Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Incidence and Predictors of Tuberculosis among Adult Diabetic Patients, Debre Markos Referral Hospital, Northwest Ethiopia, 2018: A Retrospective Cohort Study
Authors Gedfew M , Ayana M, Abate A , Bewket B , Haile D , Edmealem A , Andualem A
Received 5 October 2019
Accepted for publication 26 February 2020
Published 23 March 2020 Volume 2020:13 Pages 869—878
DOI https://doi.org/10.2147/DMSO.S233564
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Mihretie Gedfew,1 Mulatu Ayana,1 Abebe Abate,1 Bekalu Bewket,1 Dessalegn Haile,1 Afework Edmealem,2 Atsedemariam Andualem2
1College of Health Science, Debre Markos University, Debre Markos, Ethiopia; 2College of Health Science, Wollo University, Wollo, Ethiopia
Correspondence: Mihretie Gedfew Tel +251 92 5193 4333
Email [email protected]
Background: Tuberculosis remains a serious global public health problem. It mainly affects the lungs, and occurs in every part of the world. The link between tuberculosis and diabetes mellitus is essential to inform programs and policies, yet there is a scarcity of information in our study area. Therefore, this study aimed to investigate the incidence and predictors of tuberculosis among diabetic patients at Debre Markos Referral Hospital, northwest Ethiopia.
Methods: This institutionally based retrospective cohort study was undertaken among 433 diabetic patients of Debre Markos Referral Hospital between January 2013 and December 2017. All eligible diabetic patients who met the inclusion criteria were included in the study. Data were entered using EpiData version 3.1 and analyzed using Stata version 14. The survival time of diabetic patients was estimated using Kaplan–Meier survival curves, and survival time among different categorical variables compared using the log-rank test. Both bivariate and multivariate Coxproportional-hazard regression models were fitted to identify independent predictors of tuberculosis among diabetic patients.
Results: Among the cohort of 43326 (6%) developed tuberculosis during follow-up. The overall tuberculosis-incidence rate was 2.4 per 100 with 95% CI. The total time allotted to follow up the study participants was 1,101.5 person-years. Using multivariate Cox regression analysis, history of alcohol consumption (adjusted incidence ratio 4, 95% CI 1.2– 13; P=0.02) and history of tuberculosis (12, 95% CI 3– 39; P=0.01) significantly increased the risk of tuberculosis, but normal body-mass index and above (≥ 18.5 kg/m2) was associated with a rate reduction (0.34, 95% CI 0.14; P= 0.80; 0.03) forincidence of tuberculosis.
Conclusion: In this study, we found a high rate of tuberculosis among diabetic patients. Factors significantly linked with increased risk of tuberculosis included history of alcohol consumption, history of tuberculosis, and low body-mass index. Early screening and treatment for tuberculosis is highly recommended at diabetes mellitus follow-up for patients with these risk factors.
Keywords: diabetes mellitus, incidence of tuberculosis, predictors
Background
Tuberculosis (TB) is caused by Mycobacterium tuberculosis, and mainly affects the lungs. TB remains a serious public health challenge throughout the world, most notably in low- and middle-income countries, ranking above HIV/AIDS.1 Globally, around 10.4 million people fell ill with TB and 1.7 million died from the disease in 2016. The dynamics of transmission vary geographically, with the largest number of new TB cases occurring in Asia and Africa: 45% and 25% respectively.2,3
The association of TB and diabetes mellitus (DM) is a concern for health sectors, as the coexistence of these two highly prevalent diseases has made -existing treatments very complex.4 The link between TB and DM is considered more prominent in developing countries, where TB is endemic and the burden of DM increasing. Accordingly, it is estimated that about 1.6 million deaths were directly caused by DM —which is 1.69 times more likely to develop into TB than among non-DM individuals — in 2015.5,6
Currently, the worldwide prevalence of DM is increasing more quickly than ever (11.7%), which increases TB and makes existing treatments very complex among the coinfected patients.7 The prevalence of DM and the incidence of TB in Ethiopia have been found to be 6.5% and 164 per 100,000 population, respectively.1,8 However, evidence suggests that about a third of TB patients initiate care and are referred to health-care facilities with health-extension workers.9 Even though different interventions have been made by the government, TB incidence in Ethiopia remains high. Therefore, this retrospective cohort study was conducted to identify risk factors of TB among diabetic patients at Debre Markos Referral Hospital, northwest Ethiopia.
