Back to Journals » Journal of Multidisciplinary Healthcare » Volume 12
Improvement in quality of life following a multidisciplinary rehabilitation program for patients with Parkinson’s disease
Authors Ritter VC, Bonsaksen T
Received 24 January 2019
Accepted for publication 22 February 2019
Published 20 March 2019 Volume 2019:12 Pages 219—227
DOI https://doi.org/10.2147/JMDH.S202827
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Victoria C Ritter,1 Tore Bonsaksen1,2
1Faculty of Health Sciences, Department of Occupational Therapy, Prosthetics and Orthotics, OsloMet – Oslo Metropolitan University, Oslo, Norway; 2Faculty of Health Studies, VID Specialized University, Sandnes, Norway
Background: Parkinson’s disease follows a chronic course, and therefore quality of life is important to assess in relation to rehabilitation programs for persons with the disease.
Aim: To examine whether a brief rehabilitation program can promote positive changes in functional status, general self-efficacy, and quality of life and to examine factors associated with changes in quality of life.
Methods: Patients with Parkinson’s disease (n=83) completed the General Self-Efficacy Scale and the Parkinson’s Disease Questionnaire at the beginning of a rehabilitation program and at three weeks follow-up. Within-person changes were analyzed with paired t-tests. A hierarchical linear regression was conducted to assess the independent associations between the independent variables and changes in quality of life during the three weeks program, while adjusting for the covariance between the independent variables.
Results: Patients reported higher functional status (d=0.37, p<0.001), general self-efficacy (d =0.28, p<0.01), and quality of life (d=0.32, p<0.001) at three weeks follow-up, compared to their baseline scores. The regression analysis showed that having a better initial functional status (β =−0.26, p<0.05) and lower quality of life (β =0.51, p<0.001) were associated with more improvements in quality of life.
Conclusion: The study suggests that actual functioning in persons with Parkinson’s disease is a better predictor of improved quality of life than self-efficacy beliefs and that those who have lower levels of initial quality of life benefit more from rehabilitation.
Keywords: functional status Parkinson’s disease, multidisciplinary rehabilitation program, self-efficacy, quality of life
Introduction
Parkinson’s disease can severely threaten self-efficacy and quality of life, and these factors may be reduced with disease progression. In a study by Fujii and coworkers on 143 patients with Parkinson’s disease in Tokyo, it was suggested that to increase self-efficacy among patients with Parkinson’s disease, social and psychological support and providing health education were important.1 Additionally, self-efficacy has been found to be important for effective disease management and for adherence to medication in chronic diseases, such as diabetes and juvenile chronic arthritis, suggesting that self-efficacy can predict disease management.2 These factors are also presumed to affect a person with Parkinson’s disease. Less depression and more well-being have been linked with individuals who feel mastery over life activities and maintain participation in them.3,4
Motor symptoms, such as tremor, rigidity and bradykinesia and non-motor symptoms, such as anxiety, depression, fatigue, cognitive impairment, sleep disorders and restless legs, can result in increased dependence in activities of daily living (ADLs), loss of autonomy, social isolation, and falls.5–8 Non-motor symptoms occur in 90% of the people with Parkinson’s disease, and research has shown that non-motor symptoms have a greater impact on health-related quality of life than motor symptoms alone.7,9 Reduced functional mobility and reduced ability to perform ADLs have been closely linked to quality of life in persons with Parkinson’s disease.10 Consequently, as Parkinson’s disease symptoms progress and worsen, maintaining independence in ADLs may decrease, resulting in reduced quality of life.
