Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
Impulsivity, Unplanned Pregnancies, and Contraception Among Women with Bipolar Disorder
Authors Zengin Eroglu M , Lus MG
Received 16 November 2019
Accepted for publication 16 January 2020
Published 7 February 2020 Volume 2020:16 Pages 407—414
DOI https://doi.org/10.2147/NDT.S238887
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Meliha Zengin Eroglu,1 Melek Gözde Lus2
1Haydarpasa Numune Training and Research Hospital, Department of Psychiatry, Uskudar-Istanbul 34668, Turkey; 2Department of Child and Adolescent Psychiatry, Haydarpasa Numune Training and Research Hospital, Uskudar-Istanbul 34668, Turkey
Correspondence: Meliha Zengin Eroglu
Haydarpasa Numune Training and Research Hospital, Department of Psychiatry, Selimiye Mah, Tıbbiye Cad, No: 23, Uskudar-Istanbul 34668, Turkey
Tel +90 216 542 32 32
Fax +90 2163360565
Email [email protected]
Background: Impulsivity is one of the principal symptoms of bipolar and related disorders (BD). Unsafe sex and unplanned pregnancies are serious problems in clinical practice. The aim of this study was to investigate impulsivity levels, contraception methods, and levels of planned pregnancies among women with bipolar and related disorders (WBD).
Methods: Fifty-eight euthymic women with BD (bipolar disorder type I, II, or other) were matched by education levels with a control group of 59 healthy women. Data about their demographic, clinical—Barratt Impulsiveness Scale (BIS-11), Hamilton Depression Rating Scale, and Young Mania Rating Scale scores—and reproductive health features were obtained and compared between the groups.
Results: No difference was found regarding BIS-11 (total, nonplanning, motor, and attentional subscales) scores between the WBD and control groups. The overall rate of contraception use was higher in WBD (96.6%), but they generally preferred “traditional” methods (i.e., withdrawal and calendar). The total rate of unplanned pregnancies in WBD was 49.52%. Rate of unplanned pregnancies in WBD was significantly different from women without bipolar disorder (49.52% vs 15.04%).
Discussion: Levels of impulsivity in euthymic WBD under treatment were similar to those of healthy women in the control sample. WBD paid attention to contraception although they usually used traditional methods. The findings indicate that most WBD use contraception, yet the contraception is potentially ineffective especially if WBD have more unplanned pregnancies. The provision of an effective contraception method in WBD is suggested for all clinicians, in order to prevent sexually transmitted diseases and unplanned pregnancies, and thus protect the health of both mother and fetus.
Keywords: impulsivity, contraception, pregnancy, reproductive function, bipolar disorder, euthymia
Introduction
Bipolar and related disorders (BD) usually start in young adulthood and can cause serious impairment in the psychosocial, professional, and reproductive lives of patients because of its repetitive nature.1 Sometimes BD starts with a depressive episode and clinicians suppose it as a major depression until a manic or hypomanic episode occurs. Duration of untreated depression may have negative impact on clinical outcomes. Duration of untreated depression influences clinical outcomes and disability.2 Late-diagnosed patients with BD may have more disadvantages. Impulsivity is a multidimensional feature of BD, as well as of many other psychiatric disorders. It is typically associated with vulnerability, both at onset and as the disorder becomes more severe, alongside many other psychiatric comorbidities.3 Hypersexuality and increases in alcohol or substance abuse are specific symptoms that may be experienced during a manic episode. As well as in manic episodes, impulsivity also occurs in depressive and euthymic episodes. It also affects bipolar patients through personality disorders too, and many BD patients are in danger of engaging in risky behaviors.
Prior research has found that bipolar patients are more impulsive than control group patients. Moreover, in women with bipolar disorder (WBD), impulsivity is experienced differently than for men with BD. For instance, psychiatric treatment is usually interrupted by pregnancy, postpartum or when breast feeding, and these WBD become susceptible to relapses, especially during the postpartum period.4 Furthermore, untreated acute mood episodes during pregnancy is a serious risk factor for both mother and fetus.5 Therefore, these periods must be planned by clinician and patient beforehand, to ensure healthy gestation and post-partum periods.