Methods
Study Design and Setting
This institutionally based retrospective cohort study was undertaken between January 2013 to December 2017 in the chronic-care follow-up care unit of Debre Markos Referral Hospital. Debre Markos is located 300 km from Addis Ababa, the capital of Ethiopia, and 256 km from Bahir-Dar, the capital of Amhara Regional State. Debre Markos Referral Hospital is the only referral hospital found in East Gojjam Zone, and serves >3.5 million people in its catchment area. Aso, the hospital provides diabetic care services. After submission of the research proposal and getting approval from the Debre Markos university Health Science College ethical review committee (Res/Com/ser/&Post gra/Coor/Off: 781/11/10) the study was conducted.
Population
The study population for this study were all adult (≥18 years old) diabetic patients registered with Debre Markos Referral Hospital for chronic follow-up care from January 1, 2013 to December 30, 2017.
Inclusion and Exclusion Criteria
All diabetic patients who fulfilled the inclusion criteria of being registered adult diabetic patients from January 1, 2013 to December 30, 2017 in the chronic-care follow-up clinic of Debre Markos Referral Hospital were included in the study. However, we excluded diabetic patients with gestational DM, incomplete data or unavailable medical records, had been transferred in and who had had TB at the time of DM diagnosis.
Data-Collection Procedures
A 5-year institution-based retrospective follow-up study was conducted using chart review at Debre Markos Referral Hospital chronic-care follow up clinic on adult diabetic patients who had been registered from January 1, 2013 to December 30, 2017. All eligible patients were included in the study (census method) after ethical clearance had been obtained from the Institutional Review Committee of the College of Health Sciences, Debre Markos University (Res/Com/ser/&Post gra/Coor/Off: 781/11/10), and verbal informed consent was obtained from the patients. Medical record number of patients were obtained from electronic database and health management information–system registry books that had been used for the routine care of DM from January 1, 2013 to December 30, 2017. Then, by using the record numbers of the patients, their medical records were identified and their status assessed for the development of TB starting from diabetic follow-up initiation (first follow-up visit) to the end of the study using validated data-collection checklists.
Variables
The dependent variable for this study was incidence of TB among diabetic patients. Independent variables were socio-demographic factors (age, sex, and residence), personal behaviors (smoking, alcohol use, and both smoking and alcohol use), and clinical characteristics (type of DM, BMI, duration of DM, glycemic control, anti-DM medications, history of TB treatment, close contact with TB patients, and history of renal failure).
Data Analysis
Data collection–checklist tools adapted from a previous study in Ethiopia were used for data collection.10 We used EpiData Version 3.1 for data entry and Stata version 14 for data analysis. The necessary assumption of the Cox proportional-hazard regression model was checked using the Schönfeld residual test and log–log plots. Diabetic cohort characteristics of continuous data were described in terms of central tendency (mean or median), dispersion (SD or IQR) and frequency distribution for categorical data. Finally, outcomes of diabetic patients were dichotomized into censored or event categories. Kaplan–Meier survival curves were used to estimate survival time, and log-rank tests to compare survival curves. Bivariate Cox proportional-hazard regression was fitted for each explanatory variable, and those with P≤0.25 in bivariate analysis were fitted to the multivariate Cox proportional-hazard regression model. HRs with 95% CIs and P-values were used to measure the strength of association and identify statistically significant predictors. In multivariat analyses, variables with P<0.05 were considered significant predictors of TB.