For several years, exercise-based programs have been the main intervention used when treating persons with Parkinson’s disease, and they have been identified as beneficial for improving both physical functioning and quality of life.5,11 Giardini and coworkers found that among persons with Parkinson’s disease, enhanced functioning and rediscovered autonomy were reported after intensive rehabilitation treatment.12 Consequently, with improved physical and functional capabilities, participants claimed to have gained better symptoms control and overall body control, denoting higher perceived self-efficacy. However, the weakness of exercise-based programs alone is that they do not necessarily address the specific non-motor symptoms occurring in Parkinson’s disease.7,13 When compared to a control group receiving care only from a general neurologist, patients in an intervention group receiving care from a movement disorder specialist, Parkinson’s disease nurses, and social workers, improved significantly in quality of life.14 This supports the notion that a multidisciplinary rehabilitation approach particularly tailored to the challenges experienced by patients with Parkinson’s disease can produce favorable outcomes. By addressing both motor and non-motor symptoms, multidisciplinary rehabilitation programs may be better equipped to assist the patient with Parkinson’s disease to self-manage their disease, to increase their self-efficacy, and ultimately to improve their quality of life.15 However, while some research studies indicate that rehabilitation programs can improve self-perceived performance in ADLs, general functioning, and quality of life,16–18 research on the effects of multidisciplinary rehabilitation programs on self-efficacy in persons with Parkinson’s disease is scarce.19
Furthermore, better exercise capacity and higher self-efficacy prior to starting a rehabilitation program have been associated with improved quality of life,20 and rehabilitation programs have been found to reduce the psychosocial impact of disease in a number of studies on chronic and progressive diseases, such as multiple sclerosis, chronic obstructive pulmonary disease, cancer, and myocardial infarction.20–23 This evidence suggests that self-efficacy is important to target in rehabilitation programs.20 However, to date, there are no similar studies concerned with patients with Parkinson’s disease.
The complexity of Parkinson’s disease and adverse burden pertained to living with the disease may pose challenges on sustaining self-efficacy and compromise quality of life. However, modern multidisciplinary rehabilitation programs, frequently including the expertise of occupational therapists, explicitly aim at increasing a person’s sense of self-efficacy15 and to inspire a patient’s sense of mastery in everyday challenges. Promoting self-efficacy through activities is also considered a core element of occupational therapy,24 and knowledge about self-efficacy and quality of life, and the associations between them may contribute to shape and strengthen therapy interventions for patients with Parkinson’s Disease.
Study aim. The aim of the study was to examine (i) whether positive changes in functional status, general self-efficacy, and quality of life occurred among patients with Parkinson’s disease after a brief multidisciplinary rehabilitation program and (ii) the factors associated with changes in quality of life.
Methods
Design and context
The study had a prospective longitudinal design. The data material was collected at a specialized rehabilitation center in Baerum, Norway.
Intervention
The multidisciplinary rehabilitation program had a duration of three weeks and was an inpatient program. Upon arrival, participants were awarded a primary contact to ensure a unified team working toward goals set by the participant him/herself. The multidisciplinary team consisted of 10 different professions, such as occupational therapists, physical therapists, doctors, neurologists, nurses, sports educators, cognitive behavioral therapists, and nutritionists.25 Commencing the multidisciplinary rehabilitation program, participants were assessed by the relevant professional/s and typically had close follow-up the first week with individual and group-based exercise. Participants would see the physical therapist individually at least three times a week, 30 mins each time, and when required participants would have one on one with the occupational therapist, speech therapist and/or the sports educator. The occupational therapist would assess cognitive impairment when needed and create a training program suitable for the participants’ needs. Additionally, participants had a weekly program set specifically up for him/her, containing disease-specific group-based exercises and physical activity group exercises not specific to disease that they were highly encouraged to attend every day. The training programs typically followed the neuroplasticity-principled Parkinson Wellness Recovery exercises with the intent of slowing disease progression, improve symptoms, restore function, and increase quality of life.26 To address non-motor symptoms, participants also had the option of going to disease-specific educational groups, where they, for example, would learn about nutrition and medication, talk to peers, and ask the professionals questions, and they had two weekly group-based speech therapy training sessions. Based on need, cognitive behavioral therapy was also available. Towards the end of the program, participants were expected to be able to perform individually tailored exercises and activities, with the aim of carrying it over to everyday life.
