Back to Journals » Infection and Drug Resistance » Volume 13
In vitro Activity of Ceftazidime-Avibactam and Aztreonam-Avibactam Against Carbapenem-resistant Enterobacteriaceae Isolates Collected from Three Secondary Hospitals in Southwest China Between 2018 and 2019
Authors Zou C, Wei J, Shan B, Chen X, Wang D , Niu S
Received 30 July 2020
Accepted for publication 3 September 2020
Published 12 October 2020 Volume 2020:13 Pages 3563—3568
DOI https://doi.org/10.2147/IDR.S273989
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Suresh Antony
Chunhong Zou1,2 ,* Jie Wei3 ,* Baoju Shan4,5 ,* Xian Chen,6 Deqiang Wang,2,7 Siqiang Niu1
1Department of Laboratory Medicine, The First Affiliated Hospital of Chongqing Medical University, Chongqing, People’s Republic of China; 2College of Laboratory Medicine, Chongqing Medical University, Chongqing, People’s Republic of China; 3Department of Laboratory Medicine, West China Second University Hospital, Key Laboratory of Obstetric & Gynecologic and Pediatric Diseases and Birth Defects of Ministry of Education, Sichuan University, Chengdu, People’s Republic of China; 4Pediatric Research Institute; Ministry of Education Key Laboratory of Child Development and Disorders; National Clinical Research Center for Child Health and Disorders (Chongqing), China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, People’s Republic of China; 5Chongqing Key Laboratory of Pediatrics, Children’s Hospital of Chongqing Medical University, Chongqing, People’s Republic of China; 6Department of Clinical Laboratory, The Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China; 7The Key Laboratory of Molecular Biology of Infectious Diseases Designated by the Chinese Ministry of Education, Chongqing Medical University, Chongqing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Siqiang Niu
Department of Laboratory Medicine, The First Affiliated Hospital of Chongqing Medical University, No. 1 Youyi Road, Yuzhong District, Chongqing 400016, People’s Republic of China
Tel +86-23-8901 2742
Fax +86-23-8901 2513
Email [email protected]
Purpose: To assess the antimicrobial activities of ceftazidime/avibactam (CAZ/AVI) and aztreonam/avibactam (ATM/AVI) against carbapenem-resistant Enterobacteriaceae (CRE) isolates collected from three secondary hospitals in Southwest China between 2018 and 2019.
Materials and Methods: A total of 120 unique CRE clinical isolates were collected and carbapenemase genes were detected using PCR. Antimicrobial susceptibility was determined using standard broth microdilution method and the results were interpreted according to CLSI breakpoints.
Results: The 120 carbapenem-resistant strains included 92 Klebsiella pneumoniae, 10 Escherichia coli, 10 Enterobacter cloacae, five Klebsiella aerogenes, and three Klebsiella oxytoca isolates. Seventy-four percent of these 120 CRE isolates were collected from patients located in non-ICUs; 65.0% of these CRE isolates were collected from male patients; and 34.2% of these isolates were isolated from respiratory tracts. Four different carbapenemase genes were identified among 103 carbapenemase-producing Enterobacteriaceae (CPE) isolates, including blaKPC-2 (n=77), blaNDM-1 (n=16), blaNDM-5 (n=12) and blaIMP-4 (n=2). Overall, 21.7%, 37.5%, 40.8%, 75.0%, and 100% of the CRE strains were susceptible to levofloxacin, trimethoprim/sulfamethoxazole, amikacin, CAZ/AVI, and ATM/AVI, respectively. In addition, antimicrobial susceptibility testing showed that 96.7% isolates (n=116) were resistant to aztreonam, and the addition of avibactam (4 mg/L) significantly reduced the MICs of those aztreonam-resistant isolates by more than 128-fold (range: ≤ 0.125– 4 mg/L), and 90.0% (n=108) of total 120 isolates were inhibited at ATM/AVI concentration ≤ 1 mg/L.
Conclusion: Our study revealed significant antimicrobial resistance among the CRE isolates against some commonly used antibiotics in three secondary Chinese hospitals. ATM/AVI exhibited potent activity against CRE isolates, including double carbapenemase-producing isolates, whereas CAZ/AVI was active against all KPC producers.