Results
Sociodemographic Characteristics of Study Participants
In this retrospective cohort study, 433 diabetic patients at Debre Markos Referral Hospital from January 1, 2013 to December 30, 2017 were included. Figure 1. Nearly half 187 43.2%) the patients were aged <18 years. The median age of patients was 39 (18–79 years). In addition, about 241 (55.7%) participants were male and 270 (62.5%) rural residents.
 |
Figure 1 Kaplan–Meier curve of tuberculosis survival for diabetic patients at Debre Markos Referral Hospital from January 01, 2013 to December 30, 2017 |
Clinical and Behavioral Characteristics of Patients
This study revealed that about 33 (7.6%) patients were positive for HIV and 34 (7.9%) had a history of renal failure. The duration of DM in all patients varied from date of initiation to 5 years of follow-up. A toal of 53 (12.2%) participants had a family history of DM, and 224 (51.7%) had type 1 DM. About 197 (45.5%) patients were on oral hypoglycemic agents, and 362 (83.6%) were normal and overweight. About eight (1.9%) were smokers, 16 (3.7%) had a history of alcohol consumption, and only five (1.2%) had a history of both alcohol consumption and smoking (Table 1).
 |
Table 1 Baseline Sociodemographic, Clinical, and Behavioral Characteristics of People Living with Diabetes at Debre Markos Referral Hospital from January 1, 2013 to December 30, 2017 |
Incidence of Tuberculosis among Diabetic Patients
Patients were followed for a total of 1,101.5 person years (PYs). The mean, median, and range of follow-up were 2.5, 2, and 4.8 years with (IQR 3), respectively. During follow-up, 26 (6%) patients were new TB cases (events). The overall incidence-rate ratio of TB was found to be 2.4 per 100 PYs with 95% confidence. Among the 26 individuals reporting TB, 15 (57.7%) were male and 20 (76.9%) had pulmonary TB. Of these 20 (76.9%) with pulmonary TB, only four (20%) had a history of TB. Moreover, a relatively higher proportion of TB patients 14 (53.6%) were aged 18–35 years. In addition, incidence was higher among rural residents (16, 61.5%) and those that had 1–3 years' (14, (53.8%) follow-up. More than half 19 (73.1%) TB + DM patients had type 1 DM.
Tuberculosis-Incidence Density
In this study, 433 participants were followed for different periods over 5 years, producing 1,101.5 PYs of observation. The mean, median, and range of follow-up time were 2.5, 2, and 4.8 years (IQR=3), respectively. Within follow-up, 26 patients were found to have post-DM TB (new cases), with an overall TB incidence density of 2.4 per 100 PYs with 95% confidence (Table 2, Figures 2–4).
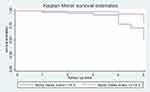 |
Figure 2 Kaplan–Meier survival curves comparing tuberculosis-free survival probability of diabetic patients based onr body-mass index. |
 |
Figure 3 Kaplan–Meier survival curves comparing tuberculosis-free survival probability of diabetic patients based on their history of tuberculosis. |
 |
Figure 4 Kaplan–Meier survival curves comparing tuberculosis-free survival probability of diabetic patients based on their history of alcohol consumption. |
Predictors of Time to TB Occurrence among Diabetic Patients
On bivariate Cox regression analysis, significant predictors (P≤0.25) of TB included HIV serostatus, history of renal failure, family history of DM, blood-glucose level, BMI, type of DM, diabetic medication, history of TB and history of alcohol consumption. To determine independent predictors of TB, a multivariate Cox proportional adjusted hazard model was fitted after the proportional hazard assumption had been checked with a global test (0.94), log-rank test for significantly associated variables on multivariate analysis (BMI 0.02, history of TB 0.001, history of alcohol consumption 0.001), and by graphic assessment. Finally, only history of alcohol consumption, history of TB, and BMI remained significant predictors of TB (P<0.05). Accordingly, those with DM who had a history of alcohol consumption had four times the risk of developing TBcompared to those who had no history of alcohol consumption (incidencerate ratio (4, 95% CI 1.2, 13); P=0.02)) and patients who had a history of TB had 12 times the risk of developing TB compared to those who had no history of TB (incidence-rate ratio 12, 95% CI 3,39; P=0.01). Conversely, patients who were normal and overweight (BMI ≥18.5 kg/m2) were less likely to develop TB (incidence-rate ratio 0.34. 95% CI 0.14–0.80; P=0.03) than their underweight (<18.5 kg/m2) counterparts.