Participation recruitment and inclusion criteria
Patients with Parkinson’s disease (n=87) were individually recruited for the study upon arrival at the rehabilitation center during January 2018 through May 2018. All of the patients with Parkinson’s disease who were admitted during the study period were asked to participate in the study as long as they were admitted for treatment, met the diagnostic criteria, provided written informed consent, and were classified within Hoehn and Yahr stages I-IV.27 Hoehn and Yahr (H&Y) describe the different stages of Parkinson’s disease, from mild to severe, on an arbitrary staging scale from I to V.27 Stage I is characterized by unilateral involvement only with minimal or no functional disability, while stage V is characterized by confinement to bed or wheelchair unless aided. Eighteen (21.7%) participants were in Hoehn and Yahr stage I, 38 (45.8%) in stage II, 24 (28.9%) in stage III, and 3 (3.6%) participants were in stage IV.
Measures
The questionnaires (PDQ-39 and GSE: see below for description), used before and after the three weeks rehabilitation program were handed out the first day with written and verbal instructions. A sociodemographic questionnaire containing age, gender, level of education, and Parkinson’s disease duration was included in the handout. Scores on functional status by the MiniBestTest (MBT)28 were later extracted from participants’ records upon completion of the rehabilitation program.
The Parkinson’s Disease Questionnaire 39 was developed for assessing quality of life in persons with Parkinson’s disease29 and has been found to have satisfactory internal consistency (Cronbach’s α = 0.89) and convergent validity in relation to the Hoehn and Yahr (r=0.51, p˂0.001).29,30 Test–retest reliability has been found to be adequate (r ranging 0.79–0.93).31 The instrument consists of 39 questions addressing the issues of mobility, ADLs, emotional well-being, stigma, social support, cognition, communication, and bodily discomfort. For all the items on the 8-step scale, the respondents are asked to indicate how often they experience difficulties ranging from “never” to “always or cannot do at all”. The score range is 39–195, with higher scores indicating lower quality of life. The change score was calculated by subtracting the follow-up score from the initial score; thus, a more positive change score reflected more improvements in quality of life.
The General Self-efficacy Scale consists of 10 items (scored 1–4; “not at all true” to “exactly true”) and was designed to assess optimistic self-beliefs related to coping with a variety of demands in life.32 The scale explicitly refers to personal agency, ie, the belief that one’s actions are the cause of successful outcomes. It is a well-known and accepted instrument that measures one underlying construct of general self-efficacy.33 Score range is 10–40, with higher scores indicating higher general self-efficacy.
Functional status was measured with the MBT,28 and the assessment was performed by the physical therapist. The MBT is a tool that was developed for predicting a person’s likelihood of falls by assessing dynamic balance.28 The MBT is composed of 14 items on a 3-level ordinal scale, with higher scores indicating higher functional status. The participant demonstrates specific tasks and is subsequently classified as having normal functioning (2 points), moderate problems (1 point), or severe problems (0 points). Higher scores indicate less risk of falling.
Data analysis
Scale scores were computed provided that the participants had less than 20% missing scores on the relevant scale items. In the eventual case of missing values, values were replaced with the mean of the completed items. Cases with missing values subsequent to the replacement procedure were deleted analysis by analysis (casewise deletion). Thus, n varied between analyses.
Initial descriptive analyses used means (M) and standard deviation (SD) for continuous variables and frequencies and percentages for categorical variables. Internal consistency of the PDQ-39 scale and the general self-efficacy scale were examined with Cronbach’s α, and coefficients exceeding 0.70 were considered acceptable.
Several methods were employed to assess scores distribution on the scale. We found that the mean and median values were fairly similar, measures of skewness were all within the generally accepted limits (skewness <2), and the visual inspection of Q–Q plots, histogram, and box plot indicated a distribution resembling the normal distribution. However, the baseline measures of functional status, general self-efficacy, and quality of life produced significant Kolmogorov–Smirnov test results. Thus, non-parametric tests were conducted to ensure that the same results were produced by the two methods of statistical testing. As the results were the same, we decided to proceed with parametric analyses as appropriate.
