Back to Journals » Open Access Emergency Medicine » Volume 14
Incidence and Predictors of Aspiration Pneumonia Among Traumatic Brain Injury in Northwest Ethiopia
Authors Shiferaw SM , Mengistie EA , Aknaw GM, Amare AT , Azanaw KA
Received 30 August 2021
Accepted for publication 10 February 2022
Published 5 March 2022 Volume 2022:14 Pages 85—98
DOI https://doi.org/10.2147/OAEM.S335927
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Sahlu Mitku Shiferaw,1 Emiru Ayalew Mengistie,2 Getasew Mulatu Aknaw,3 Abraham Tsedalu Amare,4 Kefyalew Amogne Azanaw5
1Department of Adult Health Nursing, Debre Tabor Health Science College, Debre Tabor, Ethiopia; 2Department of Adult Health, Nursing College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia; 3Department of Emergency Medicine and Critical Care, Nursing College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia; 4Department of Adult Health Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia; 5Department of Reproductive and Child Health, Debre Tabor Health Science College, Debre Tabor, Ethiopia
Correspondence: Sahlu Mitku Shiferaw, Department of Adult Health Nursing, Debre Tabor Health Science College, Po Box 83, Debre Tabor, Amhara Region, Ethiopia, Email [email protected]
Background: A significantly greater proportion of patients who die due to aspiration pneumonia were diagnosed with in-hospital aspiration pneumonia (19%). The incidence and major predictors are not known clearly, especially in Ethiopia.
Objective: To determine the incidence and predictors of aspiration pneumonia among adult traumatic brain injury patients at Felege Hiwot comprehensive specialized hospital, Bahir Dar, North west Ethiopia, in 2021.
Methods: An institution-based retrospective study was conducted from all admitted adult traumatic brain injury patients at Felege Hiwot comprehensive specialized hospital from January 1, 2015 to December 31, 2020 for 51 days of survival. Descriptive statistics, Kaplan–Meier survival curve log rank test, and the Cox proportional hazard regression model were used.
Results: A total of 396 adult patients diagnosed and admitted with traumatic brain injury in the past 5 years were included. Seventy patients (17.67%) developed aspiration pneumonia, providing an incidence rate of 32.39 (95% CI=25-62– 40.94) per 1,000 person days of observation. Independent predictors were being referred for AHR (2.43; 95% CI=1.12– 5.25), nasogastric tube insertion AHR (3.02; 95% CI=1.43– 6.39), and baseline Glasgow coma scale < 8 AHR (3.88; 95% CI=1.42– 10.062).
Conclusion: Having a nasogastric tube and low baseline Glasgow coma scale were significant predictors. This improves prehospital and hospital care during transportation and admission time.
Keywords: aspiration pneumonia, traumatic brain injury, Bahir Dar, Ethiopia
Introduction
Aspiration is often the result of impaired swallowing, which allows oral or gastric contents, or both, to enter the lung, especially in patients who also have an ineffective cough reflex;1 when there is a decreased level of consciousness, compromised airway defense mechanisms, dysphagia, gastroesophageal reflux, and recurrent vomiting.2
Decreased level of consciousness-related injury severity indicators are Glasgow Coma Scale (GCS) scores and the duration of post-traumatic amnesia; even if GCS is the usual determination (classification) method.3 Commonly, the severity of TBI has been determined according to GCS: mild (13–15 points), moderate (9–12 points), or severe (3–8 points).4,5
Aspiration pneumonia is recognized as a significant clinical problem for survivors of TBI; a significantly greater proportion of subjects who died due to AP were diagnosed with in-hospital aspiration pneumonia (19%), Patients with AP also had a significantly larger proportion of subjects with longer rehabilitation length of stay and who were discharged to nursing homes.6 Aspiration pneumonia is an infectious process because of inhalation of contaminated oropharyngeal secretions, but aspiration pneumonitis is a chemical injury from inhalation of sterile gastric contents.7 The proportion of AP cases among patients with community-acquired pneumonia was 14.2%;8 which represents 5–15% of pneumonia in the hospitalized population.9
Basic problems are possibly a lack of attention for extracranial complications, despite prevalent cause for morbidity and mortality from TBI, infrequently studied problems, unknown usual time to occurrence of aspiration pneumonia and risk factors of AP on TBI patients and its preventive mechanism, and absence of interventions necessary in the prehospital environment (in the scene area and at transportation).