Additionally, unsafe sex may cause sexually transmitted diseases, such as human immune deficiency virus infection (HIV), hepatitis, and herpes simplex virus, as well as abortions and interrupted pregnancies unless these reproductive WBD use some kind of effective contraception method.6–8 An increased possibility of contracting HIV and undertaking HIV risky behavior during manic episodes as well as a relationship to impulsivity have been established in earlier studies.9–11
Research on contraception use in WBD is generally very limited in the literature,7,12,13 but the prevalence of contraception use at nominal levels has been observed in recent studies.7,12 Therefore, the present study aims to analyze impulsivity, contraception use, and reproductive characteristics in euthymic WBD. In particular, we seek to answer the following research questions:
- Are euthymic WBD under treatment more impulsive than healthy women?
- What is the prevalence of contraception use and unplanned pregnancies in WBD?
- Is there any correlation between contraception use and impulsivity among WBD?
Materials and Methods
Fifty-eight, euthymic, sexually active, female outpatients with a BD diagnosis from psychiatry clinic of Haydarpaşa Numune Training and Research Hospital were consecutively recruited to participate in the study. The inclusion criteria were as follows: gender, being female; age, being between 18 and 45 years old; being sexually active; education, having at least high-school graduation; having a diagnosis of BD type I (BDI), type II (BDII), or other types according to the Diagnostic and Statistical Manual of Mental Disorders (fifth edition);14 being in an euthymic state, as defined by a Hamilton Depression Rating Scale (HAM-D) score of less than 8 points15 (the HAM-D scale was adapted to Turkish by Akdemir et al)16 or a Young Mania Rating Scale (YMRS) score of less than 817 for at least 8 weeks (the YMRS was adapted for Turkish use by Karadağ et al).18 Since self report scales will be given to patients, euthymic patients were included in the study in order to make a healthier assessment. Thus, it was aimed to minimize the risk of effect of psychotic symptoms during active phase of BPD and impulsive symptoms during manic phase of BPD on data. Patients were excluded if they had any clinical condition such as intellectual disability, Parkinson’s disease, or other serious medical problems, that could affect their ability to comprehend the instructions and complete the scales.
Fifty-nine women without a history of psychiatric diagnosis and other medical conditions impacting symptoms (intellectual disability, Parkinson’s disease, or other serious medical problems) were included in a control group. The women in this group were 18–45 years old, sexually active, and had no psychiatric disorders (based on participants’ self-report and judgement of psychiatrist). The study’s control group consisted of mothers or relatives of children admitted to the children’s and adolescents’ psychiatric outpatient clinic of the same hospital with a psychiatric complaint but who were found to be healthy following psychiatric examination. The control group was similar to the WBD group in terms of educational status.
Interviews with the WBD and the control group were performed by the same clinician. Sociodemographic data, including age, marital status, employment status, and education level, were collected through a form developed by authors for this study. All sociodemographic data recorded for comparison between groups. Clinical data about BD were also collected, including type of prophylactic treatment [type of mood stabilizer (lithium, valproic acid, carbamazepine, oxcarbazepine, or lamotrigine)], type of antipsychotic [(typical or atypical)], number of episodes, and so on. All participants were evaluated with the HAM-D and YMRS scales. Results of HAM-D and YMRS were recorded for comparison between groups.
The impulsivity of participants was evaluated using the Barratt Impulsiveness Scale-11 (BIS-11 scale), a self-report scale developed by Barratt and Patton.19 It consists of 30 items and contains three subscales, measuring attentional impulsiveness, motor impulsiveness, and nonplanning impulsiveness. Higher total score indicates higher impulsivity. Validity and reliability tests for the Turkish version of the scale were carried out.20 BIS scores of both women with BPD and controls were recorded for comparison between groups.