Independent t-tests and Chi-Square tests were conducted to analyze differences between men and women. Paired t-tests were conducted to analyze the differences in mean scores (functional status, general self-efficacy, and quality of life) between baseline and three weeks follow-up. Non-parametric tests were conducted to ensure same results. A hierarchical linear regression analysis was conducted to assess the independent associations between the independent variables and changes in the quality of life scale score while adjusting for the covariance between the independent variables. There were two subsequent models, where Model 1 included the independent demographic variables age, gender, and education. Model 2 also included Parkinson’s disease duration, functional status (MBT), baseline general self-efficacy scores, and baseline quality of life scores. All data were analyzed using the statistical software IBM SPSS 25 for Windows.34 Statistical significance was set at p<0.05.
Ethics
Prior to commencing the study, approval from the Norwegian Regional Committee for Medical and Health Research Ethics (project number 2017/1584) was obtained. Participants provided a written informed consent to participate in the study, after having been informed that participation was voluntary, that opting not to participate would not adversely affect their rehabilitation, and that their responses would be treated in confidence. The study was conducted in accordance with the Declaration of Helsinki.
Results
Sample characteristics
One person did not meet the inclusion criteria, two left the rehabilitation center after only a few days for various reasons, and one left without filling out the questionnaires. These were all removed from the data set prior to the analyses.
The sociodemographic characteristics of the sample are displayed in Table 1. Eighty-three (n=83) participants completed the measures at baseline and at three weeks follow-up, and these constituted the study sample. Among the participants, the mean age of the sample was 69.0 years (SD =8.3 years), with 48 being male (57.8%) and 35 (42.2%) female. The sample’s mean Parkinson’s disease duration was 5.0 years (SD=3.7 years). Fifty-one participants (63.0%) reported having three years of higher education or more.
 | Table 1 Characteristics of the study participants |
Internal consistency for the quality of life scale (valid for 72.3% of the sample) was Cronbach’s α =0.94, and for the general self-efficacy scale (valid for 91.6% of the sample) Cronbach’s α =0.91, thus, indicating very good internal consistency. Mean scores for baseline general self-efficacy was 25.3 (SD=6.8) for women and 26.5 (SD=6.2) for men (ns). The mean scores for baseline quality of life for women were 82.2 (SD=20.6) and 76.8 (SD=20.7) for men (ns). The mean score for baseline functional status (MBT) for women was 23.6 (SD=3.8) and 23.0 (SD=3.9) for men (ns).
Changes in functional status, general self-efficacy, and quality of life
Functional status scores changed from baseline (M=23.5, SD=3.3) to three weeks follow-up (M =24.7, SD=3.1, p<0.001, Cohen’s d =0.37), suggesting improved functional status at three weeks follow-up. There was a change in general self-efficacy score from baseline (M=26.0, SD=6.2) to three weeks follow-up (M =27.8, SD=6.7, p<0.01, Cohen’s d =0.28), suggesting higher general self-efficacy at three weeks follow-up. Lastly, quality of life changed from baseline (M=77.9, SD=19.6) to three weeks follow-up (M=71.7, SD=18.6, p<0.001, Cohen’s d =0.32), denoting improved quality of life at follow-up.
Associations with changes in quality of life
Table 2 shows the results from the regression analyses. Hierarchical linear regressions were conducted to assess associations between each of the independent variables and the changes in quality of life. In Model 1, the demographic variables age, gender, and education explained 7.6% (ns) of the outcome variance. When included in Model 2, Parkinson’s disease duration, functional status (MBT), baseline general self-efficacy and baseline quality of life explained an additional 20.9% of the total variance in quality of life change. Better functional status (MBT; β =0.26, p<0.05) and lower baseline quality of life (β =0.51, p<0.001) were significantly associated with more improvements in quality of life.
