Back to Journals » Nutrition and Dietary Supplements » Volume 8
Importance of low carbohydrate diets in diabetes management
Authors Hall R, Parry Strong A, Krebs J
Received 7 July 2015
Accepted for publication 14 October 2015
Published 17 March 2016 Volume 2016:8 Pages 9—19
DOI https://doi.org/10.2147/NDS.S74719
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gary Johanning
Rosemary M Hall, Amber Parry Strong, Jeremy D Krebs
Centre for Endocrine, Diabetes and Obesity Research, Capital and Coast District Health Board, Wellington, New Zealand
Abstract: Dietary strategies are fundamental in the management of diabetes. Historically, strict dietary control with a low carbohydrate diet was the only treatment option. With increasingly effective medications, the importance of dietary change decreased. Recommendations focused on reducing dietary fat to prevent atherosclerotic disease, with decreasing emphasis on the amount and quality of carbohydrate. As the prevalence of obesity and diabetes escalates, attention has returned to the macronutrient composition of the diet. Very low carbohydrate diets (VLCD's) have demonstrated effective initial weight loss and improvement in glycemic control, but difficult long-term acceptability and worsening lipid profile. Modifications to the very low carbohydrate (VLC) have included limiting saturated fat and increasing carbohydrate (CHO) and protein. Reducing saturated fat appears pivotal in reducing low-density lipoprotein (LDL) cholesterol and may mitigate adverse effects of traditional VLCD's. Increased dietary protein enhances satiety, reduces energy intake, and improves glycemic homeostasis, but without sustained improvements in glycemic control or cardiovascular risk over and above the effect of weight loss. Additionally, recent studies in type 1 diabetes mellitus suggest promising benefits to diabetes control with low carbohydrate diets, without concerning effects on ketosis or hypoglycemia. Dietary patterns may highlight pertinent associations. For example, Mediterranean-style and paleolithic-type diets, low in fat and carbohydrate, are associated with reduced body weight and improved glycemic and cardiovascular outcomes in type 2 diabetes mellitus (T2DM). A feature of these dietary patterns is low refined CHO and sugar and higher fiber, and it is possible that increasing sugar consumption is having a substantial effect on global escalations in obesity and T2DM. Dietary recommendations in type 1 diabetes and T2DM are changing. Dietary CHO is unquestionably important, but long-term acceptability of any diet is critical to sustain improvements in health benefits. Personalized dietary management, using a variety of dietary approaches, may be the key to optimal diabetes outcomes.
Keywords: low carbohydrate diets, type 2 diabetes, dietary intervention studies, type 1 diabetes, paleo nutrition
Introduction
Effective dietary strategies to prevent the onset of diabetes or manage its associated complications are critical to address the continuous rise in obesity and T2DM. Despite current recommendations for diet and lifestyle approaches, obesity and T2DM have reached epidemic proportions worldwide with major implications for individual health outcomes and health care resources.1 The development of obesity and its associated complications is a result of complex multifactorial interactions between the environment and the individual, with dietary factors underpinning these interactions. Dietary strategies remain the key to the treatment of diabetes and management of glucose homeostasis and risk factors for cardiovascular disease. Recent debate has focused on appropriate dietary advice and whether current dietary recommendations are optimal for prevention and management of T2DM, particularly with respect to a focus on macronutrient composition or dietary pattern.
Historical dietary management of diabetes
Prior to the discovery of insulin, type 1 diabetes was managed with low carbohydrate, low energy diets.2 Once discovered, insulin was found to be so effective that the importance of diet waned and patients were medically treated in preference to modifying diet and exercise. Despite the use of insulin, the composition of the diet still favored a reduction in carbohydrate with fairly equal proportions of daily energy intake coming from carbohydrate, protein, and fat.
