Back to Journals » Journal of Multidisciplinary Healthcare » Volume 9
Improving nurse-physician teamwork through interprofessional bedside rounding
Authors Henkin S, Chon T , Christopherson M, Halvorsen A, Worden L, Ratelle J
Received 18 February 2016
Accepted for publication 8 March 2016
Published 2 May 2016 Volume 2016:9 Pages 201—205
DOI https://doi.org/10.2147/JMDH.S106644
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Stanislav Henkin,1 Tony Y Chon,2 Marie L Christopherson,3 Andrew J Halvorsen,1,4 Lindsey M Worden,3 John T Ratelle5
1Department of Medicine, Mayo Clinic, 2Division of General Internal Medicine, Mayo Clinic, 3Department of Nursing, Mayo Clinic, 4Department of Medicine, Internal Medicine Residency Office of Educational Innovations, Mayo Clinic, 5Division of Hospital Medicine, Mayo Clinic, Rochester, MN, USA
Background: Teamwork between physicians and nurses has a positive association with patient satisfaction and outcomes, but perceptions of physician–nurse teamwork are often suboptimal.
Objective: To improve nurse–physician teamwork in a general medicine inpatient teaching unit by increasing face-to-face communication through interprofessional bedside rounds.
Intervention: From July 2013 through October 2013, physicians (attendings and residents) and nurses from four general medicine teams in a single nursing unit participated in bedside rounding, which involved the inclusion of nurses in morning rounds with the medicine teams at the patients’ bedside. Based on stakeholder analysis and feedback, a checklist for key patient care issues was created and utilized during bedside rounds.
Assessment: To assess the effect of bedside rounding on nurse–physician teamwork, a survey of selected items from the Safety Attitudes Questionnaire (SAQ) was administered to participants before and after the implementation of bedside rounds. The number of pages to the general medicine teams was also measured as a marker of physician–nurse communication.
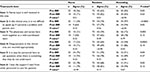
Results: Participation rate in bedside rounds across the four medicine teams was 58%. SAQ response rates for attendings, residents, and nurses were 36/36 (100%), 73/73 (100%), and 32/73 (44%) prior to implementation of bedside rounding and 36 attendings (100%), 72 residents (100%), and 14 (19%) nurses after the implementation of bedside rounding, respectively. Prior to bedside rounding, nurses provided lower teamwork ratings (percent agree) than residents and attendings on all SAQ items; but after the intervention, the difference remained significant only on SAQ item 2 (“In this clinical area, it is not difficult to speak up if I perceive a problem with patient care”, 64% for nurses vs 79% for residents vs 94% for attendings, P=0.02). Also, resident responses improved on SAQ item 1 (“Nurse input is well received in this area”, 62% vs 82%, P=0.01).
Conclusion: Increasing face-to-face communication through interprofessional bedside rounding can improve the perceptions of nurse–physician teamwork, particularly among residents and nurses.
Keywords: interprofessional care, teamwork, graduate medical education, hospital medicine
A letter to the editor has been published for this article
Introduction
Collaboration between physicians and nurses is essential for providing quality health care, and breakdown in this area is a major root cause of sentinel events.1 Indeed, improved perceptions of nurse—physician teamwork have been shown to be associated with higher satisfaction and better outcomes among hospitalized patients.2–5 Despite its importance, however, research has shown that teamwork between nurses and physicians is often suboptimal.6–8 Fortunately, structured interventions aimed to improve teamwork between nurses and physicians can succeed and have been shown to have a positive impact on teamwork and patient outcomes.9–11 Specifically, creating a system to involve nurses and physicians in rounds at the patient’s bedside can help create a shared mental model and increase collaborative activities.12
To improve the culture of teamwork on a general medical teaching unit at our institution, we designed a quality improvement (QI) project that incorporated nurses into daily bedside morning rounds with the physician team.
Methods
This QI project involved collaboration of physicians (both internal medicine residents and attendings) and nurses from four general medicine services on one 36-bed nursing unit of Mayo Clinic Hospital — Saint Mary’s Campus, Rochester, MN. Each general medicine service comprises three interns, one senior resident, and one attending physician. Residents rotate on the service in 4- or 5-week blocks, and attendings rotate in 2-week blocks.
In the spring of 2013, an interprofessional workshop was held to identify the barriers and opportunities for improving nurse—physician teamwork. The lack of face-to-face interaction on daily rounds was identified as a frequent source of communication breakdown and dissatisfaction. To address this gap, a formal process for interprofessional bedside rounding (IBR) was created. During IBR, each general medicine team would notify a patient’s nurse, through alphanumeric paging, when the team was rounding on that patient, so the nurse would meet the team at the patient’s bedside. This allowed for direct communication between the nurse and physician team, such that they were able to participate in rounds collaboratively.