Keywords: carbapenem-resistant Enterobacteriaceae, carbapenemase-producing Enterobacteriaceae, ceftazidime/avibactam, aztreonam/avibactam
Introduction
Carbapenem-resistant Enterobacteriaceae (CRE) infections have become a serious clinical concern and are associated with high morbidity and mortality, as they greatly limit therapeutic options.1,2 CRE are listed as an urgent threat by the CDC of US, and have been categorized in the critical and highest priority group of pathogens by the WHO.3,4
Carbapenem resistance in Enterobacteriaceae can be caused by different mechanisms, of which the most common are the production of carbapenemases and the outer membrane porin dysfunction with extended-spectrum β-lactamases (ESBLs) and/or hyperproduction of AmpC cephalosporinase.5,6 Three major classes of carbapenemases are associated with the spread of carbapenem-resistant Enterobacteriaceae: Ambler class A (eg KPC), Ambler class B (eg, NDM, IMP and VIM), and Ambler class D (eg OXA-48-like) carbapenemases. KPC and OXA-48-like enzymes have serine-based hydrolytic activity, while metallo-β-lactamase (MBL) enzymes (encompass the Ambler class B enzymes) require the presence of metal for their activity.5,6
With the advent of new effective therapeutic options for CRE infections, such as the novel β-lactam/β-lactamase inhibitors ceftazidime/avibactam (CAZ/AVI) (active against AmpC, ESBL, KPC and OXA-48-like producers) and aztreonam/avibactam (ATM/AVI) (active against AmpC, ESBL, KPC, MBL, and OXA producers), the therapeutic recipe might be personalized based on the antimicrobial susceptibility profiles and molecular resistance phenotypes.7–10
The CAZ/AVI combination was approved by the US Food and Drug Administration in 2015 to treat complicated intra-abdominal infections, complicated urinary tract infections, hospital-acquired bacterial pneumonia, and ventilator-associated bacterial pneumonia.11,12 This combination has broad-spectrum activity against CRE isolates.13 However, this combination is not active against MBLs and KPC enzymes with substitutions (eg D179Y substitution).14,15
ATM is the only clinically used β-lactam stable to MBL hydrolysis, although it is easily inactivated by ESBLs, KPCs, and AmpC. As MBLs-carrying Enterobacteriaceae may frequently harbor additional ATM-inactivating β-lactamases, the activity of ATM against these isolates is often mitigated. However, the addition of avibactam to aztreonam make this combination active against KPC, AmpC, MBL, and OXA producers.16,17 Consequently, ATM/AVI has been proposed to treat infections due to MBL producers.
Recent study showed that the carbapenem resistance rates and CRE species containing various carbapenemases varied in different geographical regions.18 Currently, most studies on CRE were conducted in large tertiary hospitals in large cities in China, the antimicrobial resistance status in secondary or community hospitals remains rarely explored. In addition, several studies have described the in vitro activity of CAZ/AVI and ATM/AVI against clinical CRE isolates in large tertiary hospitals in China, however, their activities against CRE isolates from secondary hospitals were largely unknown. Here, we conducted a multicenter study in Southwest China to evaluate the antibacterial effect of CAZ/AVI and ATM/AVI on clinically isolated CRE bacteria collected from three secondary hospitals.
Materials and Methods
Bacterial Strains
A total of 120 nonduplicate clinical CRE isolates that were part of the routine hospital laboratory procedure causing infectious diseases were collected between 1 January 2018 and 31 December 2019 in three secondary hospitals in Chongqing, Southwest China. Species were identified using a VITEK® MS system (bioMérieux, France). In this study, CRE was defined as: resistant to any carbapenem antimicrobials (ie MICs of ≥2 μg/mL against ertapenem or ≥4 μg/mL against meropenem or imipenem.
Screening of Carbapenemase Genes
PCR was performed to screen the carbapenemase-encoding genes, including blaKPC, blaNDM, blaIMP, blaVIM and blaOXA-48-like. Positive PCR products were sequenced by Sanger sequencing (Sangon Biotech) and the sequences were blasted in GenBank (https://blast.ncbi.nlm.nih.gov/Blast.cgi). The primers used for detecting these carbapenemase genes have been reported previously.18,19
In vitro Antimicrobial Susceptibility Testing
The MICs of CRE strains were determined using standard broth microdilution method and were interpreted according to CLSI criteria.20 For CAZ/AVI and ATM/AVI testing, AVI was tested at a fixed concentration of 4 mg/L, while CAZ and ATM was added at different concentrations, respectively. Pseudomonas aeruginosa ATCC 27853 and Escherichia coli ATCC 25922 were used as quality control strains. MICs were determined in triplicate on two separate days.