Therefore this study aimed to assess the usual time to occurrence of AP among TBI patients and risk factors for development of aspiration pneumonia.
It showed the importance of prehospital interventions in prevention of these extracranial complications, and generally noticed the magnitude of the problem and importance of prevention of AP to reduce the morbidity rate of TBI patients. This study will be important for traumatic brain injury patients not to be victim of AP, since healthcare professionals can intervene on possible risk factors and it gives information on the importance of rapid health seeking behavior.
This study will be used by healthcare providers as giving some insight on the prevention of this AP by identifying timing and risk factors for its development.
Methods and Materials
Study Area and Period
This study was conducted at FCSH from admitted patients, found in Bahir Dar city (which is located at northwest Ethiopia), and 565 km from Addis Ababa; between January 1, 2015 and December 31, 2020. Bahir Dar has tourism areas like Abay river and lake Tana in the city and Tis-abay waterfall in the surrounds. FCSH serves >5,000,000 people of the region and Bahir Dar city. There are four governmental and four private hospitals in Bahir Dar city. The surgical ward is equipped with 52 nurses, 11 general practitioners, six surgeons, one neurosurgeon, and 100 beds; whereas in the ICU there are 28 nurses, two general practitioners, and 12 beds (three for the surgical side) (FCSH human resource).
Study Design
An institution-based retrospective study was conducted at FCSH on adult TBI patients admitted at the adult ICU and surgical ward.
Source and Study Population
Source population: All adult TBI patients who were admitted at FCSH due to the diagnosis of TBI.
Study Population: All adult TBI patients from January 1, 2015 to December 31, 2020 at FCSH.
Study Unit: Selected patients by computer generated simple random sampling technique.
Eligibility Criteria
Inclusion Criteria
All TBI patients aged ≥1510,11 admitted to the FCSH ICU and surgical ward because of TBI from January 1, 2015 to December 31, 2020.
Exclusion Criteria
Adult TBI patients who had a written diagnosis of AP before admission were excluded.
Study Variables
Dependent Variable
Incidence of aspiration pneumonia in FCSH.
Independent Variables
Socio-demographic factors were sex, residence, and age.
Institutional factors were ICU admission, source of referral, and length of stay at the referring institution.
Clinical factors were GCS level, baseline vital signs, type of head injury, severity of head injury, swallowing difficulty, multiple traumas, co-morbidity, and hemiplegia/hemiparesis.
Intervention related factors were prophylactic antibiotics for aspiration pneumonia, mechanical ventilation, NGT insertion, sedation, medications, and positioning.
Operational Definition
Aspiration pneumonia was defined as a written diagnosis of aspiration pneumonia, but not aspiration pneumonitis, on the patient card after admission because of TBI.
The Glasgow coma scale is a scale used for assessing the neurological status of the patient and to classify head injury as mild TBI,13–15 moderate TBI,9–12 or severe TBI (less than or equal to 8).5
”Censored” was defined as those TBI patients who did not develop the outcome of interest (AP) at the end of the follow-up period, which might be because they were lost to follow-up or transferred to a different institution, against medical advice, or death before AP at admission.
”Event” was the occurrence of AP among TBI patients from admission to the end of the study at FCSH.
Time to event was defined as the time between admission and occurrence of AP.
Median survival time was defined as the time at which half the patients had suffered AP.
The index date was the starting date for the calculation of survival and this was the first date of admission (January 1, 2015). The closing date was the last date at which the status of the patient on the follow-up (AP or censored) was determined (December 31, 2020).
Sample Size Determination
The total sample size was determined via the double population proportion formula using epi-info version 7.2.0.1 software by assuming a one-to-one ratio of exposed to non-exposed, 95% level of confidence, and a power of 80%. Two studies were used to define thevariables that are significantly associated with development of AP and importantly linked with this study. Those were NGT, hemiplegia/hemiparesis, GCS, intubation, and ventilation.12,13
The total sample size was determined using comparable literature conducted in Korea on analysis of aspiration risk factors in severe trauma patients, based on findings of aspiration lung disease in a chest CT. GCS decrement associated significantly with the occurrence of AP. Mild TBI was used as the exposure group and moderate TBI was used as the non-exposure (control group). Thus, provided a relatively large sample size (ie, 374), incomplete patient’s charts and medical records that were not found during data collection were considered; a 10% contingency was considered for each group and 37 TBI patient’s charts were added to the initial sample. So the final sample size was 411 TBI patient charts12 (Table 1).
 |
Table 1 Sample Size Determination Calculated by the Proportion of Variables from Previous Studies |
Sampling Technique and Procedure
The patient charts were selected by using a computer generated random sampling technique from the registration book of the adult ICU and surgical ward in FCSH.