In the 1950s, the relationship between plasma lipoprotein and atherosclerotic heart disease was identified and a report to the American Heart Association in 1957 suggested that dietary fat, particularly the ratio between saturated and unsaturated fat, may be an important determinant in the pathogenesis of atherosclerosis.3,4 In response to this suggestion, and subsequent epidemiological data, by 1977 the dietary guidelines for the US recommended an increase in carbohydrate consumption to 55%–60% of energy, a decrease in fat to 30% of energy with a reduction in saturated fat and cholesterol consumption, and a decrease in sugar consumption to 15% of total energy intake. Recognizing that T2DM was an additional risk factor for atherosclerotic heart disease, these recommendations were adopted for the management of diabetes. Randomized controlled trials at this time suggested a benefit for blood glucose control and a reduction in total cholesterol when high carbohydrate–low fat diets were adopted in people with T2DM.5–7 Notably, these diets emphasized complex unrefined carbohydrates which were high in fiber, and were comprised of larger proportions of mono and polyunsaturated fats relative to saturated fat. For many years, this has been the standard dietary recommendation for those with T2DM.
As the incidence of obesity and T2DM continues to rise, there has been renewed debate and the appearance of numerous alternative diets in the search for the optimal diet to prevent and manage obesity and diabetes. Additionally, the actual composition and consumption of the high carbohydrate–low fat diet has changed substantially from that originally recommended. The availability of caloric sweeteners increased by 23% from 1984 to 2000.8 Sugar intake has increased and average fiber consumption has decreased, and these shifts have paralleled the rise in T2DM during the 20th century.9
Optimal diet in T2DM
The three fundamental components of managing diabetes are promoting weight loss or weight maintenance, improving glycemic control, and preventing or reducing the risk of microvascular and macrovascular complications. Dietary composition is integral to overall diabetes management and recommendations for a particular diet must consider all these components.
Diet and weight regulation
Determining the relationship between specific dietary components and obesity is limited by the complexity of eating behavior and food intake in humans. If food consumption is under-reported, nutrient intake will be underestimated or inaccurate so that identifying a nutrient-specific role in the development and therefore the management of obesity is difficult. Moreover, it is recognized that under-reporting of total energy and fat intake is a greater problem in overweight and obese individuals.10,11 Dietary patterns have therefore been explored to investigate whether a broader group of food or nutrients may be more closely associated with obesity. Diets high in fat or sugar and low in fiber have been associated with obesity, while a change to a diet lower in fat and sugar and high in fiber over 10 years resulted in a reduction in Body Mass Index (BMI) in obese women and less increase in BMI in lean women.12 In children, high fat, low fiber, and energy dense dietary patterns are associated with an increase in fat mass and linked to excess gain in body mass.13 The Mediterranean-style diet, a classic dietary pattern characterized by a high consumption of vegetables, monounsaturated fatty acids, primarily from olive oil, fruits, cereals, and legumes, a low consumption of red or processed meat, and a low to moderate consumption of red wine during meals, has been associated with lower body weight, improved glycemic outcomes, and improved cardiovascular risk in people with T2DM.14 These diets suggest that, among other factors, lower sugar intake and less refined carbohydrate may be beneficial in obesity and T2DM and therefore promoting such diets may be advantageous.15
One mechanism by which dietary patterns may influence body weight is the effect of macronutrients on satiety and energy intake. Satiety and subsequent energy intake appear to be linked to the ability to store or utilize dietary energy and so macronutrients that are tightly regulated, protein and carbohydrate, have more effect on subsequent energy intake and energy balance.16–18 There is limited ability to store protein, and protein oxidation is closely linked to protein intake.17,19 Conversely, the ability to store fat is large, and there appears to be almost no autoregulation between fat intake and fat oxidation, leading to fat storage when intake is in excess.20 Excess total energy consumption leads to excess body weight. However, numerous studies using a meal preload design have suggested that increasing the proportion of energy from protein, and reducing carbohydrate, increases satiety and decreases subsequent energy intake.21–27 Additionally, weight regain is less after weight loss in free-living individuals.16,28
Very low carbohydrate diets
Weight loss
The widespread interest in popular low carbohydrate diets, particularly the Atkins diet,29 among people with obesity and metabolic disease led to randomized controlled intervention studies aiming to determine their efficacy and safety.