Results
Bacterial Isolates and Patient Information
A total of 120 CRE isolates were collected from three secondary hospitals between 1 January 2018 and 31 December 2019 in Chongqing, Southwest China. The highest proportion of isolates was collected from Hospital A (40.8%) (Table 1). The majority of isolates were collected from patients located in non-ICUs (74.2%) and 65.0% of isolates were collected from male patients. In addition, most isolates were collected from adult patients (90.8%) (data not shown).
 |
Table 1 Species Distribution Among CRE and CPE |
The CRE isolates were mainly isolated from respiratory tracts (n=41, 34.2%), urinary tracts (n=24, 20.0%) and blood culture (n=19, 15.8%). K. pneumoniae (n=92, 76.7%), E. coli (n=10, 8.3%) and E. cloacae (n=10, 8.3%) were the most common species. K. pneumoniae and E. coli isolates were mostly from respiratory tracts, while E. cloacae isolates were more frequently isolated from urinary tracts (data not shown).
Molecular Characteristics of CRE
Among the 120 CRE isolates, 85.8% (n=103) were CPE. Among the 103 CPE isolates, 99 (96.1%) were single carbapenemase-producers while four (3.9%) carried two carbapenemase genes. Notably, three K. pneumoniae strains were found to co-carry two carbapenemase genes (two with blaKPC-2 and blaNDM-1, and one with blaNDM-1 and blaIMP-4), whilst one E. cloacae isolate co-harbored the blaKPC-2 and blaNDM-1. Among the carbapenemase genes detected, blaKPC-2 (n=77, 74.8%) was the most prevalent (Table 2). However, no isolates were found to harbor blaVIM or blaOXA-48-like. There were some differences in the proportion of carbapenemase genes by hospital, and the above 4 carbapenemase genes were prevalent in Hospital A and Hospital B, while only blaKPC-2 was found in Hospital C (Table 2).
 |
Table 2 Prevalence of Carbapenamase Genotype by Hospital |
Antimicrobial Susceptibility
These 120 CRE isolates were tested against clinically used antibiotics. The results showed that these isolates had high resistance rates against most common clinically used antibiotics tested (Table 3). According to CLSI criteria,20 over 80% isolates were resistant to imipenem and meropenem, and over 60% isolates were resistant to gentamicin, ciprofloxacin, levofloxacin and sulfamethoxazole-trimethoprim, and the most active compounds were CAZ/AVI (75.0% susceptible) and ATM/AVI (100.0% susceptible). The addition of AVI significantly lowered the ceftazidime MICs (range: 0.125–4 mg/L) by more than 128-fold, rendering 100% activity of CAZ/AVI against all the KPC-producers. A total of 29 isolates were resistant to CAZ/AVI and they were all MBL-producers. Furthermore, addition of AVI significantly lowered the aztreonam MICs (range: ≤0.125–4 mg/L) by more than 128-fold against all the 120 CRE isolates tested.
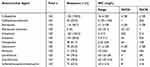 |
Table 3 In vitro Susceptibility of Different Antibiotics Against 120 CRE Isolates |
Discussion
Carbapenem-resistant Enterobacteriaceae strains have become a serious global public health threat.21 In China, the first strain harboring blaKPC was reported in 2007, and since then, blaKPC-2 has become the predominant carbapenemase gene and widely spread in China.18 Similarly, since the first description of China NDM-1-producing strain in 2010, the blaNDM gene has been recovered from various regions in China and been found in the various species of Enterobacteriaceae, including E. coli, K. pneumoniae, E. cloacae, K. oxytoca, E. aerogenes, and C. freundii.18,19,22
Avibactam is a non-β-lactam-β-lactamase inhibitor that inhibits the activities of Ambler class A -lactamases (eg, ESBLs, KPC), class C β-lactamases, and some class D β-lactamases, and avibactam restores the in vitro activity of both ceftazidime and aztreonam against KPC-producing K. pneumoniae isolates, including, in the case of ATM/AVI, activity against isolates that coproduced MBLs, and avibactam in combination with ceftazidime or aztreonam has the potential to be an agent to treat infections caused by multidrug-resistant bacteria producing the groups of β-lactamases compared with piperacillin-tazobactam and other agents.13,16,17 In addition, our results are similar to those of studies previously reported for the action of avibactam.16–18
In this observational study, we investigated the molecular mechanism of the CRE isolates collected from three secondary Southwest Chinese hospitals, and further assessed the in vitro antimicrobial activities of CAZ/AVI and ATM/AVI against these CRE isolates, while most of the other studies focused on CRE isolates from tertiary hospitals in China.18,19,22,23 Our study revealed three interesting findings.
