Back to Journals » Research and Reports in Urology » Volume 13
In Patients with Neurogenic Detrusor Overactivity and Hinman’s Syndrome: Would Intravesical Botox Injections Decrease the Incidence of Symptomatic Urinary Tract Infections
Authors Banakhar M , Yamani A
Received 24 April 2021
Accepted for publication 23 August 2021
Published 2 September 2021 Volume 2021:13 Pages 659—663
DOI https://doi.org/10.2147/RRU.S317361
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Mai Banakhar,1 Ahmed Yamani2
1Urology Department, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia; 2Urology Department, King Abdulaziz University, Jeddah, Saudi Arabia
Correspondence: Mai Banakhar
Urology Department, Faculty of Medicine, King Abdulaziz University, P.O. Box: 215089, Jeddah, Saudi Arabia
Tel +966 593435049
Fax +966 126408222
Email [email protected]
Purpose: To study the effect of intravesical Botox injection on the incidence of recurrent symptomatic UTI in neurogenic bladder patients with detrusor overactivity.
Patients and Methods: This was a prospective cohort study for patients who received Botox intravesical injection. We included patients with neurogenic bladder with detrusor overactivity and symptomatic recurrent UTI. We compared the number of symptomatic UTIs at six months pre- and post-intravesical Botox injection. Patient files were reviewed for diagnosis, vesico-uretric reflux, hydronephrosis, urodynamic findings pre- and post-injection, and dose of Botox used. Patients were followed for the number of symptomatic UTIs post-Botox injection.
Results: There were 93 patients diagnosed with neurogenic detrusor overactivity and symptomatic recurrent UTI. Patients were categorized into three categories: Group 1 – adults, Group 2 – pediatrics, Group 3 – non-neurogenic neurogenic bladder (Hinman’s syndrome). Spina bifida was diagnosed in 22 adults (Group 1) and 32 pediatric patients (Group 2). After receiving Botox injection, 75% of all patients (70) had a significant decrease in number of symptomatic UTIs. Urodynamic tests post-injection showed an improvement in bladder capacity, compliance, and detrusor pressure versus baseline in all three groups. Correlation analysis showed significant correlation between decreased symptomatic UTI post-Botox injection and detrusor pressure post-injection as well as bladder compliance; p-value=0.01 and p=0.021, respectively.
Conclusion: Intravesical Botox injection may decrease incidence of symptomatic UTI in neurogenic detrusor overactivity. This effect seemed to be related to better bladder management.
Keywords: neurogenic detrusor overactivity, intravesical Botox injections, symptomatic urinary tract infections, neurogenic bladder, recurrent UTI
Introduction
Botulinum toxin is a neurotoxin produced by the anaerobic bacteria Clostridium botulinum first isolated by Van Ermengem.1 There are several types, but type A has the best results regarding duration.1 The first usage of botulinum toxin A by Stohrer et al was in 1999, and since that time it has become a treatment for neurogenic detrusor overactivity (NDO).2,3 The FDA approved botulinum toxin A for the treatment of NDO in August 2011.
Despite the efficacy of BTX injection, the most common adverse effects post-BTX injection are urinary tract infection (UTI) and urinary retention.1,4 One randomized trial compared different doses of BTX and found the rate of post-procedural UTI to be 34–48%, with the highest being in the 200-U dose group.5
The prevalence of UTI after Botox injection is well known, but the effect of Botox injection on recurrent UTI patients is less clear. Thus, this work studies the effect of intravesical Botox injection on the incidence of recurrent symptomatic UTI in neurogenic bladder patients with detrusor overactivity.
Patients and Methods
Study Design
This was a prospective cohort study at King Abdulaziz University Hospital, Jeddah, Saudi Arabia, from April 2014 till August 2019. We received approval from the ethical board committee in agreement with the Declaration of Helsinki; we obtained patient consent from all participants, and patient anonymity was preserved. A parent or legal guardian of the pediatric patients provided informed consent.
Study Population
We recruited patients diagnosed with neurogenic overactive bladder (defined as evidence of uninhibited detrusor contraction on urodynamic test in a patient with neurological cause). This group received the maximum tolerated dose of anti-muscarinic (defined as the highest dose of treatment that does not cause unacceptable side effects) and had recurrent symptomatic UTI (defined as frequent ≥2 symptomatic UTIs in the six months before Botox therapy in a patient taking prophylactic antibiotic). This group had symptomatic UTIs (defined by any, or a combination of, fever, pain, hematuria, and/or abdominal pain and confirmed positive urine analysis and urine culture). The exclusion criteria were idiopathic overactive bladder or prostatic injections, patients with bladder stones, bladder cancer, and with indwelling catheter.