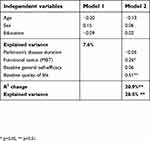 | Table 2 Hierarchical linear regression analyses showing direct associations with changes in quality of life |
The changes in quality of life scores as moderated by initial levels of functioning and quality of life are presented in Figures 1 and 2. For those with initial levels of functioning at the median value (Md =24.0) or higher, quality of life improved markedly between baseline (M =72.6, SD=22.3) and three weeks follow-up (M=62.1, SD=15.4, p<0.001, Cohen’s d=0.55). For those with initial levels of functioning lower than the median value, quality of life improved, but not as markedly, from baseline (M=78.4, SD=16.3) to three weeks follow-up (M=74.5, SD=17.2, p<0.01, Cohen’s d=0.23).
 | Figure 1 Changes in quality of life moderated by initial functional status. |
 | Figure 2 Changes in quality of life moderated by initial quality of life scores. |
For those with initial quality of life scores lower than the median value (Md=77.0: ie, those with better quality of life), quality of life improved from baseline (M=61.8, SD=8.3) to three weeks follow-up (M=58.5, SD=9.9, p<0.01, Cohen’s d=0.37). For those with initial quality of life scores at the median value or above (ie, those with poorer quality of life), quality of life improved markedly from baseline (M=95.3, SD=11.7) to three weeks follow-up (M=86.1, SD =15.1, p<0.001, Cohen’s d =0.68). In other words, participants who had better initial functioning, and lower initial quality of life, increased their quality of life more in comparison to their counterparts.
Discussion
To the best of our knowledge, this is the first study to examine changes in quality of life and factors associated with the change, during a three-week rehabilitation program for patients with Parkinson’s disease. The study suggests that a three-week multidisciplinary rehabilitation program can promote positive change in functional status, general self-efficacy, and quality of life. Moreover, the regression models showed that higher baseline functional status and lower baseline quality of life levels were associated with more improvement in quality of life.
Our results showed that functional status, general self-efficacy, and quality of life improved from baseline to three weeks follow-up. On average, participants saw a 1.2 point improvement in functional status (MBT), 1.8 point improvement in general self-efficacy, and a 6.2 point improvement in quality of life. The minimal clinically detectable change in PDQ-39 has been found to be −4.72/+4.22 (improvement/worsening),35 thus, denoting that the improvements found in our study would be of significance to the participants. The improvement in quality of life is fairly similar to that found in Ferrazzoli and colleagues’ study where an 8.3 point improvement was reported following a 10-week multidisciplinary rehabilitation intervention.18 Additionally, their improvement sustained, although not as markedly, at the four-month follow-up. In comparison, our study was one of a relatively short duration, which could explain the short-term improvements, and did not include a follow-up assessment beyond the three-week follow-up.
After completing the baseline functional status testing, one would assume that the adversities that were found, among others, became targeted in the exercise program the participants underwent and worked on during their three-week multidisciplinary rehabilitation program. Consequently, one explanation for the increase in the reported functional status could be that the participants worked on improving the physical adversities during the rehabilitation program. Improved functioning has similarly been found in other studies.17,36 Additionally, the multidisciplinary rehabilitation program may have provided tools for participants to better self-manage their disease, resulting in higher general self-efficacy at follow-up. Thus, higher levels of quality of life at the end of the rehabilitation program could be an effect of improved functioning and general self-efficacy.1,2,10,18 Another explanation for the positive results could be that the participants experienced that there is hope, even for a progressive disease such as Parkinson’s disease, although there is no cure.37,38
When including Parkinson’s disease duration, functional status, baseline general self-efficacy, and baseline quality of life in Model 2 of the regression analyses, we found better initial functional status and lower initial levels in quality of life to be associated with more improvements in quality of life. One interpretation of the findings is that participants who had better initial functional status were able to utilize and benefitted more from the rehabilitation program compared with those with poorer who reported lower initial functional status. Moreover, participants with poorer initial levels of functional status may be in need of a rehabilitation program of longer duration to benefit from it. Reduced functional status has been linked with reduced independence, inability to perform ADLs, and decreased mobility.39,40 As symptoms are worse, participants’ scores in functional status would reflect this notion. Thus, substantial improvements in quality of life among those with poorer functioning appear less likely.