First, the CRE isolates were detected from five different Enterobacteriaceae species. K. pneumoniae was the most common CRE species, accounting for 76.7% (92/120) of all CRE isolates. In addition, the CRE isolates were most isolated from respiratory tracts (n=41, 34.2%).
Second, diverse types of carbapenemases were identified, including KPC-2, NDM-1, NDM-5, and IMP-4. Of the 120 CRE isolates, 103 (85.8%) were found to produce carbapenemases. Among these 103 CPE strains, KPC-2 was the dominant carbapenemase (77/103, 74.8%) and was primarily found in K. pneumoniae (73/77, 94.8%). Notably, PCR failed to screen any carbapenemase genes among 17 out of 120 CRE strains, including 12 K. pneumoniae, two E. coli, two K. aerogenes and one E. cloacae, suggesting that other mechanisms may have contributed to the carbapenem resistance among these 17 isolates tested.
Third, this study demonstrated that CAZ/AVI exhibited potent activity against all the KPC producers tested in our study. Although some reports have documented cases of CAZ/AVI resistance to in KPC-2-producing K. pneumoniae isolates in China (with ESBL overexpression and OMP loss),22 our study showed that all KPC producers were highly sensitive to CAZ/AVI. Meanwhile, all the studied CRE isolates, including the MBL producers, were highly sensitive to ATM/AVI in vitro.
Taken together, our study revealed significant antimicrobial resistance of the CRE isolates against the most commonly used antibiotics in three secondary Southwest Chinese hospitals. ATM/AVI exhibited potent activity against all CRE isolates, including MBL-producing isolates, whereas CAZ/AVI was active against all KPC producers. The clinical application of these new agents should be personalized and standardized to limit misuse and avoid the emergence of resistance.
Ethical Approval
Not required.
Acknowledgments
The authors would like to thank Professor Liang Chen (Center for Discovery and Innovation, Hackensack Meridian Health, Department of Medical Sciences, Hackensack Meridian School of Medicine, Nutley, NJ, USA) for the drug avibactam and the manuscript revision.
Funding
This work was supported by the Science and Technology Research Program of Chongqing Municipal Education Commission (KJ1702022) and the Medical Research Program of Chongqing Health and Family Planning Commission in 2016 (2016MSXM001).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Righi E, Peri AM, Harris PN, et al. Global prevalence of carbapenem resistance in neutropenic patients and association with mortality and carbapenem use: systematic review and meta-analysis. J Antimicrob Chemother. 2017;72(3):668–677. doi:10.1093/jac/dkw459
2. Jee Y, Carlson J, Rafai E, et al. Antimicrobial resistance: a threat to global health. Lancet Infect Dis. 2018;18:939–940. doi:10.1016/S1473-3099(18)30471-7
3. WHO. Global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. Available from: https://www.who.int/medicines/publications/global-priority-list-antibiotic-resistant-bacteria/en/.
4. CDC. Antibiotic Resistance Threats in the United States, 2019. https://www.cdc.gov/drugresistance/biggest-threats.html. Available from:
5. Bush K. Past and present perspectives on β-lactamases. Antimicrob Agents Chemother. 2018;62:e01076–18. doi:10.1128/AAC.01076-18
6. Lee CR, Lee JH, Park KS, et al. Global dissemination of carbapenemase-producing Klebsiella pneumoniae: epidemiology, genetic context, treatment options, and detection methods. Front Microbiol. 2016;7:895. doi:10.3389/fmicb.2016.00895
7. Sader HS, Castanheira M, Shortridge D, Mendes RE, Flamm RK. Antimicrobial activity of ceftazidime–avibactam tested against multidrug-resistant Enterobacteriaceae and Pseudomonas aeruginosa isolates from U.S. medical centers, 2013 to 2016. Antimicrob Agents Chemother. 2017;61:e01045–17. doi:10.1128/AAC.01045-17
8. Sader HS, Mendes RE, Pfaller MA, Shortridge D, Flamm RK, Castanheira M. Antimicrobial activities of aztreonam-avibactam and comparator agents against contemporary (2016) clinical Enterobacteriaceae isolates. Antimicrob Agents Chemother. 2018;62:e01856–17. doi:10.1128/AAC.01856-17
9. Abboud MI, Damblon C, Brem J, et al. Interaction of avibactam with class B metallo-β-lactamases. Antimicrob Agents Chemother. 2016;60:5655–5662. doi:10.1128/AAC.00897-16
10. Bush K. Game changers: new β-lactamase inhibitor combinations targeting antibiotic resistance in Gram-negative bacteria. ACS Infect Dis. 2018;4:84–87. doi:10.1021/acsinfecdis.7b00243