IBR was piloted in small Plan—Do—Study—Act cycles during June 2013 with direct feedback solicited from participating nurses and physicians. Early responses to the pilot indicated that IBR interactions were frequently unstructured, and this sometimes led to ineffective communication. To address this barrier, a rounding “checklist” (Figure 1) was created and utilized by the nurse during IBR to ensure that key issues were addressed. The content of the checklist was derived from feedback of physician and nurse participants and input from the QI leadership team and included key patient care-related issues. Daily audits were performed by the charge nurse to assess the rates of participation. IBR was fully implemented on all the medicine teams at the start of the academic year in July 2013.
  | Figure 1 Interprofessional bedside rounding checklist. |
To measure the impact of IBR on nurse—physician teamwork, we used the teamwork climate items from the Safety Attitudes Questionnaire (SAQ) short form.13 The SAQ is a teamwork assessment tool scored on a 5-point Likert scale (1, strongly disagree; 3, neutral; 5, strongly agree).14 The SAQ has been shown to be reliable with known internal structure, criterion, and outcomes validity, and the teamwork climate items have been used in previous research regarding nurse—physician teamwork in a medical inpatient setting.15,16 Responses were solicited from 36 attendings, 73 residents, and 73 nurses before (May 2013) and 36 attendings, 72 residents, and 73 nurses after (October 2013) the intervention. To encourage participation in the project, surveys from physicians and nurses were submitted anonymously, and responses were not linked to demographic information such as age, sex, or years of experience.
Given their ordinal nature, the SAQ responses of strongly agree and agree were combined into “agree”, and the responses neutral, disagree, and strongly disagree were combined into “do not agree” for analysis. The number (percentage) of those who responded agree was reported by group for each SAQ item. Within-group and between-group survey responses were compared using Fischer’s exact tests.
As an additional measurement of the effect of IBR on nurse—physician communication, the total number of pages to the medicine service pagers (adjusted for patient census) was collected over a 30-day period before and after implementation of IBR and assessed using a Wilcoxon rank sum test.
According to the policy activities that constitute research at the Mayo Clinic, this study met the criteria for QI activities exempt from ethics review.
Results
SAQ responses were available from all (100%) attendings and residents before and after IBR, along with those from 32 nurses (44%) pre-IBR and 14 nurses (19%) post-IBR (Table 1). Average participation in IBR, defined as occurring when the physician team and nurse met at the patient’s bedside to discuss the plan of care, across all four medicine services during the QI project was 58%.
Within-group comparisons showed that after the implementation of IBR, resident agreement significantly improved on SAQ item 1 (“Nurse input is well received in this area”, 62% vs 82%, P=0.01). Between-group comparisons showed that prior to IBR, a significant difference existed between the nurses, residents, and attendings for all six SAQ items (Table 1), with nurses generally indicating lower SAQ responses than residents and attendings. Post-IBR, the differences in agreement between nurses, residents, and attendings remained significant only on SAQ item 2 (“In this clinical area, it is not difficult to speak up if I perceive a problem with patient care”, 64% vs 79% vs 94%, P=0.02).
Analysis of pages to the medicine service pagers revealed that after the implementation of IBR, there was a trend toward decreased number of pages per patient per day (7.5 vs 6.9, P=0.08).
Discussion
To our knowledge, this project is the first to assess the impact of IBR on nurse—physician teamwork in an internal medicine teaching unit. We found that the implementation of IBR led to improvement in several domains of teamwork between nurses and physicians. Our findings have implications for nursing and physician hospital administrators, as they attempt to improve interprofessional collaboration in inpatient medical units.
The positive effects of bedside interprofessional collaboration have been shown in other hospital practice settings such as obstetrics17 and the intensive care unit.10 As it relates to medical units specifically, our findings build upon the work of Sharma and Klocke,18 who evaluated the effect of IBR on a hospitalist unit and found similar improvement in perceptions of teamwork among nurses. In addition to teamwork perceptions, we also found a trend toward a reduction in page volumes to physicians by nurses, although this did not reach statistical significance. However, previous literature has shown that the effect of interventions on communication practices can be complex and difficult to predict and should be a focus of future research.19
Baseline attitudinal discrepancies regarding teamwork existed between providers, with physicians giving higher ratings than nurses. Similar findings have been shown in previous research of medical16 and nonmedical units,20 and high baseline perceptions of teamwork by physicians may explain why we did not find a significant improvement in SAQ scores of attendings after implementation of IBR. The reason for the difference in teamwork perceptions is likely multifactorial and may, in part, be related to hierarchical differences between physicians and nurses in the decision-making process.21,22 Further research is required to better understand these discrepant perceptions.
While we have shown that IBR appears to have a positive impact on nurse—physician teamwork, our project has limitations. SAQ responses were not linked to demographic data and were submitted anonymously, and therefore, they could not be paired for analysis. Response rates from nursing staff were lower than from residents and attendings, which likely limited the power with which to detect a significant improvement in SAQ scores for that group. This difference in response rate may have been due to difference in survey administration methods, as physicians were surveyed electronically, while nursing staff provided paper surveys.