A broadly composed measure of quality of life, like the PDQ-39, is likely to be quite stable over time, reflecting that quality of life is in fact a more generic concept than, for example, emotions tied to immediate circumstances. In addition, the shorter the time span between the measurements, the stronger the association between quality of life scores. One could, therefore, expect patients who initially report higher baseline quality of life to report higher follow-up quality of life. Results supporting this idea have been found in a study of stroke patients who participated in a rehabilitation program (mean duration of 57 days), where baseline quality of life was found to predict follow-up quality of life.41
Given the brevity of the rehabilitation program provided in our study, we found it more appropriate to associate initial measures with changes in quality of life instead of the follow-up measure. We found that higher initial quality of life scores (ie, lower quality of life) was strongly associated with more improvement in quality of life at three weeks follow-up. Clearly, participants with lower initial levels of quality of life indicated that the participants had troubled feelings about their performance capacity and other aspects of their life circumstances. However, considering the two findings in combination may be worthwhile. During the rehabilitation program, those with better functional capacity would likely be those who could more readily change their performance of daily life activities, and subsequently their beliefs and feelings related to their life circumstances in a more general sense. Those with poorer initial functioning may not have experienced similar changes in what they can do in their daily life, and therefore, their quality of life have may not have been as susceptible to change. Thus, the combined results indicate that those with better initial functioning, but who were inclined toward considering their own functioning and general life circumstances as poor, had the best prospects of improving quality of life over the course of a brief program.
To illustrate the main findings from the regression analysis (see Table 2), we examined how the changes in quality of life were moderated by the participants’ initial functional status and quality of life. The results showed that baseline levels of these measures moderated the changes in quality of life, most apparent in the sharp improvement for those whose initial quality of life was in the poorer half of the scores (see Figures 1 and 2). However, the participants with the sharpest improvement still reported poorer quality of life compared with the participants who reported better initial quality of life.
Study limitations
This study is limited by a relatively small sample size. The sample was also one of convenience, thus, generalizations should be made with caution. Participants may have interpreted the questionnaires differently as well as becoming disinterested while filling them out, possibly resulting in skewed results. We used a general measure for measuring quality of life. However, one could assume that certain aspects of quality of life change more, while others change less, but this is not assessed in the present study.
The participants’ level of activity throughout the stay was not recorded. Participation may have varied substantially from person to person, which could have affected the results. Which activities the individual patient participated in during the multidisciplinary rehabilitation program was not accounted for, and future studies should report more clearly both the level and the content of activity participation during the rehabilitation program. Medication, and/or adjustment of medication during the stay, was not accounted for, and this could have influenced the results. Additionally, we report findings from a brief rehabilitation program, and sustained changes are not reported. With this in mind, one should, therefore, use these results with caution.
Conclusion
This study showed that persons with Parkinson’ disease reported positive changes in functional status, general self-efficacy, and quality of life following a brief multidisciplinary rehabilitation program. Participants with higher functional status and lower levels of quality of life at the beginning of the rehabilitation program, reported more improvement in quality of life at three weeks follow-up, compared to their counterparts. Moreover, the study suggests that actual functioning in persons with Parkinson’s disease is a better predictor of improved quality of life than self-efficacy beliefs and that those who have lower levels of initial quality of life benefit more from rehabilitation.
Data Availability
The dataset used to support the findings of this study will be available from the authors on reasonable request when the research project is completed.
Acknowledgment
The interest in the study is greatly appreciated, and the authors are grateful for the responses from the participants.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fujii C, Aoshima T, Sato S, Mori N, Ohkoshi N, Oda S. Self-efficacy and related factors related in Parkinson’s disease patients. [Nihon koshu eisei zasshi] Jpn J Public Health. 1997;44(11):817–826.