All patients received Botox injection dose 200 or 300 IU Botox (Allergan Inc., Irvine, CA, USA) via intravesical injection after treating UTI with a negative urine culture. Prophylactic antibiotics were given pre-operatively and continued orally for three post-operative days. Patients were followed after injection for six months. Visits were scheduled at 2, 6, 16, and 24 weeks post-operatively. During all visits, patients were assessed for symptoms of UTI including fever, abdominal pain, hematuria, cystitis, and pyelonephritis (orchitis in male). If any were positive from history, then urine analysis and culture were sent and marked in the patient's file as developed UTI. Patients were counseled on the frequency and setup of intermittent catheterization, and instructed to have good level of hydration during each visit.
Urodynamic tests were done in addition to the other assessments during the visit at week 16 using ICS standards. Patient files were reviewed for diagnosis, presence of reflux, hydronephrosis, urodynamic findings before and after injection, and dose of Botox used. Follow-up was up to 24 weeks (six months) because most Botox effects can wear off by six months. The number of symptomatic UTI attacks was recorded for each patient at baseline and at six months post-injection. Because of the heterogeneity of study population, the patients were categorized into three groups: Group 1 - adults, Group 2 - pediatrics, Group 3 - non-neurogenic neurogenic bladder (Hinman’s syndrome). Hinman’s is not due to pathology in the nervous system by definition, but it behaves as neurogenic bladder; thus, this population is important and was included as Group 3.
Urodynamic Test
Urodynamic tests were done at baseline for all patients before Botox injection and post-injection at week 16 using International Continence Society standards.
Measures
The primary endpoint is the number of symptomatic UTIs post-injection, which will be compared to pre-injection attacks of symptomatic UTI. All patient demographics and data were stored in Excel spreadsheets and further analyzed using IBM SPSS statistics version 26. Descriptive statistics were reported as frequencies for categorical variables. Comparisons between urodynamic variables before and after BTX injection were performed using a t-test. Correlation analysis (two-sided Pearson with two degrees of freedom) was used between incidence of UTI post-Botox injection and other patient parameters. Statistical significance was considered for p-values <0.05.
Results
A total of 93 patients were diagnosed as neurogenic detrusor overactivity and symptomatic recurrent UTI. Median patient age was 22 y (8−55 y). Group 1 had 26 adults including 22 spina bifida, two multiple sclerosis, and two spinal myelitis. Group 2 had 32 subjects all diagnosed with spina bifida. Group 3 had 35 patients.
In Group 1, 11 patients received 200 IU Botox, while 15 received 300 IU. In Group 2, 15 patients received 200 IU, while 17 received 300 IU. In Group 3, 13 received 200 IU, while 22 received 300 IU. See Table 1 for patient demographics. Group 1 had 17 patients with decreased number of recurrent UTIs. The mean number of symptomatic UTIs in Group 1 was 3±0.8, which significantly decreased post-injection to 1.1±1.1. Urodynamic parameters in Group 1 included a baseline detrusor pressure decrease from the mean of 66.2±15.3 to 32.1±15.7; bladder compliance was impaired in 11 patients and improved in only two patients. Bladder capacity improved in this group from the baseline mean of 135.3±67 mL to 273±70 mL.
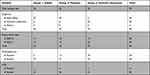 |
Table 1 Patient Demographics |
Group 2 had 25 patients with a decrease in the number of recurrent symptomatic UTIs (mean from 2±65 to 1±1). The detrusor pressure decreased from 64±17 to 30±10 post-Botox injection. Bladder compliance improved in four patients post-injection, and bladder capacity increased from 148±78 mL to 288±64 mL.