When the Atkins diet was adopted by community-based free-living obese subjects with either minimal dietary advice (n=63)30 or regular dietary instruction (n=132),31 weight loss was greater in the Atkins group after 6 months (−7.0%±0.8% vs −3.2%±0.7%, minimal advice and −4.5%±0.8% vs 1.44%±0.2%, regular advice), but was not sustained at 12 months.32
In patients with T2DM, an “Atkins”-type diet results in significant weight loss up to 24 weeks.33 The primary reduction in carbohydrate produces only a small reciprocal increase in protein and fat and therefore a reduction in total energy intake.34,35 A systematic review demonstrated that low carbohydrate, Atkins-type diets were more effective at reducing weight than low fat, low energy diets over 6 months. Additionally, low carbohydrate, high protein diets were at least as effective as low fat diets up to 1 year.36 There are substantial limitations to these data. Studies in those with diabetes are limited and no studies have demonstrated long-term sustained weight loss in obesity or T2DM beyond 12 months.37
Glycemic control
The acute response to a substantial reduction in dietary carbohydrate is a significant effect on glucose metabolism. Reduced glucose and insulin concentration and improved glycemic control have been demonstrated in several small and very short studies ranging from 7 days to 5 weeks38–40 with postprandial glucose curves normalizing in at least one study.35 In short-term studies, people with T2DM require less antidiabetic agents to control glucose levels and achieve improvements in glycated hemoglobin (HbA1c).33,34,37 In some studies, these improvements are greater with a very low carbohydrate diet compared with other approaches,41 but data are not consistent and there are no long-term studies convincingly demonstrating any greater benefit on HbA1c from VLCD’s. Davis et al demonstrated similar modest weight loss but no significant improvement in glycemic control in those with T2DM on a low fat or low carbohydrate diet after 1 year.42 In the longest very low carbohydrate diet trial currently reported, a −0.9% reduction in HbA1c at 2 years was achieved compared with −0.5% in a Mediterranean diet and −0.4% in a low fat diet; however, the difference between groups was not significant. Only a small proportion of the study group had diabetes, limiting the power of this conclusion.43 Recently, Tay et al reported on a randomized controlled study investigating hypocaloric low carbohydrate versus high carbohydrate diets over 24 weeks and 1 year, respectively, in obese adults with T2DM.44,45 Saturated fat intake was limited to <10% despite total fat intake being 58% and carbohydrate 14% of the total energy intake in the low carbohydrate group. Intensive dietary counseling and a physical activity plan were included. With weight loss being the same in both groups, analysis focused on the intrinsic differences in the diets per se. There was a suggestion of improved glycemic control with reduced glycemic variability and a reduction in medication requirement, but no difference in HbA1c was observed. This suggests great interindividual variability and the glycemic effect of the very low carbohydrate diet are undoubtedly influenced by the ability to maintain the diet on a daily basis over the long-term.