Discussion
Despite numerous interventions to prevent TB, it remains a serious global public health concern, especially in low- and middle-income countries. Therefore, we conducted this retrospective cohort study to determine the incidence of TB among diabetic patients at Debre Markos Referral Hospital, Ethiopia. The overall incidence rate of TB at Debre Markos Referral Hospital was found to be 2.4 per 100 PYs with 95% confidencew among diabetic patients. Our figure is higher than results of a number of studies conducted in Texas (0.31 per 100PYs), China (0.30 per 100PYs, 0.22 per 100PYs), and Tanzania (1.7 per 100 PYs).11–13 These variations among studies could be explained in part by differences in sample size, study settings, follow-up periods, and sociodemographic characteristics of study participants. In addition, the distinction might be the use of sophisticated screening and diagnostic techniques for early testing and detection prior to disease progression in developed countries like the US and China. This is supported by other studies showing that sophisticated screening and diagnostic techniques for early testing and detection reduced the incidence of TB disease.7,14
Though the findings of this study are consistent with a study conducted in India (2.2 per 100 PYs),15 they are inconsistent with one in north India (0.655 per 100 PYs).16 This might be due to differences in population and study layout (a prospective study was conducted on patients with type 2 DM) in north India, which had relatively decent insulin secretion and glycemic control that prevented the development of complications and coinfections compared to type 1 DM. Conversely, our finding is much lower than the TB incidence reported in Australia (5.8 per 100 PYs) and Ethiopia (Black Lion [ 3.8 per 100PYs]17 and Dessie [6.2 per 100PYs] referral hospitals18). In the same way, these variations among studies could be explained in part by differences in sample size, study settings, follow-up periods, and sociodemographic characteristics of study participants. In this study, nearly half (48%) the respondents had type 2 DM, which is more common in advanced ages with minimal complications, including TB, because of relatively decent insulin secretion for glycemic control.11 In addition, most respondents in this study were rural residents, and so socioeconomic and demographic factors, such as problems in getting to the health-care organization, may have played a part.
In this cohort study, a history of alcohol consumption was significantly associated with TB. Accordingly, patients with a history of alcohol consumption were four times as likely to develop TB than patients with no history of TB(incidence-rate ratio 4, 95% CI 1.2–13; P=0.02). This is consistent with studies in Texas,19 Australia,20 India,21 and Ethiopia.22 However, this study contradicts findings reported from US,23 UK 24 and China.25 Variations among studies could be attributable to differences in sample size, study settings, follow-up periods, and sociodemographic characteristics of study participants.
Furthermore, one of the most significant predictors of TB among diabetic patients was a history of TB. Accordingly, patients with a history of TB were 12 times as likely to develop TB than their counter parts (incidence-rate ratio 12, (95% CI 3–39); P=0.01), which is consistent with a study conducted in Australia20 and studies in Ethiopia.17,18,22 In addition, our study demonstrated that patients with BMI ≥18.5 kg/m2 were at higher risk of TB than their counterparts (BMI <18.5 kg/m2, incidence-rate ratio 0.34, 95% CI 0.14–0.80; P=0.03), which aligns with previous studies conducted in southeastern Amhara,26 Ethiopia (systematic review),22 Egypt,27 the US,23,28 and China (adjusted HR 0.89, 95% CI 0.76–1.03).25
Conversely, this study's findings contradict those of the study conducted in Ethiopia at Black Lion hospital.10 This could be due to difference in sociodemographic characteristics as more than half the respondents in this study were rural residents and underweight. It is known that most commonly, underweight patients are considered immunocompromised to withstand TB infection. In addition, most respondents in this study were rural residents, so suchproblems as getting to the health -care organization, may have played a part.
Limitations
The main strength of this study is it was conducted using retrospective cohort design. Therefore, we were able to include a range of sociodemographic, clinical, and behavioral factors, which were very important in determining seroconversion. Despite these strengths, this study has a number of limitations. Firstly, it was conducted at a hospital; therefore, diabetic patients at home could have been missed. Moreover secondary data were used, and consequently some important variables, such as a history of cancer, chemotherapy, adherence status, glycated hemoglobin, and organ transplantation, might have been missed. Furthermore, the impact of provider training, supplies, equipment, and setup were notexplored.