Sexual orientation was toward men in both WBD and controls. All participants were assessed regarding the following reproductive characteristics: menstrual irregularities, number of past pregnancies (planned or unplanned, before or after the onset of BD), lifetime number of abortions or electively interrupted pregnancies, future pregnancy plans (as discussed with a doctor), use of contraception methods, and knowledge level pertaining to contraception methods. The current contraception method (traditional or modern) used by participants was recorded, and they were asked about the types of contraception methods they knew about. Contraception methods were classified as follows: none, withdrawal method, calendar method, oral contraceptive, condom (male and female types), intrauterine contraception device (IUD), tubal ligation, vasectomy, injection, or implant. Determination of contraceptive methods as modern [oral contraceptive, condom (male and female types), intrauterine contraception device (IUD), tubal ligation, vasectomy, injection, or implant] and traditional (withdrawal method and calendar method) is made according to literature (The impact of underuse of modern methods of contraception among adolescents with unintended pregnancies in 12 low- and middle-income countries.21 Underuse of modern methods of contraception: underlying causes and consequent undesired pregnancies in 35 low- and middle-income countries.22
Ethical Considerations
The study was executed in Haydarpaşa Numune Training and Research Hospital. This study was conducted in accordance with the Declaration of Helsinki. The study was approved by Ethics Committee of Haydarpaşa Numune Training and Research Hospital and all subjects gave written informed consent. The prospective participants of each group were provided with verbal and written details regarding the study, including the objectives and details of study. Also, the choice of withdrawal from the study at any time is provided to participants.
Statistical Analysis
SPSS for Windows23 was used for the analysis. To evaluate the study data, in addition to descriptive statistical methods (mean, standard deviation, and frequency), a chi-squared test was used to compare the qualitative data. To assess relationships between clinical variables, comparative statistics in the form of Pearson’s correlation analysis was performed. Significance in the analysis was accepted at p ≤ 0.05. All statistical analyses were performed using SPSS Statistics 22.0.
Results
The control group (n=59) was similar in terms of educational status with the WBD group (n=58) (p=0.250). Distribution of educational status of WBD was high-school graduate n=41 and university graduate n=17. Distribution of educational status of controls was high-school graduate n=42 and university graduate n=17. The mean age of participants in the WBD group was 31.5±7.1 and in the control group was 36.0±5.4 years (p = 0.000). Unemployment rates were significantly higher in the WBD group (p = 0.016).
BIS scores of WBD were BIS—total: 65.53±10.28, BIS—nonplanning: 24.67±5.13, BIS—motor: 22.65±5.14 and BIS—attention: 18.39±3.63. BIS scores of controls were BIS—total: 63.11±8.89, BIS—nonplanning: 23.52±5.69, BIS—motor: 21.28±3.90 and BIS—attention: 18.63±2.95. No difference was found in BIS total and subscale (BIS—nonplanning, BIS—motor, and BIS—attention) point scores between the WBD and control groups (see Table 1).
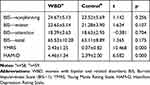 |
Table 1 Comparison of Data from the Scales |
HAM-D score of WBD is 4.46±1.34 and HAM-D score of controls is 2.39±2.00. YMRS score of WBD is 2.43±1.25 and YMRS score of controls is 0.37±0.82. Although we included participants according to cut-off points of HAM-D and YMRS scores, participants in the WBD group attained significantly higher scores than those in the control group for both scales (p = 0.000 and p = 0.000, respectively) (see Table 1).
There was no significant correlation between number of episodes and BIS—total (p = 0.422, r = 0.108), BIS—nonplanning (p = 0.966, r = −0.006), BIS—motor (p = 0.131, r = 0.201) and BIS—attention (p = 0.044, r = 0.746) scores in the WBD group.
Regarding the awareness of the groups about contraception methods, for women in the WBD group, the relative rates of knowledge about contraception methods were as follows: withdrawal, 100% (n=58); oral contraceptive pill, 89.7% (n=52); male condom, 79.3% (n=46); IUD, 58.6% (n=34); tubal ligation, 46.6% (n=27); morning-after pill, 12.1% (n=7); injectable contraception, 12.1% (n=7); calendar method, 6.9% (n=4); spermicides, 1.7% (n=1); vasectomy, 3.4% (n=2); female condom, 0% (n=0) (See Table 2).
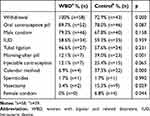 |
Table 2 Awareness of Contraception Among Groups |
In the control group, the rates of knowledge about contraception methods were as follows: oral contraceptive pill, 78.0% (n=46); withdrawal, 72.9% (n=43); male condom, 67.8% (n=40); IUD, 59.3% (n=35); tubal ligation, 57.6% (n=34); morning-after pill, 39.0% (n=23); calendar method, 37.3% (n=22); injectable contraception, 25.4% (n=15); vasectomy, 15.3% (n=9); female condom, 6.8% (n=4); spermicides, 1.7% (n=1) (See Table 2).