Cardiovascular disease risk
Long-term consumption of a VLCD has raised concerns of the potential for increased dietary saturated fat to detrimentally affect the lipid profile and therefore cardiovascular risk. The initial change in lipid profile observed when these diets are adopted is a dramatic decrease in triglyceride concentration with some increase in LDL cholesterol. In the setting of weight loss, a beneficial reduction in LDL cholesterol has been demonstrated alongside a reduction in triglycerides and an increase in high density lipoprotein (HDL) cholesterol over 24 weeks.33 A systematic review demonstrated that low carbohydrate, Atkins-type diets improved cardiovascular disease risk factors, assessed by favorable effects on high-density lipoprotein cholesterol, triacylglycerols, and systolic blood pressure, to a greater degree than low fat, low energy diets over 6 months.36 However, the effect was diminished after 1 year when weight change was equivalent, highlighting the importance of weight loss per se to improve lipid profiles, perhaps irrespective of the diet composition.36 Of concern are recent data suggesting that increasing LDL cholesterol in the Atkins diet may have detrimental effects on vascular function.44 Additionally, it is questionable whether the increase in HDL provides any meaningful benefit, further compounding the adverse effect of a VLCD in obesity and T2DM. However, these adverse effects may be overcome. Tay et al demonstrated that maintaining saturated fat to the recommended level below 10% prevents increases in LDL cholesterol seen with traditional low carbohydrate high fat diets.45 Intensive dietary counseling was required to sustain the study diets but this study suggests that VLCD’s may be possible in T2DM without worsening cardiovascular risk. Some of these factors are present in the “paleolithic diet”, which is discussed later.
Lower carbohydrate, higher protein diets
The acceptability and feasibility of maintaining a very low carbohydrate diet and the underlying concern about the high consumption of saturated fat have drawn many researchers to focus on increasing protein in the diet, with a reciprocal reduction in carbohydrate, while maintaining fat at a relatively low level.
Weight loss
Adopting a diet moderately low in carbohydrate (35%–45% of energy), moderately high in protein (25%–35% of energy), and maintaining fat at 30% of energy in overweight and obese adults produces an initial greater weight loss compared to a high carbohydrate diet,46,47 which is not sustained in the long-term48 and has not been demonstrated in T2DM.49–52 It has been observed that a greater number of people are able to achieve weight loss of more than 10% of body weight48 with diets moderately low in carbohydrate (eg, the South Beach diet) and during weight maintenance after weight loss these diets are more acceptable.52,53 These studies suggest that maintenance of a reduction in energy intake remains the most critical factor in inducing weight loss but lower carbohydrate, higher protein diets may confer some advantage in improving compliance in the long-term.
Glycemic control
Glucose and insulin curves are significantly lower after a high protein, low carbohydrate meal than after a carbohydrate-rich meal, which is sustained over a 24-hour period in a highly controlled setting.54 In a short-term intervention study in eight men with T2DM, a diet high in protein (30% protein, 20% carbohydrate, 50% fat) compared to a control diet (15% protein, 55% carbohydrate, 30% fat) produced a significant reduction in mean 24 hours serum glucose and glycosylated hemoglobin.38 As all three macronutrients differed between diet groups, interpretation of these data is difficult. Improvement in glycemic control has not been demonstrated in other short-term studies55 or after 1 year.42 In the Diabetes Excess Weight Loss (DEWL) randomized controlled trial, there was no difference in glycemic control in subjects with T2DM over 2 years when the dietary intervention was implemented in a manner similar to standard clinical practice.51 Initial changes in intake as prescribed returned to habitual consumption over time. Therefore, whilst experimental investigations suggest a benefit of lowering carbohydrate on glucose homeostasis, sustained improvements in glycemic control require a dietary change that is acceptable and able to be maintained in the long-term.