The participation rate in IBR was consistently lower than our predetermined goal, which brings into question its sustainability, but our rates are similar to those of previous studies on IBR.23 Currently, we are working to overcome this barrier by promoting the use of a white board in the patient’s room, which contains prompts and space to write similar information to that outlined in the checklist. It can be updated by the physician team or nursing staff to allow for asynchronous communication, when IBR is not possible. Future steps in this will aim to promote sustainability and generalizability to other units and hospitals.
Conclusion
In summary, improving physician—nurse collaboration through IBR can positively impact perceptions of teamwork. Further work is required to understand the impact of IBR on patient satisfaction and outcomes.
Acknowledgment
This work was presented in poster form at Minnesota American College of Physicians on November 8, 2013 and in oral form at National American College of Physicians on April 11, 2014.
Disclosure
The authors report no conflicts of interest in this work.
References
Sentinel Event Data Root Causes by Event Type 2004 —2015. Available from: http://www.jointcommission.org/assets/1/18/Root_Causes_by_Event_Type_2004-2015.pdf. Accessed February 17, 2016. | ||
Baggs JG, Schmitt MH, Mushlin AI, et al. Association between nurse-physician collaboration and patient outcomes in three intensive care units. Crit Care Med. 1999;27(9):1991—1998. | ||
Meterko M, Mohr DC, Young GJ. Teamwork culture and patient satisfaction in hospitals. Med Care. 2004;42(5):492—498. | ||
Schmitt MH. Collaboration improves the quality of care: methodological challenges and evidence from US health care research. J Interprof Care. 2001;15(1):47—66. | ||
Davenport DL, Henderson WG, Mosca CL, Khuri SF, Mentzer RM Jr. Risk-adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions. J Am Coll Surg. 2007;205(6):778—784. | ||
Thomas EJ, Sexton JB, Helmreich RL. Discrepant attitudes about teamwork among critical care nurses and physicians. Crit Care Med. 2003;31(3):956—959. | ||
Nair DM, Fitzpatrick JJ, McNulty R, Click ER, Glembocki MM. Frequency of nurse-physician collaborative behaviors in an acute care hospital. J Interprof Care. 2012;26(2):115—120. | ||
O’Leary K, Ritter C, Wheeler H, Szekendi M, Brinton T, Williams M. Teamwork on inpatient medical units: assessing attitudes and barriers. Qual Saf Health Care. 2010;19(2): 117—121. | ||
O’Leary KJ, Buck R, Fligiel HM, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678—684. | ||
Narasimhan M, Eisen LA, Mahoney CD, Acerra FL, Rosen MJ. Improving nurse-physician communication and satisfaction in the intensive care unit with a daily goals worksheet. Am J Crit Care. 2006;15(2):217—222. | ||
Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072. | ||
McComb SA, Henneman EA, Hinchey KT, et al. Improving teamwork on general medical units: when teams do not work face-to-face. Jt Comm J Qual Patient Saf. 2012;38(10):471—478. | ||
Safety Attitudes: Frontline Perspectives from this Patient Care Area. Available from: https://med.uth.edu/chqs/files/2012/05/SAQ-Short-Form-2006.pdf. | ||
Sexton JB, Helmreich RL, Neilands TB, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006;6:44. | ||
Havyer RD, Wingo MT, Comfere NI, et al. Teamwork assessment in internal medicine: a systematic review of validity evidence and outcomes. J Gen Intern Med. 2014;29(6):894—910. | ||
O’Leary KJ, Wayne DB, Haviley C, Slade ME, Lee J, Williams MV. Improving teamwork: impact of structured interdisciplinary rounds on a medical teaching unit. J Gen Intern Med. 2010;25(8):826—832. | ||
Baldwin M, Hashima J, Guise JM, Gregory WT, Edelman A, Segel S. Patient-centered collaborative care: the impact of a new approach to postpartum rounds on residents’ perception of their work environment. J Grad Med Educ. 2010;2(1):62—66. | ||
Sharma U, Klocke D. Attitudes of nursing staff toward interprofessional in-patient-centered rounding. J Interprof Care. 2014;28(5):475—477. | ||
Quan SD, Wu RC, Rossos PG, et al. It’s not about pager replacement: an in-depth look at the interprofessional nature of communication in healthcare. J Hosp Med. 2013;8(3):137—143. | ||
Adler-Milstein J, Neal K, Howell MD. Residents’ and nurses’ perceptions of team function in the medical intensive care unit. J Crit Care. 2011;26(1):104.e7—115.e7. | ||
Zwarenstein M, Rice K, Gotlib-Conn L, Kenaszchuk C, Reeves S. Disengaged: a qualitative study of communication and collaboration between physicians and other professions on general internal medicine wards. BMC Health Serv Res. 2013;13:494. | ||
Gotlib Conn L, Reeves S, Dainty K, Kenaszchuk C, Zwarenstein M. Interprofessional communication with hospitalist and consultant physicians in general internal medicine: a qualitative study. BMC Health Serv Res. 2012;12:437. | ||
O’Leary KJ, Killarney A, Hansen LO, et al. Effect of patient-centred bedside rounds on hospitalised patients’ decision control, activation and satisfaction with care. BMJ Qual Saf. Epub 2015 Dec 1. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.