Rates for currently using any kind of contraceptive method were higher in the WBD than in the control group (96.6% vs 76.3%, p = 0.001). The distribution of currently used contraceptive methods is shown in Table 3. When the contraception methods are divided into two groups—“traditional methods” (withdrawal and calendar) and “modern methods” (the others)—it can be seen that participants in the WBD group (n=23) use traditional methods more than participants in the control group (n=9) (p = 0.024).
 |
Table 3 Reproductive Characteristics of WBD and Controls |
Rate of irregular menstrual cycle was higher in WBD than controls (25.9% vs 23.7%, p=0.789). The number of times participants in the WBD group had been pregnant was distributed as follows: none, 34.5% (n=20); once, 8.6% (n=5); twice, 20.7% (n=12); three times or more, 36.2% (n=21). The number of times participants in the control group had been pregnant was distributed as follows: none, 5.1% (n=3); once, 15.3% (n=9); twice, 39.0% (n=23); three times or more, 40.7% (n=24).
The number of lost or interrupted pregnancies for women in the WBD group was distributed as follows: once, 15.5% (n=9); twice or more, 22.4% (n=13). The number of lost or interrupted pregnancies for women in the control group was distributed as follows: once, 22% (n=13); twice or more, 6.8% (n=3).
Number of times been pregnant was higher in controls than WBD (2.25±1.02 vs 1.77±1.56, p=0.053). Number of total planned pregnancy was higher in controls than WBD (1.91±0.95 vs 0.89±1.03, p=0.000). Number of lost or interrupted pregnancy was similar in WBD than controls (0.65±0.94 vs 0.40±0.79, p=0.126). Number of children was higher in controls than WBD (1.88±0.91 vs 1.13±1.20, p=0.000, Cohen’s d=0.70).
The mean number of total pregnancies (planned and unplanned) after onset of BPD in the patient group was 0.77±0.79; the mean number of planned pregnancies after onset of BPD in the patient group was 0.13±0.39. The rate of total unplanned pregnancies in the WBD group was 49.52%, while, in the control group, it was 15.04%. The rate of total planned pregnancies in the WBD group was 50.48%; in the control group, it was 84.96%. The rate of subscribing a future pregnancy plan to a doctor in the WBD group was 70.7% (n=41); in the control group, it was 67.8% (n=40). Detailed information about pregnancies for both groups is presented in Table 3. No relationship was found between using any contraception method and BIS-11 scale scores (total and subscales) in either the WBD or the control groups. In WBD group using any contraception method or not; compared with using t-test for equality of means. The results were mean point of BIS—total: 66.87±6,18 vs 65.49±10.43 (p=0.854), mean point of BIS—nonplanning: 25.30±1.55 vs 24.65±5.22 (p=0.863), mean point of BIS—motor: 24.44±1.72 vs 22.58±5.21 (p=0.621) and BIS—attention: 16.80±3.39 vs 18.45±3.65 (p=0.532).
The WBD group participants were further separated out into two subgroups: those being treated with any type of mood stabilizer/stabilizers (lithium, valproic acid, carbamazepine, oxcarbazepine or lamotrigine) (n=23) and those receiving treatment comprising a mood stabilizer/stabilizers (lithium, valproic acid, carbamazepine, oxcarbazepine, or lamotrigine) and any type of antipsychotic [(typical or atypical)] (n=35). The goal of the analysis was to understand the effect of antipsychotic drugs on impulsivity in euthymic bipolar women. BIS—nonplanning scores were found to be significantly higher in the former group (mood stabilizer group mean=26.59±3.47 vs mood stabilizer + antipsychotic group mean=24.41±5.68, p = 0.020, Cohen’s d=0.46).