This was carried out by using the registration book of the past 5 years in the adult ICU and surgical ward, and selected by using the medical registration numbers of these patients, then having cards through these medical record numbers at the card room.
Data Collection Tool and Procedure
Data Collection Tool and Period
The data were collected by using a semi-structured data extraction checklist from March 16, 2021 to April 16, 2021.
The data extraction checklist had socio-demographic data-related questions, clinical variables, preinjury health-related variables, and intervention related questions which were collected for all subjects in the sample from medical records.
Data Collection Procedure
The data was collected from selected cards by a semi-structured data extraction checklist. Before cascading data collection, two BSc. nurses were recruited for data collection and one MSc. nurse for supervision.
Two days of training was provided for the data collectors and supervisor regarding the meaning of every item of the questionnaire and the techniques of data collection.
Data Quality Control
Before the actual data collection a pre-test was conducted on 5%21 of the sample size in FCSH, 2 weeks before the actual data collection. The pre-test was analyzed and interpreted and finally modifications were made to the data extraction tool (variables were adjusted by their access).
Quality of data was assured by training data collectors and supervisors, monitoring the data collection process, and checking the completeness of data during the collection time.
Data Processing and Analysis Procedure
The collected data were verified, coded, entered by epi-data version 3.1, and exported to STATA version 14.2. The Kaplan-Meier survival curve was used to estimate the median survival time. Log rank test was used to compare survival curves between categorical variables. Cox-proportional hazard regression model was used to see the association of each independent variable with the dependent variable and pairwise correlation tests were used to check for the presence of multicollinearity between each independent variable. Bivariable Cox regression analysis was used to assess the degree of relationship within each predictor variable and TBI-related AP.
Variables that had a P-value <0.2514 with TBI-related aspiration pneumonia in the Bi-variable Cox proportional hazards regression model and had no multicollinearity were entered into the multivariable Cox-proportional hazards regression analysis model. The measure of necessary assumptions of the Cox proportional hazard model was checked using the Schoenfeld residuals test. The Cox Snell residuals test was used to assess overall model fitness.
A P-value of less than 0.05 at 95% confidence interval was taken as a cut-off point to declare a statistically significant association between predictors and post-raumatic AP.
The results of the study are presented using text, tables and figures.
Results
Socio-Demographic Characteristics of the Study Participants
There were 1,450 TBI patients listed in the registration book of the ICU (378) and surgical ward (1072) between January 1, 2015 and December 31, 2020 in FHCSH. Four hundred and eleven patient charts were selected by a computer generated simple random sampling technique, and 396 were eligible, with 15 patient charts being ineligible among the selected patient charts. From these 396 patient charts, 326 (82.32%) were censored and 70 (17.68%) had developed AP. The median age of patients at the time of admission was 29 years (IQR=22–39). Most (367; 92.68%) of the TBI and 66 (94.2%) of the post-traumatic AP were in the age group of 15–54 years. Most (288; 72.73%) came from rural areas; and 56 (80%) of the post-traumatic AP were from this group, which could show that those having a rural residency are much more affected than urban dwellers (Table 2).
 |
Table 2 Socio-Demographic Characteristics of TBI Patients at FCSH Bahir Dar, Ethiopia, from January 1, 2015 to December 31, 2020 |
Institutional Characteristics of Study Participant
Concerning their system of transfer to FCSH, 290 (73.2%) patients were referred from other health institutions; and 86% of post-traumatic AP were from such groups, which is higher than the directly admitted TBI patients. The median time for duration of presentation to FCSH was 8 hours (IQR=4–24) and their duration of presentation to FCSH revealed that most (281; 71%) patients arrived within 18 hours after injury; 80% of patients who developed AP were in this group (Table 3).
 |
Table 3 Institutional, Clinical, and Intervention Related Characteristics Study Participants |
Clinical Characteristics of Study Participants
The median baseline GCS level is 9 (IQR=6–13). Fifty-three (75.7%) patients with AP originated from GCS level within 3–8; which was measured at the time of admission to FCSH. Similarly some patients with a GCS level of >8 at baseline might deteriorate to have a level <8 which in turn results in AP (Table 3).