Cardiovascular disease risk
There are no dietary intervention studies which have reported on long-term cardiovascular outcomes such as myocardial infarction or stroke. Therefore, we are limited to evidence on the effects on cardiovascular disease risk factors. Consistent reductions in triacylglycerols have been observed in low carbohydrate diets during short interventions.46,53,56 Triacylglycerols are associated with cardiovascular events and the promotion of atherosclerosis; therefore, the reduction in levels observed in high protein diets may have positive long-term effects on cardiovascular disease.57,58 Improvements in LDL cholesterol have not been seen in similar studies56 or in T2DM.59,60 However, beneficial effects on HDL may occur when higher proportions of protein and fat are derived from plant-based sources.59
Blood pressure is intrinsically related to weight loss and specific beneficial effects of lowering carbohydrate in T2DM have not been consistently reported in long-term studies.51,52,59 Two 8-week studies with low carbohydrate diets, including people with T2DM, demonstrated a 5–10 mmHg reduction in systolic blood pressure compared to control diets, suggesting that in a more controlled setting, lowering carbohydrate may confer some advantages on blood pressure, which are difficult to translate in the long-term.55,61
Adiposity, particularly intra-abdominal adiposity, is associated with an increased risk of cardiovascular disease and is essential to the diagnosis of the metabolic syndrome.62 Altering the ratio of lean-to-adipose tissue during weight loss or weight maintenance may therefore have long-term health benefits. An improvement in body composition, by reducing the proportion of adipose mass and/or muscle sparing, has been shown in human studies with lower carbohydrate and additional dietary protein in energy restricted diets63,64 during ad libitum eating47,48,52,65 and is seen in habitual consumers of high protein diets.66
Low carbohydrate paleolithic- type diets
Paleolithic-type diets, comprising lean meat, fish, fruit, vegetables, root vegetables, eggs, and nuts, have recently increased in popularity, stimulated in part by popular press and the portrayal that these diets will improve health and vitality and promote weight loss. The concept is based on the hypothesis that in evolutionary terms our deviation from a hunter-gatherer diet has occurred too rapidly for adequate genetic adaptation, and that the resulting mismatch helps to cause some common chronic diseases.67–69 The exact composition of the paleolithic diet has been the subject of much research and therefore the manner that it has been adopted into popular diets has varied. When Konner and Eaton reflected on their initial presentation of the diet, they argued that based on archaeological and paleontological evidence they had overestimated some proportions of macronutrients in the diet and underestimated others.67,68 Notably, they concluded that the paleolithic diet was low in fat, particularly saturated fat, was higher in protein, particularly marine protein as opposed to wild animals, had very low energy density, and substantially higher fiber. The proportion of carbohydrate in the diet varied by location and accessibility to grains but overall the carbohydrate source was predominantly fruit and vegetables, some honey, and no added sugars or refined carbohydrate. Alluded to in these articles is the considerable amount of physical activity that hunter-gatherer populations performed compared to modern day levels, and its potential for independently improving health outcomes, which has rarely been factored into overall consideration of this diet.
Short to longer term, weeks to 2-year intervention studies have demonstrated beneficial effects on blood pressure, cholesterol, waist circumference, and satiety.70,71 A randomized controlled trial in 29 patients with ischemic heart disease and glucose intolerance or T2DM demonstrated improved glucose tolerance in a paleolithic diet compared to a Mediterranean diet.72 To identify the mechanistic basis of paleolithic diets, Bligh et al investigated the effects of a paleolithic meal and a World Health Organization reference meal in a crossover design on blood glucose control, gut hormone response, and appetite regulation in healthy subjects.73 Over 180 minutes, satiety scores were higher in the paleolithic diet, as were glucagon-like peptide 1 and peptide YY concentrations independent of energy or protein content of the meal. In contrast, glucose and insulin curves did not differ between the diets.73
It is certainly conceivable that a diet based on less processed, fresh food may have considerable benefits, depending perhaps on the way that the diet is interpreted. The observed effects on satiety may lead to changes in total daily energy intake and ultimately in weight loss, possibly mediated through gut hormones. With potential benefits on other cardiovascular risk factors, adopting a paleolithic-type diet may be a useful alternative for people with diabetes; however, further research is required in this area before these health claims can be clearly attributable to features of a paleolithic diet.