2. Cramm J, Strating M, Nieboer A. The importance of general self-efficacy for the quality of life of adolescents with diabetes or juvenile rheumatoid arthritis over time: a longitudinal study among adolescents and parents. Front Pediatr. 2013;1(40). doi:10.3389/fped.2013.00040
3. Holroyd S, Currie LJ, Wooten GF. Depression is associated with impairment of ADL, not motor function in Parkinson disease. Neurology. 2005;64(12):2134–2135. doi:10.1212/01.WNL.0000165958.12724.0D
4. Livneh H, Antonak RF. Review of research on psychosocial adaptation to neuromuscular disorders: I. Cerebral palsy, muscular dystrophy, and Parkinson’s disease. J Soc Behav Pers. 1994;9(5):201–230.
5. Cascaes Da Silva F, Da Rosa Lop R, Domingos Dos Santos P, Aguiar Bezerra de Melo LM, Barbosa Gutierres Filho PJ, Da Silva R. Effects of physical-exercise-based rehabilitation programs on the quality of life of patients with Parkinson’s disease: A systematic review of randomized controlled trials. J Aging Phys Activ. 2016;24(3):484–496. doi:10.1123/japa.2015-0162
6.
7. Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM, Chaudhuri KR. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov Disord. 2011;26(3):399–406. doi:10.1002/mds.23462
8.
9. Barone P, Antonini A, Colosimo C, et al. The PRIAMO study: a multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov Disord. 2009;24(11):1641–1649. doi:10.1002/mds.22643
10. Reuther M, Spottke EA, Klotsche J, et al. Assessing health-related quality of life in patients with Parkinson’s disease in a prospective longitudinal study. Parkinsonism Relat Disord. 2007;13(2):108–114. doi:10.1016/j.parkreldis.2006.07.009
11. Cusso ME, Donald KJ, Khoo TK. The impact of physical activity on non-motor symptoms in Parkinson’s disease: A systematic review. Front Med. 2016;3:35. doi:10.3389/fmed.2016.00035
12. Giardini A, Pierobon A, Callegari S, et al. Towards proactive active living: patients with Parkinson’s disease experience of a multidisciplinary intensive rehabilitation treatment. Eur J Phys Rehabil Med. 2017;53(1):114–124. doi:10.23736/S1973-9087.16.04213-1
13. Keus S, Munneke M, Graziano M, et al. [Homepage on Internet] The Netherlands: European Physiotherapy Guideline for Parkinson’s Disease.
14. van der Marck MA, Bloem BR, Borm GF, Overeem S, Munneke M, Guttman M. Effectiveness of multidisciplinary care for Parkinson’s disease: a randomized, controlled trial. Mov Disord. 2013;28(5):605–611. doi:10.1002/mds.25194
15.
16. Sturkenboom IH, Graff MJ, Hendriks JC, et al. Efficacy of occupational therapy for patients with Parkinson’s disease: a randomised controlled trial. Lancet Neurol. 2014;13(6):557–566. doi:10.1016/S1474-4422(14)70055-9
17. Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL. The effectiveness of exercise interventions for people with Parkinson’s disease: a systematic review and meta-analysis. Mov Disord. 2008;23(5):631–640. doi:10.1002/mds.21922
18. Ferrazzoli D, Ortelli P, Zivi I, et al. Efficacy of intensive multidisciplinary rehabilitation in Parkinson’s disease: a randomised controlled study. J Neurol Neurosurg Psychiatry. 2018;89(8):828–835. doi:10.1136/jnnp-2017-316437
19. Tan SB, Williams AF, Kelly D. Effectiveness of multidisciplinary interventions to improve the quality of life for people with Parkinson’s disease: a systematic review. Int J Nurs Stud. 2014;51(1):166–174. doi:10.1016/j.ijnurstu.2013.03.009
20. Bentsen SB, Wentzel-Larsen T, Henriksen AH, Rokne B, Wahl AK. Self-efficacy as a predictor of improvement in health status and overall quality of life in pulmonary rehabilitation - an exploratory study. Patient Educ Couns. 2010;81(1):5–13. doi:10.1016/j.pec.2009.11.019
21. Brink E, Alsen P, Herlitz J, Kjellgren K, Cliffordson C. General self-efficacy and health-related quality of life after myocardial infarction. Psychol Health Med. 2012;17(3):346–355. doi:10.1080/13548506.2011.608807
22. Heckman JE, Chamie K, Maliski SL, et al. The role of self-efficacy in quality of life for disadvantaged men with prostate cancer. J Urol. 2011;186(5):1855–1861. doi:10.1016/j.juro.2011.06.059
23. Motl RW, McAuley E, Wynn D, Sandroff B, Suh Y. Physical activity, self-efficacy, and health-related quality of life in persons with multiple sclerosis: analysis of associations between individual-level changes over one year. Qual Life Res. 2013;22(2):253–261. doi:10.1007/s11136-012-0149-z
24.