Intervention Related Characteristics of Study Participants
Two hundred and twelve (53.54%) TBI patients and 61 (87.1%) post-traumatic AP patients had a NGT (inserted for feeding and medication instillation purpose); which has a much higher incidence of AP than for patients without a NGT (Table 3).
Survival Status of TBI Patients to Develop AP
The overall incidence rate of AP in the cohort during the 2,161 person days of observation (PDO) was 32.39 per 1,000 (95% CI=25.62–40) person days of follow-up. Three hundred and twenty-ix (82.3%) patients were censored until the end of the study period. Among the censored patients, 223 (68.4%) were improved and discharged to home, 77 (23.61%) died, seven (2.1%) were referred to other institutions, and 19 (5.8%) left against medical advice before development of the outcome (AP) (Figure 1).
 |
Figure 1 The proportion of traumatic brain injury patient outcomes in FCSH admitted patients, Bahir Dar, Ethiopia, from January 1, 2015 to December 31, 2020. |
Overall Incidence of AP in TBI Patients
Three hundred and ninety-six TBI patients were followed for a total of 2,161 days. Kaplan Meier survival estimation showed that the cumulative survival probability after admission to FCSH was 77.68% (95% CI=72.07–82.3) at 2,161 days of follow-up. The estimated cumulative survival probability was 93.18% (95% CI=90.21–95.27) in the first 24 hours follow-up time, 87.75% (95% CI=83.97–90.69) in the next 48 hours, 83.08% (95% CI=78.70–86.64) in the next 72 hours, 78.84% (95% CI=73.74–83.05) after the first week of follow-up, and 77.68% (95% CI=72.07–82.30) on the 8th day and for the rest of the entire period.
The probability of having event free days decreases as the follow-up time increases. In this study the highest rate of AP occurred in the first week after TBI-related admission.
Incidence of AP Among Different Groups of TBI Patients
Equality of survival curves was tested by log rank test for the presence of any significant differences in survival time among various levels of categorical variables. This study shows some significant difference among survival functions of different categorical variables. The Kaplan-Meier analysis indicated significant evidence of differences in survival times(ie, the mean incidence rate of AP for referral patients was lower than those who were directly admitted, which is statistically significant at a P-value of 0.0114). The mean incidence rate of AP for sedation was lower than patients without sedation; which is statistically significant at a P-value <0.01; which reveals sedation shortens the time for occurrence of AP. Concerning NGT insertion, the mean incidence rate of AP for patients with a NGT was higher than without; which is statistically significant at a P-value <0.01. The mean incidence rate of AP for patients with blunt TBI is shorter than the penetrating type of TBI; which is significantly associated at 0.0026. This indicates that being a victim for blunt TBI shortens the time to occurrence of AP as compared to penetrating TBI. As baseline GCS level decreases, cumulative survival times get shorter and shorter; this is significantly associated with a P-value <0.01. (Table 4 and Figures 2–4).
 |
Table 4 Survival Time, Cumulative Survival Probability, and Log Rank Test in 51 Days of Follow-Up (Kaplan-Meier Method) of TBI Patients at FCSH |
 |
Figure 2 The Kaplan-Meier survival curves comparing incidence of AP on directly admitted versus referral patients in FCSH, Bahir Dar, Ethiopia, from January 1, 2015 to December 31, 2020. |
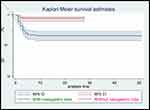 |
Figure 3 The Kaplan-Meier survival curves comparing incidence of AP on patients with nasogastric tube versus without NGT in FCSH, Bahir Dar, Ethiopia, from January 1, 2015 to December 31, 2020. |
 |
Figure 4 The Kaplan-Meier survival curves comparing incidence of AP on patients with three categories of baseline GCS level In FCSH, Bahir Dar, Ethiopia, from January 1, 2015 to December 31, 2020. |
Predictors of Aspiration Pneumonia
In the bivariable Cox proportional hazard regression model, the system of transfer to FCSH, residence, duration of presentation, mechanical ventilation use, sedation status, NGT insertion, head injury type, GCS level, and vital signs like pulse rate, respiratory rate, and temperature all fulfilled the criteria to be analyzed in multivariable Cox regression analysis; which have a P-value of <0.2514 in nivariable analysis and non-collinear independent variables (based on pairwise correlation test). In the multivariable Cox proportional hazard model, three variables were significantly associated with the development of TBI-related AP (being referred, NGT insertion, and GCS level).