Discussion
Contrary to our expectations, obtained data from the study showed that impulsivity levels of participants in the WBD group were similar to those in the control group. This was probably related to the participants being under long-term treatment and in an euthymic state, along with social, cultural, and genetic factors.24 Recent studies from Turkey report higher impulsivity levels in euthymic bipolar patients. For example, BIS—motor and BIS—attention subscale scores were higher than controls.25 In another study total score and all subscales of BIS were reported higher in patients with BPD than controls.26 We did not compare our results with these study results because their study samples were mixed in gender. Also, we found no relationship between number of past episodes and impulsivity in the WBD group participants. In literature combination treatment of mood stabilizer and antipsychotic is known more effective than only mood stabilizer in bipolar disorder.27,28 Factors such as patient adherence to treatment, educational attainment levels and easy access to hospital may have affected this situation and the corresponding finding. Conversely, to our data, bipolar patients are found more impulsive than healthy people in a different study. In that study, attention (p=0.020) and motor (p=0.006) impulsivity found higher in patients with bipolar disorder.25 Also, those in the WBD group tended to be younger for their first three pregnancies than those in the control group. In parallel with this finding, it has been previously observed that lower levels of planned pregnancies feature among WBD.29
When we evaluated data from a fertility perspective, we found that the total number of pregnancies was higher in the control group. Similar pregnancy rates between WBD and control groups have been reported previously.29 In our study, although both groups consisted of women of reproductive age, the control group was marginally older, which may explain the higher number of pregnancies found in the latter group. A prior study from Turkey reported higher rates of pregnancies and children in WBD (mean of total number of pregnancies = 3.02±2.0, mean of total number of children = 2.18±1.4).30
Indeed, the overall rate of unplanned pregnancies in WBD group was found to be 49.52%; in the control group, it was 15.04%. Many studies have previously reported high rates of unplanned pregnancies in this population. For example, one third of pregnancies in WBD versus 7% of pregnancies in a control group were found to be unplanned in a prior paper.23 In a follow-up study, results pertaining to adolescents with BD were shown to feature 30% with unplanned pregnancies.31 In other research, the number of unplanned pregnancies was likewise found to be higher in the BD group (mean=1.64±2.59) than in the control group.13 When the relationship between contraception use and impulsivity in WBD was explored, we saw that no association was existed. In WBD group using any contraception method or not; compared with using t-test for equality of means. The results were mean point of BIS-total: 66.87±6.18 vs 65.49±10.43 (p=0.854), mean point of BIS—nonplanning: 25.30±1.55 vs 24.65±5.22 (p=0.863), mean point of BIS—motor: 24.44±1.72 vs 22.58±5.21 (p=0.621) and BIS—attention: 16.80 ±3,39 vs 18.45±3.65 (p=0.532).
According to our data, the number of total planned pregnancies was found to be lower in the WBD than the control group (50.48% vs 84.96%). Awareness about BD, teratogenicity, and contraception in the WBD group may have influenced these results. Also, the high rates (70.7%) of sharing future pregnancy plan with doctors in the WBD group suggests that WBD patients are more in contact with their doctors. In a similar study, rates of planned pregnancies in the BD group was 32.8%, while, in the control group, it was 78.1%;29 planned pregnancy rates in our study were found to be higher than in this earlier research. A similar study from Turkey has reported higher numbers of planned pregnancies (1.71±1.44) in the control group too.13
Marinelli et al found 55% of their WBD group reported abortions.32 At least one voluntary interruption of pregnancy rate has been reported previously: 42% in the WBD group and 14% in the control group.29 We did not asses the reasons for pregnancies being electively interrupted or for abortions, but found similar results in both of our study’s groups. In contrast to our results, though, another recent study found that the number of abortions (dilatation and curettage) was higher in the BD group than in the control group.13
Arguably, the most significant result of our study was the finding concerning the high rates of contraceptive use in WBD (96.6% vs 76.3%). Factors such as high educational levels, high levels of psychosocial functioning, easy access to medical care, living in a city center, and a high awareness of reproductive health care may explain this result. A study from Turkey has reported this rate to be between 73.7% and 85.2% in WBD.13,33 We found the most used contraception method in WBD to be withdrawal, while, in the control group, it was IUDs. Traditional contraception methods were more popular in WBD. Previous authors have found no difference between the groups in terms of the frequency of using family planning methods.13 However, similar to our results, the withdrawal method was found to be commonly used in WBD, while condom use was common among the control group.13 Contrasting results regarding the use of contraception methods among WBD are seen in the literature, ranging from no differences to suboptimal contraception use being recorded in respect of WBD compared with control groups.7,29,34
Hormonal contraception and IUDs are safe for use by WBD. That is, oral contraceptives, levonorgestrel-releasing IUDs, and depot medroxyprogesterone acetate use among WBD was not associated with a worsening of the clinical course of the disease compared with the use of non-hormonal methods.35 In addition, tube ligation and quarterly injection have been suggested as the most effective contraception methods in this context.8
Rate of irregular menstruation is 25.9% in our WBD group. Research has found the rate of irregular menstruation in bipolar women to be 15.1%, with a lifetime rate of irregular menstruation being recorded as 38.7%.13 Stress factors, adverse effects of treatment and hormonal problems may cause irregular menstruation in WBD. Menstrual abnormalities have been reported by 51.5% of WBD.30
As well as the above-discussed findings, the present study also features some limitations, including its small sample size, cross-sectional design, the inclusion only of patients from a training and research hospital, limited comparison of the groups from the treatment perspectives, self-reported and retrospective data collection (recall bias), and the lack of evaluation of episode type occurring with an unplanned pregnancy. Positive aspects of the study include its use of a control group, its descriptive design, and its exploration of both impulsivity and of contraception methods.