Group 3 had 26 patients with decreased number of recurrent symptomatic UTIs from 3±0.7 to 1.3±1.3. The detrusor pressure decreased from 65.3±16 to 32±15, bladder compliance improved in six patients, and bladder capacity increased from 108±66 mL to 263±64 mL (Table 2). Correlation analysis showed significant correlation between decreased number of symptomatic UTIs post-Botox injection and post-injection detrusor pressure (p=0.01) and post-injection bladder compliance (p=0.021).
 |
Table 2 Urodynamic Reading at Baseline and Post-Injection |
Discussion
Intravesical BTX is an effective treatment for neurogenic detrusor overactive patients who do not respond to conventional treatment.6,7 The detrusor paralysis is an effect of the BTX injections and decreases the incidence of incontinence due to NDO.1,8 One of the most adverse effects of BTX injections is UTI, and its incidence ranges from 21% to 58%.9 According to Mouttalib et al, the rate of symptomatic UTIs during the first week after intravesical injections of BTX was 7.1%, and the urinary bacterial colonization rate was 31% one week after BTX injection (it decreased to 26% at six weeks).11 In regard to the incidence of UTIs after BTX injections, most studies discuss the effectiveness of prophylactic antibiotics in decreasing the incidence of UTIs. A single dose of antibiotics before the procedure is usually effective for prevention of post-operative infection.12 Many other studies have discussed the importance of antibiotic prophylaxis in the neurological patient for decreasing the UTI incidence.11 Paradellaa et al confirm that the use of a single dose of antibiotics before intravesical BTX injection in patients with asymptomatic bacteriuria is enough to prevent symptomatic UTI.13 In comparison, Leitner et al investigated asymptomatic bacteriuria as a risk for UTI after BTX injections for NDO without antibiotic prophylaxis. In that study, post-injection UTI incidence was low (5–7%) and insignificant. The authors concluded that the use of prophylactic antibiotic needs to be critically reconsidered.14
To our knowledge, few studies have discussed the effect of BTX injections in NDO patients with recurrent symptomatic UTI. There seem to be discordant findings about whether intravesical BTX injection could decrease the incidence of symptomatic recurrent UTIs in patients with NDO. Game et al15 found that intravesical BTX injections decreased the incidence of symptomatic UTI significantly in patients with NDO caused by SCI or multiple sclerosis. Jia et al10 agreed with Game et al15 and found that intravesical BTX injection significantly decreased UTI in SCI patients with NDO. This was comparable to our results. Herschorn et al16 showed that the incidence of UTI was unchanged in these patients. Cruz et al21 discovered that the incidence of UTI was unchanged in SCI patients and increased in multiple sclerosis patients after intravesical BTX injections.
Our study also found that intravesical BTX injections significantly decreased UTI in patients with NDO, which shows that intravesical BTX injections might have a preventive role for UTI in those patients. It is unclear why intravesical BTX injections in NDO patients decreased the incidence of UTI. High bladder pressure is a risk factor for upper urinary tract damage and symptomatic UTI.17,18 It promotes vesicoureteral reflux and ischemic injury to the bladder walls, creating a favorable environment for infection.19,20 BTX injection improves urine incontinence and minimizes the use of urine pads. This might be a cause for the decreasing incidence of UTIs.10 In our study, urodynamic tests after injection showed an increase in bladder capacity, improved compliance, and decreased intravesical pressure in all groups. The limitations of our study are its small sample size; it cannot replace existing RCTs.
Conclusion
Intravesical Botox injection may decrease incidence of symptomatic UTI in neurogenic detrusor overactivity. This effect seemed to be related to better bladder management.
Ethics
Ethical approval No 318-20.
Author Contributions
Mai Banakhar: design, ethical approval, statistical analysis, supervision, review. Ahmed Yamani: data collection, writing. Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Duthie JB, Vincent M, Herbison GP, Wilson DI, Wilson D. Botulinum toxin injections for adults with overactive bladder syndrome. Cochrane Database Syst Rev. 2011;(12):CD005493. doi:10.1002/14651858.CD005493.pub3
2. Stohrer M, Schurch B, Kramer G, et al. Botulinum toxin A in the treatment of detrusor hyperreflexia in spinal cord injured patients: a new alternative to medical and surgical procedure? Neurourol Urodyn. 1999;18:401–402.
3. Schurch B, Schmid DM, Sto€hrer M. Treatment of neurogenic incontinence with botulinum toxin A. N Engl J Med. 2000;342:665. doi:10.1056/NEJM200003023420918
4. Kennelly M, Dmochowski R, Schulte-Baukloh H, et al. Efficacy and safety of onabotulinumtoxinA therapy are sustained over 4 years of treatment in patients with neurogenic detrusor overactivity: final results of a long-term extension study. Neurourol Urodyn. 2015;36(2):368–375.