The results of the multivariable Cox regression analysis revealed that the hazard of developing AP after being referred from other health institutions is 2.43-times higher as compared to those patients who were directly admitted to FCSH (AHR=.43; 95% CI=1.12–5.25).
Patients who had a nasogastric tube for feeding and medication installation purposes were 3.02-times more likely to develop TBI-related AP than patients who had no such an intervention (AHR=3.02 95% CI=1.43–6.39). The hazard of developing AP among patients who had a GCS level of less than 8 was 3.88-times more risky than a baseline GCS level >13 category (AHR=3.88; 95% CI=1.42–10.62) (Table 5).
 |
Table 5 Results of the Bivariable and Multivariable Cox Proportional Hazard Regression Analysis of TBI Patients at FCSH |
Overall Model Fitness Test
The figure below shows overall model fitness of the data in the Cox proportional hazard regression model. Residuals have a standard censored exponential distribution with hazard ratio. If we compare the jagged line with the reference line (Cox Snell residual), we observe that the hazard function follows the reference line closely, with some detachment at the end (Figure 5).
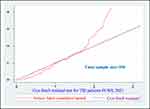 |
Figure 5 Cox Snell residual test showing overall goodness of fit for posttraumatic AP In FCSH from January 1, 2015 to December 31, 2020. |
Test of Proportional Hazard Assumption
The effects of socio-demographic, institutional, clinical, and intervention related characteristics of TBI patients for incidence of AP were examined by the Cox proportional hazards regression model. Variables included in the model as predictors were residence admission, duration of presentation, mechanical ventilation use, sedation status, nasogastric tube insertion, head injury type, respiratory rate, pulse rate, temperature, and GCS level. A goodness of fit (GOF) test was conducted to assess the proportional hazard assumptions of the Cox model for given predictor variables statistically. It reveals that almost all variables included in the model satisfied PH assumptions (P-value>0.05 except residence). The overall global test is 0.1083. So is good fit, since it is greater than 0.05 (Table 6).
 |
Table 6 Goodness of Fit Test Assesses Proportional Hazard Assumption for Incidence of Posttraumatic AP in FCSH Admitted Patients, from January 1, 2015 to December 31, 2020 |
Discussion
Aspiration pneumonia is a recognized complication following TBI. This study sought to identify the incidence and known risk factors associated with TBI induced AP while patients were in admission.
During the study period, 17.67% of the patients developed AP; which was lower than the result of a study conducted at Taiwan as “pneumonia incidence among severe TBI patients” (29.66%),12 this might be because of variation in diagnostic approaches. The cumulative probability of event free survival days for AP were 93.18%, 87.75%, 83.08%, 78.84%, and 77.68% at the 1st, 2nd, 3rd, 7th, and 8th day and for the rest of the entire period, respectively; which is shorter than the finding in the study conducted as pneumonia incidence among severe TBI patients (65%, 60%, 55%, 55%, and 55% at 10, 20, 30, 40, and 50 days, respectively).12 This discrepancy might be because of clinical service variation between these two countries.