Conclusion
In this 5-year diabetic cohort, the overall incidence of TB was high. Pulmonary TB accounted for the highest proportion. History of alcohol consumption and history of TB were found to be independent predictors of TB, but being normal and overweight (BMI ≥18.5 kg/m2) was found to be an independent positive factor associated with decreased risk of TB occurrence. Special attention should be given patients who have a history of alcohol consumption, history of TB, and low BMI to reduce the risk of TB incidence by improving modifiable risk factors. All diabetic patients should be screened for TB in clinical practice to prevent the occurrence of TB as early as possible. Furthermore, a prospective cohort study should be conducted to clarify relationships between predictors and TB incidence among diabetic patients.
Abbreviations
BMI, body-mass index; DM, diabetes mellitus.
Data-Sharing Statement
The data set will not be shared, in order to protect participants’ identities, but is available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from the Institutional Review Committee of the College of Health Sciences, Debre Markos University (Res/Com/ser/&Post gra/Coor/Off: 781/11/10). Oral permission was obtained from hospital administrations. Each diabetic patient received an explanation about the purpose of study, and verbal informed consent was obtained from each participant prior to proceeding. The ethical committee formally waived the need for formal written consent, since the study was done through interviewing and reviewing medical records of the couples. Therefore, the committee declared that this study was less invasive inasmuch as confidentiality was maintained. To ensure confidentiality, all collected data were coded and locked in a separate room prior to the data-entry process. Participant names were not included in the data-collection format, and data were not disclosed to any person other than the principal investigators.
Acknowledgments
We would like to acknowledge Debre Markos University for the financial funding of this research. We extend our special thanks to all data collectors and nurses working in Debre Markos Referral Hospital and supervisor.
Author Contributions
All authors contributed to data analysis, drafting, or revising the article, gave final approval of the revision to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Global, WHO. Tuberculosis Report 2017. Switzerland: Geneva; 2017.
2. WHO. Global Tuberculosis Report 2016; 2016.
3. Gilpin C, Korobitsyn A, Migliori GB, et al. The World Health Organization standards for tuberculosis care and management. Eur Respir Soc. 2018;51(3):1800098. doi:10.1183/13993003.00098-2018
4. Gyawali B, Hansen MRH, Povlsen MB, et al. Awareness, prevalence, treatment, and control of type 2 diabetes in a semi-urban area of Nepal: findings from a cross-sectional study conducted as a part of COBIN-D trial. PLoS One. 2018;13(11):e0206491. doi:10.1371/journal.pone.0206491
5. Baker MA, Harries AD, Jeon CY, et al. The impact of diabetes on tuberculosis treatment outcomes: a systematic review. BMC Med. 2011;9(1):81. doi:10.1186/1741-7015-9-81
6. Motamed N, Khonsari M, Rabiee B, et al. Discriminatory ability of Visceral Adiposity Index (VAI) in diagnosis of metabolic syndrome: a population based study. Exp Clin Endocrinol Diabetes. 2017;125(03):202–207. doi:10.1055/s-0042-119032
7. Zheng C, Hu M, Gao F. Diabetes and pulmonary tuberculosis: a global overview with special focus on the situation in Asian countries with high TB-DM burden. Glob Health Action. 2017;10(1):1264702. doi:10.1080/16549716.2016.1264702
8. Aynalem SB, Zeleke AJ. Prevalence of diabetes mellitus and its risk factors among individuals aged 15 years and above in Mizan-Aman town, Southwest Ethiopia, 2016: a cross sectional study. Int J Endocrinol. 2018;2018:1–7. doi:10.1155/2018/9317987
9. Baker M, Harries AD, Jeon CY, et al. The impact of diabetes on tuberculosis treatment outcomes: a systematic review. Туберкульоз, Легеневі Хвороби, ВІЛ-Інфекція. 2016;4:66–79.
10. Tiroro S. The magnitude and associated factors of tuberculosis among diabetic patients at Tikur Anbessa specialized teaching hospital in Addis Ababa, Ethiopia.In press 2020.