Conclusion
In our research, euthymic WBD were found to use contraception extensively, but they mostly favored traditional methods. They were not more impulsive than their healthy counterparts in the control group, but rates of unplanned pregnancies were still unacceptably high. This study presents substantial information about impulsivity, contraceptive methods, and other reproductive characteristics of WBD from Turkey. Contraception use is not associated with impulsivity only. Many other factors affect it. True and effective contraception method, decided by patient and clinician, must be used in WBD for better course of BD, healthy mothers, and babies. For future research, more data from longitudinal studies about contraception, chose of contraceptive methods, reproduction, side effects of medications on reproduction, pregnancy planning, and family planning in WBD should be obtained.
Acknowledgment
We would like to thank all the women who participated in our research, and also department secretary Fatma Zehra Deniz.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Özerdem A, Rasgon N. Women with bipolar disorder: a lifetime challenge from diagnosis to treatment. Bipolar Disord. 2014;16(1):1–4. doi:10.1111/bdi.2014.16.issue-1
2. Ghio L, Gotelli S, Cervetti A, et al. Duration of untreated depression influences clinical outcomes and disability. J Affect Disord. 2015;175:224–228. doi:10.1016/j.jad.2015.01.014
3. Rote J, Dingelstadt A-M-L, Aigner A, et al. Impulsivity predicts illness severity in long-term course of bipolar disorder: a prospective approach. Aust N Z J Psychiatry. 2018;52(9):876–886. doi:10.1177/0004867418783062
4. Miller LJ, Ghadiali NY, Larusso EM, et al. Bipolar disorder in women. Health Care Women Int. 2015;36(4):475–498. doi:10.1080/07399332.2014.962138
5. Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–1819. doi:10.1016/S0140-6736(14)61277-0
6. Grimes DA, Benson J, Singh S, et al. Unsafe abortion: the preventable pandemic. Lancet. 2006;368(9550):1908–1919. doi:10.1016/S0140-6736(06)69481-6
7. da Silva Magalhães PV, Kapczinski F, Kauer-Sant’Anna M. Use of contraceptive methods among women treated for bipolar disorder. Arch Womens Ment Health. 2009;12(3):183. doi:10.1007/s00737-009-0060-y
8. Berenson AB, Asem H, Tan A, Wilkinson GS. Continuation rates and complications of intrauterine contraception in women diagnosed with bipolar disorder. Obstet Gynecol. 2011;118(6):1331. doi:10.1097/AOG.0b013e318233beae
9. Meade CS, Graff FS, Griffin ML, Weiss RD. HIV risk behavior among patients with co-occurring bipolar and substance use disorders: associations with mania and drug abuse. Drug Alcohol Depend. 2008;92(1–3):296–300. doi:10.1016/j.drugalcdep.2007.07.013
10. Beyer JL, Taylor L, Gersing KR, Krishnan KRR. Prevalence of HIV infection in a general psychiatric outpatient population. Psychosomatics. 2007;48(1):31–37. doi:10.1176/appi.psy.48.1.31
11. Namlı Z, Karakuş G, Tamam L, Demirkol ME. Sexuality and sexual dysfunctions in bipolar disorder. Curr Approaches Psychiatry. 2016;8(4):309–320.
12. McCandless F, Sladen C. Sexual health and women with bipolar disorder. J Adv Nurs. 2003;44(1):42–48. doi:10.1046/j.1365-2648.2003.02766.x
13. Dinc H, Boyacioglu NE, Ozcan NK, Enginkaya S. Reproductive and sexual health in women with bipolar disorder: a comparative study. Dusunen Adam. 2019;32(1):23–32.
14. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub; 2013.
15. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56. doi:10.1136/jnnp.23.1.56
16. Akdemir A, Orsel S, Dag İ, Turkcapar H, Iscan N, Ozbay H. Validity, reliability and clinical application of Hamilton Depression Rating Scale (HDRS). J Psychiatry Psychol Psychopharmacol. 1996;4:251–259.
17. Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133(5):429–435. doi:10.1192/bjp.133.5.429
18. Karadağ F, Oral T, Yalcin FA, Erten E. Reliability and validity of Turkish translation of young mania rating scale. Turk Psikiyatri Derg. 2002;13(2):107–114.
19. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51(6):768–774. doi:10.1002/(ISSN)1097-4679
20. Güleç H, Tamam L, Turhan M, Karakuş G, Zengin M, Stanford MS. Psychometric properties of the Turkish version of the Barratt Impulsiveness Scale-11. Bull Clin Psychopharmacol. 2008;18:4.
21. Bellizzi S, Pichierri G, Menchini L, Barry J, Sotgiu G, Bassat Q. The impact of underuse of modern methods of contraception among adolescents with unintended pregnancies in 12 low-and middle-income countries. J Glob Health. 2019;9:2. doi:10.7189/jogh.09.020429
22. Bellizzi S, Sobel HL, Obara H, Temmerman M. Underuse of modern methods of contraception: underlying causes and consequent undesired pregnancies in 35 low-and middle-income countries. Human Reprod. 2015;30(4):973–986. doi:10.1093/humrep/deu348
23. IBM Corp N. IBM SPSS statistics for windows. Version 220; 2013.
24. Eroglu MZ, Ozpoyraz N, Tamam L. Prophylactic treatment in bipolar disorder. J Mood Disord. 2014;4(3):95. doi:10.5455/jmood.
25. Apaydin ZK, Atagun Mİ. Relationship of functionality with impulsivity and coping strategies in bipolar disorder. J Psychiatry Neurol Sci. 2018;31(2):21–29.
26. Gulec H, Tamam L, Usta H, et al. Impulsivity in bipolar disorder. Anadolu Psikiyatri Derg. 2009;10(3):198–203.
27. Eroglu MZ, Özpoyraz N. Long-term treatment in bipolar disorder. Curr Approaches Psychiatry. 2010;2(2):206.
28. Tohen M, Chengappa KR, Suppes T, et al. Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. Br J Psychiatry. 2004;184(4):337–345. doi:10.1192/bjp.184.4.337
29. Marengo E, Martino DJ, Igoa A, et al. Unplanned pregnancies and reproductive health among women with bipolar disorder. J Affect Disord. 2015;178:201–205. doi:10.1016/j.jad.2015.02.033
30. Annagür BB, Zincir SB, Bez Y, et al. Social and reproductive lives of women with bipolar disorder: a descriptive study from Turkey. Psychiatry Behav Sci. 2013;3(1):11.
31. Heffner JL, DelBello MP, Fleck DE, Adler CM, Strakowski SM. Unplanned pregnancies in adolescents with bipolar disorder. Am Journal Psychiatry. 2012;169(12):1319. doi:10.1176/appi.ajp.2012.12060828
32. Marinelli M, Lorenzo L, Zaratiegui R. Reproductive characteristics of female outpatients of childbearing age with affective disorders: P157. Bipolar Disord. 2012;14:102–103.
33. Aldemir E, Akdeniz F, Isikli S, Bilen NK, Vahip S. Reproductive and sexual functions in bipolar patients: data from a specialized mood disorder clinic. Dusunen Adam. 2016;29(1):67. doi:10.5350/DAJPN2016290107
34. Özcan NK, Boyacıoğlu NE, Enginkaya S, Dinç H, Bilgin H. Reproductive health in women with serious mental illnesses. J Clin Nurs. 2014;23(9–10):1283–1291. doi:10.1111/jocn.2014.23.issue-9pt10
35. Pagano HP, Zapata LB, Berry-Bibee EN, Nanda K, Curtis KM. Safety of hormonal contraception and intrauterine devices among women with depressive and bipolar disorders: a systematic review. Contraception. 2016;94(6):641–649. doi:10.1016/j.contraception.2016.06.012
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