Dietary sugar
There has been growing interest in the impact of refined carbohydrate and sugar specifically. The intake of sugar has been steadily increasing globally with epidemiological evidence linking this with obesity and T2DM. Consequently, the World Health Organization reviewed its advice on dietary free sugar intake in 2014, and concluded that it would continue its recommendation of less than 10% of total energy considering this a strong recommendation to prevent obesity and tooth decay.74 However, it did add a second recommendation that a free sugar intake of 5% (25 g/day for an adult) was associated with additional health benefits. Free sugars include “all monosaccharides and disaccharides added to foods and beverages by the manufacturer, cook or consumer, and sugars naturally present in honey, syrups, fruit juices and fruit juice concentrates”.74 There have been several recent reviews concluding that sugar is positively associated with body weight, and increasing sugar consumption resulted in a weight gain of ~0.75 kg in a meta-analysis.75–77 High sugar intake has also been associated with higher blood pressure (mean difference 6.9 mmHg [95% confidence interval (CI): 3.4, 10.3 mmHg; P<0.001 compared with low sugar intake] for systolic blood pressure and 5.6 mmHg [95% CI: 2.5, 8.8 mmHg; P=0.0005] for diastolic blood pressure).78 The other notable effect of a high sugar intake is on triglycerides (mean difference: 0.11 mmol/L; 95% CI: 0.07, 0.15 mmol/L; P<0.0001) and LDL cholesterol (0.12 mmol/L; 95% CI: 0.05, 0.19 mmol/L; P=0.0001) when compared with a low sugar intake.78
There is also evidence that sugar intake directly influences development of T2DM. In women consuming one or more sugar-sweetened beverages per day, the diabetes relative risk was 1.83 when compared with those who had one drink per month.79 Similarly, in African-American women, the incidence rate ratio for two or more soft drinks per day was 1.24 (95% CI: 1.06–1.45). For fruit drinks, the incidence rate ratio was 1.31 (95% CI: 1.13–1.52). The association of diabetes with soft drink consumption was strongly mediated by BMI, whereas the association with fruit drink consumption was independent.80 In men, the hazard ratio was 1.24 (95% CI: 1.09, 1.40; P<0.01) for those in the top quartile of intake.81 While the World Health Organization recommendation only specifically addresses obesity, restricting free sugars to less than 10% of total energy intake is likely to prevent diabetes for a portion of the at-risk population. Reducing dietary carbohydrate is likely to have the added effect of reducing free sugars, which will benefit weight, cardiovascular risk, and glucose metabolism.
Type 1 diabetes
Low carbohydrate diets in the management of type 1 diabetes
Low carbohydrate diets were once the conventional treatment for type 1 diabetes, but with the increasing availability of human insulin, and new research around risk factors for heart disease, low carbohydrate diets were replaced in the early 1980s with higher carbohydrate/higher fiber patterns of eating. Some people with type 1 diabetes however continued to do well on a low carbohydrate diet, even when compared with a high carbohydrate/high fiber diet.82,83
While low carbohydrate diets have received a lot of attention recently in T2DM, there have only been two studies recently considering this type of diet in type 1 diabetes. One was an audit of a diabetes service education class on low carbohydrate eating. It then followed 48 patients who self-reported to have chosen to follow a low carbohydrate diet. Mean HbA1c dropped from 7.7% to 6.4% after 3 months and stayed at this level for 4 years.84,85 The second was a small study comparing a low carbohydrate diet with carbohydrate counting. The low carbohydrate group had significant reductions in HbA1c (63 to 55 mmol/mol [8.9% to 8.2%], P<0.05) and daily insulin use (64.4 to 44.2 units/day, P<0.05).86
The gold standard for type 1 diabetes care worldwide has moved to flexible intensive insulin therapy (“FIIT”), developed in the 1970s and delivered through large scale education programs such as Dose Adjustment For Normal Eating (DAFNE).87 The cornerstone of this approach is carbohydrate counting, giving people the skills to match insulin boluses with desired carbohydrate intake. When done well, this can give a large amount of freedom – to have no carbohydrate at one meal and then 60 g at the next, the freedom any person without diabetes enjoys. For those who find carbohydrate counting too difficult, there is still the option of “pattern adjusting” where relatively fixed stable amounts of carbohydrate are consumed at each meal with a set dose of insulin, and the type of carbohydrate can be exchanged within quantity limits. Research has shown that carbohydrate counting is effective for people with type 1 diabetes88 and that people can be taught to estimate carbohydrate reasonably accurately.89,90
In a recent qualitative review of participants who had undergone the DAFNE course, it was revealed that flexible insulin therapy had led some patients to severely restrict carbohydrate as they found that large amounts of carbohydrate coupled with large insulin doses led to unpredictable blood glucose results.91 Many of the participants reported finding FIIT to be very difficult in practice due to the challenge of estimating the carbohydrate contents of different foods. This led them to limit their intake to a diet that they could control, thus not utilizing the potential freedom FIIT could give them. This real world experience highlights the need to continue to find alternatives so that people with type 1 diabetes have choice over their treatment. If some individuals are naturally tending toward a low carbohydrate diet despite such tools as FIIT, studies must be conducted to assess the effect of this.