11. Allergan, Inc. AVYCAZVR Package Insert. 2018. Available from: https://www.allergan.com/assets/pdf/avycaz_pi.
12. Pfizer Pharmaceuticals. Zavicefta Summary of Product Characteristics. Available from: https://www.pfizer.com/news/press-release/press-release-detail/pivotal_phase_iii_study_underscores_efficacy_of_zavicefta_ceftazidime_avibactam_for_treatment_of_hospital_acquired_pneumonia_a_leading_cause_of_mortality_in_hospitals..
13. de Jonge BL, Karlowsky JA, Kazmierczak KM, et al. In vitro susceptibility to ceftazidime-avibactam of carbapenem-nonsusceptible Enterobacteriaceae isolates collected during the INFORM global surveillance study (2012 to 2014). Antimicrob Agents Chemother. 2016;60:3163–3169. doi:10.1128/AAC.03042-15
14. Barnes MD, Winkler ML, Taracila MA, et al. Klebsiella pneumoniae carbapenemase-2 (KPC-2), substitutions at Ambler position Asp179, and resistance to ceftazidime–avibactam: unique antibiotic-resistant phenotypes emerge from β-lactamase protein engineering. mBio. 2017;8:e00528–17. doi:10.1128/mBio.00528-17
15. Castanheira M, Mendes RE, Jones RN, et al. Changes in the frequencies of β-lactamase genes among Enterobacteriaceae isolates in U.S. hospitals, 2012 to 2014: activity of ceftazidime-avibactam tested against β-lactamase-producing isolates. Antimicrob Agents Chemother. 2016;60:4770–4777. doi:10.1128/AAC.00540-16
16. Das S, Li J, Riccobene T, et al. Dose selection and validation for ceftazidime-avibactam in adults with complicated intra-abdominal infections, complicated urinary tract infections, and nosocomial pneumonia. Antimicrob Agents Chemother. 2019:63. doi:10.1128/AAC.02187-18.
17. Li H, Estabrook M, Jacoby GA, Nichols WW, Testa RT, Bush K. In vitro susceptibility of characterized beta-lactamase-producing strains tested with avibactam combinations. Antimicrob Agents Chemother. 2015;59:1789–1793. doi:10.1128/AAC.04191-14
18. Wang Q, Wang X, Wang J, et al. Phenotypic and genotypic characterization of carbapenem-resistant Enterobacteriaceae: data from a longitudinal large-scale CRE study in China (2012–2016). Clin Infect Dis. 2018;67(Suppl2):S196–205. doi:10.1093/cid/ciy660
19. Zhou T, Zhang X, Guo M, et al. Phenotypic and molecular characteristics of carbapenem-non-susceptible Enterobacteriaceae from a teaching hospital in Wenzhou, southern China. Jpn J Infect Dis. 2013;66:96–102. doi:10.7883/yoken.66.96
20. Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing.
21. Iovleva A, Doi Y. Carbapenem-Resistant Enterobacteriaceae. Clin Lab Med. 2017;37(2):303–315. doi:10.1016/j.cll.2017.01.005
22. Zou H, Xiong SJ, Lin QX, Wu ML, Niu SQ, Huang SF. CP-CRE/non-CP-CRE stratification and CRE resistance mechanism determination help in better managing cre bacteremia using CAZ/AVI and ATM/AVI. Infect Drug Resist. 2019;12:3017–3027. doi:10.2147/IDR.S219635
23. Wei J, Zou C, Wang D, Huang A, Niu S. Genetic diversity and in vitro activity of ceftazidime/avibactam and aztreonam/avibactam against imipenem-resistant Enterobacteriaceae isolates in Southwest China: a single-centre study. J Glob Antimicrob Resist. 2020;2:448–451. doi:10.1016/j.jgar.2020.04.023
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