25.
26.
27. Hoehn MM, Yahr MD. Parkinsonism: onset, progression, and mortality. 1967. Neurology. 2001;57(10 Suppl 3):S11–S26.
28. Franchignoni F, Horak F, Godi M, Nardone A, Giordano A. Using psychometric techniques to improve the balance evaluation systems test: the mini-BESTest. J Rehabil Med. 2010;42(4):323–331. doi:10.2340/16501977-0537
29. Peto V, Jenkinson C, Fitzpatrick R, Greenhall R. The development and validation of a short measure of functioning and well being for individuals with Parkinson’s disease. Qual Life Res. 1995;4(3):241–248.
30. Jenkinson C, Fitzpatrick RAY, Peto VIV, Greenhall R, Hyman N. The Parkinson’s Disease Questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Age Ageing. 1997;26(5):353–357.
31. Hagell P, Nygren C. The 39 item Parkinson’s disease questionnaire (PDQ-39) revisited: implications for evidence based medicine. J Neurology Neurosurg Psychiatry. 2007;78(11):1191–1198. doi:10.1136/jnnp.2006.111161
32. Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in Health Psychology: a User’s Portfolio. Winsor (UK): Nfer-Nelson; 1995:35–37.
33. Scholz U, Dona BG, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur J Phsychol Assess. 2002;18:242–251. doi:10.1027//1015-5759.18.3.242
34.
35. Horváth K, Aschermann Z, Kovács M, et al. Changes in quality of life in Parkinson’s Disease: how large must they be to be relevant? Neuroepidemiology. 2017;48(1–2):1–8. doi:10.1159/000455863
36. Frazzitta G, Maestri R, Ferrazzoli D, et al. Multidisciplinary intensive rehabilitation treatment improves sleep quality in Parkinson’s disease. J Clin Mov Dis. 2015;2(11):1–8.
37. Soundy A, Stubbs B, Roskell C. The experience of Parkinson’s Disease: A systematic review and meta-ethnography. Scientific World J. 2014;2014:19. doi:10.1155/2014/613592
38. Schiavon CC, Marchetti E, Gurgel LG, Busnello FM, Reppold CT. Optimism and hope in chronic disease: A systematic review. Front Psychol. 2016;7:1–10.
39. Lawrence BJ, Gasson N, Kane R, Bucks RS, Loftus AM. Activities of daily living, depression, and quality of life in Parkinson’s disease. PLoS One. 2014;9(7):e102294. doi:10.1371/journal.pone.0102294
40. Trend P, Kaye J, Gage H, Owen C, Wade D. Short-term effectiveness of intensive multidisciplinary rehabilitation for people with Parkinson’s disease and their carers. Clin Rehabil. 2002;16(7):717–725. doi:10.1191/0269215502cr545oa
41. Katona M, Graessel E, Schmidt R, Schupp W. Predictors of health-related quality of life in stroke patients after neurological inpatient rehabilitation: a prospective study. Health Qual Life Outcomes. 2015;13(1):1–7. doi:10.1186/s12955-014-0204-2
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