11. Restrepo BI, Camerlin AJ, Rahbar MH, et al. Cross-sectional assessment reveals high diabetes prevalence among newly-diagnosed tuberculosis cases. Bull World Health Organ. 2011;89(5):352–359. doi:10.2471/BLT.10.085738
12. Qiu H, Shi Y, Li Y, et al. Incident rate and risk factors for tuberculosis among patients with type 2 diabetes: retrospective cohort study in Shanghai, China. Trop Med Int Health. 2017;22(7):830–838. doi:10.1111/tmi.2017.22.issue-7
13. Said K, Verver S, Kalingonji A, et al. Tuberculosis among HIV-infected population: incidence and risk factors in rural Tanzania. Afr Health Sci. 2017;17(1):208–215. doi:10.4314/ahs.v17i1.26
14. Viswanathan V, Kumpatla S, Aravindalochanan V, et al. Prevalence of diabetes and pre-diabetes and associated risk factors among tuberculosis patients in India. PLoS One. 2012;7(7):e41367. doi:10.1371/journal.pone.0041367
15. Das S, Das E, Bhuyan K, et al. Bi-directional screening of tuberculosis patients for type 2 diabetes mellitus and diabetes patients for tuberculosis in Bhubaneswar, Odisha. Int J Community Med Public Health. 2017;4(7):2435–2442. doi:10.18203/2394-6040.ijcmph20172837
16. Singh SP, Singh SP, Kishan J, et al. Association of tuberculosis and diabetes Mellitus: an analysis of 1000 consecutively admitted cases in a tertiary care hospital of North India. Pan Afr Med J. 2016;24. doi:10.11604/pamj.2016.24.4.8153
17. Hamusse S, Demissie M, Teshome D, et al. Prevalence and incidence of smear-positive pulmonary tuberculosis in the Hetosa District of Arsi Zone, Oromia Regional State of Central Ethiopia. BMC Infect Dis. 2017;17(1):214. doi:10.1186/s12879-017-2321-0
18. Amare H, Gelaw A, Anagaw B, et al. Smear positive pulmonary tuberculosis among diabetic patients at the Dessie referral hospital, Northeast Ethiopia. Infect Dis Poverty. 2013;2(1):6. doi:10.1186/2049-9957-2-6
19. Restrepo B, FISHER-HOCH SP, CRESPO JG, et al. Type 2 diabetes and tuberculosis in a dynamic bi-national border population. Epidemiol Infect. 2007;135(3):483–491. doi:10.1017/S0950268806006935
20. Narasimhan P, Wood J, Macintyre CR, et al. Risk factors for tuberculosis. Pulm Med. 2013;2013:828939.
21. Rao V, Bhat J, Yadav R, et al. Smoking and alcohol consumption: risk factors for pulmonary tuberculosis among the tribal community in central India. Indian J Tuberc. 2017;64(1):40–43. doi:10.1016/j.ijtb.2016.11.009
22. Workneh MH, Bjune GA, Yimer SA, Wilkinson KA. Prevalence and associated factors of tuberculosis and diabetes mellitus comorbidity: a systematic review. PLoS One. 2017;12(4):e0175925. doi:10.1371/journal.pone.0175925
23. Goldhaber-Fiebert JD, Jeon CY, Cohen T, et al. Diabetes mellitus and tuberculosis in countries with high tuberculosis burdens: individual risks and social determinants. Int J Epidemiol. 2011;40(2):417–428. doi:10.1093/ije/dyq238
24. Pealing L, Wing K, Mathur R, et al. Risk of tuberculosis in patients with diabetes: population based cohort study using the UK clinical practice research datalink. BMC Med. 2015;13(1):135. doi:10.1186/s12916-015-0381-9
25. Zhang H, Li X, Xin H, et al. Association of body mass index with the tuberculosis infection: a population-based study among 17796 adults in rural China. Sci Rep. 2017;7(1):41933. doi:10.1038/srep41933
26. Workneh MH, Bjune GA, Yimer SA. Diabetes mellitus is associated with increased mortality during tuberculosis treatment: a prospective cohort study among tuberculosis patients in South-Eastern Amahra Region, Ethiopia. Infect Dis Poverty. 2016;5(1):22. doi:10.1186/s40249-016-0115-z
27. Khalil NH, Ramadan RA. Study of risk factors for pulmonary tuberculosis among diabetes mellitus patients. Egypt J Chest Dis Tuberc. 2016;65(4):817–823. doi:10.1016/j.ejcdt.2016.05.009
28. Benoit SR, Gregg EW, Jonnalagadda S, et al. Association of diabetes and tuberculosis disease among US-bound adult refugees, 2009–2014. Emerg Infect Dis. 2017;23(3):543. doi:10.3201/eid2303.161053
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

