giving us a chance to conduct this study. Secondly, we would like to thank Felege Hiwot and Tibebe Ghion Referral Hospital staffs working in the ICU Clinic, Card room and Administration, and Amhara Public Health Institute for their assistance during the collection of data, and for providing valuable data about the patients on antiretroviral therapy. We would like to acknowledge Bahir Dar University for making this thesis public through their institutional repository system.
We would also like to give our appreciation to the data collectors and supervisors for their endeavor.
Funding
No specific funding for this work. We would like to acknowledge Bahir Dar University for making this thesis public through their institutional repository system.
Disclosure
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
1. American Thoracic S; Infectious Diseases Society of A. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
2. Bassi GL, Marti JD, Comaru T, Torres A. Ventilator associated pneumonia. Sem Respi Critical Care Med. 2014;35(4):469–481.
3. Erb CT, Orr JE, Bice T, et al. Management of adults with hospital acquired and ventilator associated pneumonia. Ann Am Thoracic Soc. 2016;13(12):2258–2260. doi:10.1513/AnnalsATS.201608-641CME
4. Mathai AS, Phillips A, Kaur P, Isaac R. Incidence and attributable costs of ventilator-associated pneumonia (VAP) in a tertiary-level intensive care unit (ICU) in northern India. J Infect Public Health. 2015;8(2):127–135. doi:10.1016/j.jiph.2014.07.005
5. Charles MP, Easow JM, Joseph NM, Ravishankar M, Kumar S, Umadevi S. Incidence and risk factors of ventilator associated pneumonia in a tertiary care hospital. Australas Med J. 2013;6(4):178–182. doi:10.4066/AMJ.2013.1627
6. Kollef MH, Chastre J, Fagon JY, et al. Global prospective epidemiologic and surveillance study of ventilator-associated pneumonia due to Pseudomonas aeruginosa. Crit Care Med. 2014;42(10):2178–2187. doi:10.1097/CCM.0000000000000510
7. Bulent M. Ertugrul Ventilator-associated pneumonia in surgical emergency intensive care unit. Saudi Med J. 2006;27(1);548.
8. A-SN AY, Ziad M, Antonio A. Ventilator-associated pneumonia in adults in developing countries: a systematic review. Int J Infect Dis. 2008;12(5):505–512. doi:10.1016/j.ijid.2008.02.010
9. Cook D. Ventilator associated pneumonia: perspectives on the burden of illness. Intensive Care Med. 2000;1;26.
10. Abdelrazik Othman A, Abdelazim S. Ventilator-associated pneumonia in adult intensive care unit prevalence and complications. Egyptian J Critical Care Med. 2017;5(2):61–63. doi:10.1016/j.ejccm.2017.06.001
11. Rotstein C. Clinical practice guidelines for hospital-acquired pneumonia and ventilator-associated pneumonia in adults. Canadian J Infectious Dis. 2008;19(1):19.
12. Bassetti M, Giacobbe DR, Pelosi P. Management of ventilator-associated pneumonia: epidemiology, diagnosis and antimicrobial therapy. Expert Rev Anti Infect Ther. 2012;10(5):25. doi:10.1586/eri.12.36
13. Agrafiotis M, Siempos II, Ntaidou TK, Falagas ME. Attributable mortality of ventilator-associated pneumonia: a meta-analysis. Int J Tuberculosis Lung Dis. 2011;15(9):1154–1163. doi:10.5588/ijtld.10.0498
14. Kollef MHH, Cindy W, Ernst FR. Economic impact of ventilator-associated pneumonia in a large matched cohort”. Infect Control Hospital Epidemiol. 2012;2:250–256. doi:10.1086/664049
15. Alp E, Kalin G, Coskun R, Sungur M, Guven M, Doganay M. Economic burden of ventilator-associated pneumonia in a developing country. J Hospital Infection. 2012;81(2):128–130. doi:10.1016/j.jhin.2012.03.006
16. Timsit J, Esaied W, Neuville M, Boadma L, Mourvillier B. Update on ventilator associated pneumonia. f1000Reasearch. 2017;6;548.