Practically, a low carbohydrate diet for people with type 1 diabetes could be relatively easy to follow for those who are already carbohydrate “counting”; however, the transition may require intensive monitoring with a diabetes health professional to ensure insulin adjustments are accurate. People may also find they must give an insulin bolus for protein intake, as gluconeogenesis from protein occurs in the absence of carbohydrate. The starting point for this has been suggested as half that of the insulin to carbohydrate ratio, for example, if the insulin to carbohydrate ratio is 1 unit for 10 g, then the insulin to protein ratio would be 1 unit per 20 g.92
Ketosis, or the use of ketone bodies for energy instead of glucose, usually occurs when consuming less than 52 g carbohydrate per day, in a VLCD.93 This could then be a risk factor for ketoacidosis in people with type 1 diabetes, when inadequate insulin is supplied and ketones accumulate to a dangerous level. However, there is no evidence that ketoacidosis would occur given the usual amounts of insulin. Consuming between 75 and 130 g of carbohydrate per day, as the definition of a low carbohydrate diet, means ketosis is unlikely and therefore any risk of ketoacidosis is minimal. This is further reinforced by ensuring the correct amount of insulin is given, hence the reason why working with a diabetes health care team is paramount.
Macronutrient quality
To identify beneficial effects for T2DM of diets based on macronutrient manipulation requires consistent evidence derived from well-designed studies. The difficulty with obtaining this evidence is that the composition of the diets used varies in quality and proportion of carbohydrate, protein, and fat.94 For example, high carbohydrate diets in T2DM initially showed significant benefits on glucose metabolism and lipid profiles contrary to the data reported above.95 However, the focus of the high carbohydrate diet was a high fiber intake, which has not been consistently repeated in later studies. The acute effect of dietary fiber is seen in combination with a low glycemic index meal in a recent study in people with T2DM where improvements in postprandial glucose and insulin responses were most prominent in the meals high in fiber and low in glycemic index.94
In a similar manner to carbohydrates, protein-type appears to influence lipids and glucose metabolism in differing ways.96 Meat protein is associated with weight gain and an increased risk of heart disease. In the Nurses Health study, animal low carbohydrate diets were associated with a 23% increase in all cause mortality while a vegetable low carbohydrate diet was associated with a 20% reduction in all cause mortality and cardiovascular mortality.97
Current recommendations
As discussed, recommendations for a healthy diet in diabetes have followed the high carbohydrate, low fat approach since the first association of saturated fat and cardiovascular disease. In keeping with the substantial body of evidence that a variety of different diets may produce beneficial effects on weight loss and cardiovascular risk, these recommendations are changing. It is becoming more apparent that the most important features of a dietary approach in diabetes is a diet which can be followed in the long-term with sustained effects on weight, glucose control, and cardiovascular risk factors.98 Additionally, consideration must be given to the economic sustainability of any dietary recommendations. Reducing carbohydrate intake with reciprocal increases in protein, particularly animal protein, may have significant implications on farming practices, environmental consequences of ongoing deforestation required for farmland, and increased greenhouse gas production. Additionally, higher protein diets tend to be more costly for the individual and, given the high prevalence of diabetes in low socioeconomic areas, are unlikely to be a feasible option for the wider diabetes population.