5. Dmochowski R, Chapple C, Nitti VW, et al. Efficacy and safety of onabotulinumtoxinA for idiopathic overactive bladder: a double- blind, placebo controlled, randomized, dose ranging trial. J Urol. 2010;184(6):2416–2422. doi:10.1016/j.juro.2010.08.021
6. Lucas MG, Bosch RJL, Burkhard FC, et al. European Association of Urology guidelines on assessment and nonsurgical management of urinary incontinence. Eur Urol. 2012;62(6):1130–1142. doi:10.1016/j.eururo.2012.08.047
7. Schurch B, deSeze M, Denys P, et al. Botulinum toxin type a is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol. 2005;174:196–200. doi:10.1097/01.ju.0000162035.73977.1c
8. Kalsi V, Apostolidis A, Popat R, et al. of life changes in patients with neurogenic versus idiopathic detrusor overactivity after intradetrusor injections of botulinum neurotoxin type A and correlations with lower urinary tract symptoms and urodynamic changes. Eur Urol. 2006;49:528–535. doi:10.1016/j.eururo.2005.12.012
9. Kennelly M, Dmochowski R, Ethans K, et al. Long-term efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: an interim analysis. Urology. 2013;81(3):491–497. doi:10.1016/j.urology.2012.11.010
10. Jia C, Liao L, Chen G, et al. Detrusor botulinum toxin A injection significantly decreased urinary tract infection in patients with traumatic spinal cord injury. Spinal Cord. 2013;51(6):487–490. doi:10.1038/sc.2012.180
11. Mouttalib S, Khan S, Castel-Lacanal E, et al. Risk of urinary tract infection after detrusor botulinum toxin A injections for refractory neurogenic detrusor overactivity in patients with no antibiotic treatment. BJU Int. 2010;106:1677–1680. doi:10.1111/j.1464-410X.2010.09435.x
12. Togo Y, Kanematsu A, Kanematsu A, et al. Antimicrobial prophylaxis to prevent perioperative infection in urological surgery: a multicenter study. J Infect Chemother. 2013;19(6):1093–1101. doi:10.1007/s10156-013-0631-8
13. Paradellaa A, Musegante A, Brites C, et al. Comparison of Different Antibiotic Protocols for Asymptomatic Bacteriuria in Patients with Neurogenic Bladder Treated with Botulinum Toxin A. Braz J Infect Dis. 2016;20(6):623–626.
14. Leitner L, Sammer U, Walter M, et al. Antibiotic prophylaxis may not be necessary in patients with asymptomatic bacteriuria undergoing intradetrusor onabotulinumtoxinA injections for neurogenic detrusor overactivity. Sci Rep. 2016;6:33197. doi:10.1038/srep33197
15. Game X, Castel-Lacanal E, Bentaleb Y, et al. Botulinum toxin A detrusor injections in patients with neurogenic detrusor overactivity significantly decrease the incidence of symptomatic urinary tract infections. Eur Urol. 2008;53:613–618. doi:10.1016/j.eururo.2007.08.039
16. Herschorn S, Gajewski J, Ethans K, et al. Efficacy of botulinum toxin A injection for neurogenic detrusor overactivity and urinary incontinence: a randomized, double-blind trial. J Urol. 2011;185:2229–2235. doi:10.1016/j.juro.2011.02.004
17. D’Hondt F, Everaert K. Urinary tract infections in patients with spinal cord injuries. Curr Infect Dis Rep. 2011;13:544–551. doi:10.1007/s11908-011-0208-6
18. Sauerwein D. Urinary tract infection in patients with neurogenic bladder dysfunction. Int J Antimicrob Agents. 2002;19:592–597. doi:10.1016/S0924-8579(02)00114-0
19. Esclarin De Ruz A, Garcia Leoni E, Herruzo Cabrera R. Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J Urol. 2000;164:1285–1289. doi:10.1016/S0022-5347(05)67157-1
20. Siroky MB. Pathogenesis of bacteriuria and infection in the spinal cord injured patient. Am J Med. 2002;113(Suppl.1A):67S–79S. doi:10.1016/S0002-9343(02)01061-6
21. Cruz F, Herschorn S, Aliotta P, et al. Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial. Eur Urol. 2011;60:742–750. doi:10.1016/j.eururo.2011.07.002
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