17. Bird DZA, O’Donnell C, Silva J, et al. Adherence to ventilator-associated pneumonia bundle and incidence of ventilator-associated pneumonia in the surgical intensive care unit. Arch Surg. 2010;145(5):465–470. doi:10.1001/archsurg.2010.69
18. Arabi Yaseen A, Al-Shirawi N, Memish Z, Anzueto A. Ventilator-associated pneumonia in adults in developing countries: a systematic review. Int J Infect Dis. 2008;12(5):505–512.
19. Molalign G. Assessment of Disease Burden and Risk Factors Associated with the Development of Ventilator Associated Pneumonia in and Its Outcome in at Adult Intensive Care Unit of Tikur Anbessa Specialized Hospital. Addis Ababa, Ethiopia: Addis ababa university; 2018.
20. Tuche F, Brunkhorst F, Ranieri VM, Reinhart K, Sakr Y. Diagnosis of ventilator-associated pneumonia: a systematic review of the literature. Critical Care. 2008;12(2):R56. doi:10.1186/cc6877
21. Patil HV, Patil VC. Incidence, bacteriology, and clinical outcome of ventilator-associated pneumonia at tertiary care hospital. J Nat Sci Biol Med. 2017;8(1):46–55. doi:10.4103/0976-9668.198360
22. Salama BEA, Alwakil I, Elsayed M, Elsheref S, Elsheref S. Ventilator Associated Pneumonia: incidence and Risk Factors in a University Hospital. J High Inst Public Health. 2014;44(1):8–12. doi:10.21608/jhiph.2014.20336
23. Deborah J. Incidence of and Risk Factors for Ventilator-Associated Pneumonia in Critically ill Patients. Ann Intern Med. 1998;129(6):123.
24. Joseph NMSS, Dutta TK, Badhe AS, Parija SC, Parija SC. Ventilator-associated pneumonia in a tertiary care hospital in India: incidence and risk factors. J Infect Dev Countries. 2009;3(10):771–777. doi:10.3855/jidc.396
25. Erbay RHYA, Zincir M, Serin S, Atalay H. Costs and risk factors for ventilator associated pneumonia in a Turkish university hospitals intensive care unit: a case control study. BMC Pulm Med. 2004;4(1):1–7. doi:10.1186/1471-2466-4-3
26. Masih Sanjay GS, Abhishek S, Rakesh T, Sanjeev K, Sudhir S. Incidence and risk factors associated with development of ventilator-associated pneumonia from a tertiary care center of northern India. Int J Res Med Sci. 2016;1692–1697. doi:10.18203/2320-6012.ijrms20161251
27. Ding C, Zhang Y, Yang Z, et al. Incidence, temporal trend and factors associated with ventilator-associated pneumonia in mainland China: a systematic review and meta-analysis. BMC Infect Dis. 2017;17(1):468. doi:10.1186/s12879-017-2566-7
28. Kasatasm M, Kostakoglu U, Yilmaz G. An assessment of ventilator associated pneumonias and risk factors identified in the intensive care unit. Pakistan j Med Sci. 2016;32(4):817. doi:10.12669/pjms.324.10381
29. Rit K, Saha R, Chakraborty B, Majumder U. Ventilator associated pneumonia in a tertiary care hospital in India: incidence, etiology, risk factors, role of multidrug resistant pathogens. Int J Med Public Health. 2014;4(1):51. doi:10.4103/2230-8598.127125
30. Apostolopoulou E, Bakakos P, Katostaras T, Gregorakos L. Incidence and risk factors for ventilator-associated pneumonia in 4 multidisciplinary intensive care units in Athens, Greece. Respir Care. 2003;48(7):681–688.
31. Vaya SJA. Ventilator Associated Pneumonia-Study Of Demo-Graphic Profile, Risk Factors, Pathogens And Mortality In Critical Care Unit In A Tertiary Care Center. Int J Med Sci Educ. 2019;6(4):87.
32. Gacouin A, Barbarot N, Camus C, et al. Late-onset ventilator-associated pneumonia in nontrauma intensive care unit patients. Anesth Analg. 2009;109(5):1584–1590. doi:10.1213/ANE.0b013e3181b6e9b6
33. Tejerina E, Restrepo MI, Anzueto A, et al. Internacional mechanical ventilation study group. incidence, risk factors, and outcomes of ventilator associated pneumonia. J Crit Care. 2006;21(1):56–65. doi:10.1016/j.jcrc.2005.08.005
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