The hazard of developing aspiration pneumonia among referral TBI patients was 2.43-times higher as compared to TBI patients who were directly admitted to FCSH. This is probably because of the distance from place of injury to hospital and rescuing speed (unlike developed countries who use helicopters for ambulance service, low income countries use own foot, by vehicle ambulance, private car and stretcher), stayed without any medical attendance by a healthcare professional, the generally long transport to hospital, and the absence of prehospital medical care exposure for such a problem.15
Those TBI patients who had a nasogastric tube for feeding and medication installation purposes were 3.02-times more likely to develop AP as compared to those TBI patients who did not have a nasogastric tube (AHR=3.04; 95% CI=1.44–6.40). This finding is in line with the findings of a study conducted in Taiwan on pneumonia incidence among severe TBI patients (AHR=4.56; 95% CI=1.11–18.64).12 Since NGT can mainly be a risk factor for aspiration pneumonia, there were misplacement during insertion, displacement of tube location in the meantime, adding additional feed from excessive residuals (ie, >150 mL), and bolus feedings for high risk patients16,17 elevated intraabdominal pressure, which are also causes for aspiration pneumonia in critically ill patients.18 NGT increases the chance of gastroesophageal reflux of gastric contents compared to patients without a NGT.19
TBI patients admitted with a baseline GCS level <8 were 3.88-times more likely to develop aspiration pneumonia than those with a GCS level >13 (AHR=3.88; 95% CI=1.42–10.62). This finding is in line with a study conducted on the analysis of aspiration risk in severe trauma patients by CT findings in Korea (ie, OR=5.073; 95% CI=2.442–10.539) since both studies showed this factor as a predictor for AP.1 As the GCS level becomes lower there should not be effective airway clearance, no adequate airway protection by the epiglottis, and there is an insufficient gag and cough reflex.1,20 These abnormalities in turn result in aspiration of oral and gastric contents, which results in aspiration pneumonia. A decreased level of consciousness associated with trauma, intoxication, or sedation from general anesthesia are risk factors for aspiration pneumonia.21,22 When there is a decreased level of consciousness, there is a greater chance of compromised airway defense mechanisms, dysphagia, gastroesophageal reflux, and recurrent vomiting.2 Dysphagia from neurological deficits can also be considered as a main cause for AP in adults.23
Conclusion
The overall incidence rate was 32.39 per 1,000 person days of follow-up, and nasogastric tube placement and low baseline Glasgow coma scale were significant predictors of incidence of aspiration pneumonia following traumatic brain injury. Prehospital airway management, adherence to standard NGT insertion and feeding procedural rules, and coma care are important management issues for prevention of post-traumatic AP.
Abbreviations
AP, aspiration pneumonia; ARDS, acute respiratory distress syndrome; CT, computed tomography; CXR, chest X-ray; FCSH, Felege Hiwot comprehensive specialized hospital; GCS, Glasgow coma scale; ICU, intensive care unit; IQR, inter-quartile range; NGT, naso-gastric tube; TBI, traumatic brain injury.
Data Sharing Statement
The data sets analyzed here are available from Sahlu Mitku Shiferaw, Emiru Ayalew Mengistie, Getasew Mulatu Aknaw, Abraham Tsedalu Amare, and Kefyalew Amogne Azanawon upon reasonable request.
Ethical Approval and Informed Consent
Ethical clearance was obtained from the institutional ethical review board of Bahir Dar University. A waiver of informed consent was approved from FCSH to review the patient’s medical records as per Helsinki declaration. Patient identification numbers and their names were removed for their confidentiality. A supporting letter was obtained from FCSH quality office. Data was only used for the purpose of this study; not for other purposes.
Acknowledgments
We would like to extend our sincere thanks to hospital staff, data collectors, and supervisors.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Amhara regional Health bureau is the external funding source for this study.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Mandell LA, Niederman MS. Aspiration pneumonia. New Engl J Med. 2019;380(7):651–663. doi:10.1056/NEJMra1714562
2. Hu X, Lee JS, Pianosi PT, Ryu JH. Aspiration-related pulmonary syndromes. Chest. 2015;147(3):815–823. doi:10.1378/chest.14-1049
3. Spitz G, Maller JJ, Ng A, O’Sullivan R, Ferris NJ, Ponsford JL. Detecting lesions after traumatic brain injury using susceptibility weighted imaging: a comparison with fluid-attenuated inversion recovery and correlation with clinical outcome. J Neurotrauma. 2013;30(24):2038–2050. doi:10.1089/neu.2013.3021
4. Silva T, Massetti T, Silva T, et al. Influence of severity of traumatic brain injury at hospital admission on clinical outcomes. Fisioter Pesqui. 2018;25(1):3–8. doi:10.1590/1809-2950/17019225012018
5. Mbakile-Mahlanza L, Manderson L, Ponsford J. The experience of traumatic brain injury in Botswana. Neuropsychol Rehabil. 2015;25(6):936–958. doi:10.1080/09602011.2014.999000
6. Howle AA, Nott MT, Baguley IJ. Aspiration pneumonia following severe traumatic brain injury: prevalence and risk factors for long-term mortality. Brain Impair. 2011;12(3):179. doi:10.1375/brim.12.3.179
7. Marik PE. Aspiration pneumonitis and aspiration pneumonia. New Engl J Med. 2001;344(9):665–671. doi:10.1056/NEJM200103013440908
8. Jeon I, Jung GP, Seo HG, Ryu JS, Han TR, Oh B-M. Proportion of aspiration pneumonia cases among patients with community-acquired pneumonia: a single-center study in Korea. Ann Rehabil Med. 2019;43(2):121. doi:10.5535/arm.2019.43.2.121
9. DiBardino DM, Wunderink RG. Aspiration pneumonia: a review of modern trends. J Crit Care. 2015;30(1):40–48. doi:10.1016/j.jcrc.2014.07.011
10. Odgaard L, Aadal L, Eskildsen M, Poulsen I. Nursing sensitive outcomes after severe traumatic brain injury: a nationwide study. J Neurosci Nurs. 2018;50(3):149–154. doi:10.1097/JNN.0000000000000365
11. Seifu W, Woldemichael K, Tsehaineh B. Prevalence and risk factors for diabetes mellitus and impaired fasting glucose among adults aged 15–64 years in Gilgel Gibe Field Research Center, Southwest Ethiopia, 2013: through a WHO step wise approach. MOJ Public Health. 2015;2(4):00035. doi:10.15406/mojph.2015.02.00035
12. Wang K-W, CHen H-J, Lu K, et al. Pneumonia in patients with severe head injury: incidence, risk factors, and outcomes. J Neurosurg. 2013;118(2):358–363. doi:10.3171/2012.10.JNS127
13. Heo GJ, Lee J, Choi WS, Hyun SY, Cho J-S. analysis of aspiration risk factors in Severe Trauma Patients: based on findings of aspiration lung disease in Chest Computed Tomography. J Trauma Inj. 2020;33(2):88–95. doi:10.20408/jti.2020.0003
14. Hosmer DW
15. Aenderl I, Gashaw T, Siebeck M, Mutschler W. Head injury-a neglected public Health problem: a four-month prospective study at Jimma University specialized hospital, Ethiopia. Ethiop J Health Sci. 2014;24(1):27–34. doi:10.4314/ejhs.v24i1.4
16. Yang F-H, Lin F-Y, Hwu Y-J. The feasibility study of a revised standard care procedure on the capacity of nasogastric tube placement verification among critical care nurses. J Nurs Res. 2019;27(4):e31. doi:10.1097/jnr.0000000000000302
17. Fan MC, Wang QL, Fang W, Jiang YX, Sun P, Wang ZH. Early enteral combined with parenteral nutrition treatment for severe traumatic brain injury: effects on immune function, nutritional status and outcomes. Chin Med Sci J. 2016;31(4):213–220. doi:10.1016/S1001-9294(17)30003-2
18. Galvagno SM, Nahmias JT, Young DA. Advanced trauma life support® Update 2019: management and applications for adults and special populations. Anesthesiol Clin. 2019;37(1):13–32. doi:10.1016/j.anclin.2018.09.009
19. Kim G, Baek S, Park HW, Kang EK, Lee G. Effect of nasogastric tube on aspiration risk: results from 147 patients with dysphagia and literature review. Dysphagia. 2018;33(6):731–738. doi:10.1007/s00455-018-9894-7
20. Hu PJ, Pittet J-F, Kerby JD, Bosarge PL, Wagener BM. Acute brain trauma, lung injury, and pneumonia: more than just altered mental status and decreased airway protection. Am J Physiol Lung Cell Mol. 2017;313(1):L1–L15. doi:10.1152/ajplung.00485.2016
21. Facts T. The American Association for the Surgery of Trauma; 2019.
22. Metheny NA. Prevention of aspiration in adults. Crit Care Nurse. 2016;36(1):e20–e24. doi:10.4037/ccn2016831
23. Goldsmith T, Kurash A. Swallowing Disorders and Aspiration in Palliative Care: Definition, Consequences, Pathophysiology, and Etiology. MA: UpToDate Inc Waltham; 2019.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