Dietary recommendations from both the American Diabetes Association99 (Figure 1) and Diabetes UK100 (Figure 2) have become much less prescriptive in macronutrient composition, recognizing that a number of different dietary approaches may be beneficial. There is unquestionably an importance in considering dietary carbohydrate, but whether this is to promote high quality, low glycemic index, high fiber carbohydrate, consistent daily carbohydrate intake for ease of management or to replace some carbohydrate with protein is more open to individual choice.
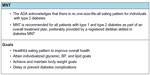  | Figure 1 ADA dietary recommendations. |
  | Figure 2 Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. |
Conclusion
Due to the complex nature of eating behavior and the reciprocal nature of macronutrient proportion in an isoenergetic diet, defining the optimal diet for T2DM is extremely difficult. Decades of research into the impact of various macronutrient manipulation have finally concluded that a variety of dietary approaches produce similarly beneficial effects on weight, glycemic control, and cardiovascular risk dependent on the ability to maintain a diet in the long-term. There are some specific dietary elements that confer increased health risk such as saturated fat and sugar, with some beneficial elements such as fiber and mono and polyunsaturated fat. It is probable that there are genetic or ethnic determinants which favor one diet over another. This gene–environment interaction is an important area for further research with the possibility of being able to personalize and optimize dietary management in diabetes.
Disclosure
The authors report no conflicts of interest in this work.
References
Ministry of Health. A Portrait of Health. Key results of the 2006/07 New Zealand Health Survey. Wellington: Ministry of Health; 2008. | |
Acheson KJ. Diets for body weight control and health: the potential of changing the macronutrient composition. Eur J Clin Nutr. 2013; 67(5):462–466. | |
Kritchevsky D. History of recommendations to the public about dietary fat. J Nutr. 1998;128(2 Suppl):449S–452S. | |
Page IH, Stare FJ, Corcoran AC, Pollack H, Wilkinson CF Jr. Atherosclerosis and the fat content of the diet. J Am Med Assoc. 1957; 164(18):2048–2051. | |
Hockaday TD, Hockaday JM, Mann JI, Turner RC. Prospective comparison of modified fat-high-carbohydrate with standard low-carbohydrate dietary advice in the treatment of diabetes: one year follow-up study. Br J Nutr. 1978;39(2):357–362. | |
Simpson HC, Simpson RW, Lousley S, et al. A high carbohydrate leguminous fibre diet improves all aspects of diabetic control. Lancet. 1981;1(8210):1–5. | |
Simpson RW, Mann JI, Eaton J, Moore RA, Carter R, Hockaday TD. Improved glucose control in maturity-onset diabetes treated with high-carbohydrate-modified fat diet. Br Med J. 1979;1(6180):1753–1756. | |
Murphy SP, Johnson RK. The scientific basis of recent US guidance on sugars intake. Am J Clin Nutr. 2003;78(4):827S–833S. | |
Gross LS, Li L, Ford ES, Liu S. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecologic assessment. Am J Clin Nutr. 2004;79(5):774–779. | |
Livingstone MB, Black AE. Markers of the validity of reported energy intake. J Nutr. 2003;133 (Suppl 3):895S–920S. | |
Rennie KL, Jebb SA, Wright A, Coward WA. Secular trends in under-reporting in young people. Br J Nutr. 2005;93(2):241–247. | |
Newby PK, Weismayer C, Akesson A, Tucker KL, Wolk A. Longitudinal changes in food patterns predict changes in weight and body mass index and the effects are greatest in obese women. J Nutr. 2006;136(10):2580–2587. | |
Johnson L, Mander AP, Jones LR, Emmett PM, Jebb SA. Energy-dense, low-fiber, high-fat dietary pattern is associated with increased fatness in childhood. Am J Clin Nutr. 2008;87(4):846–854. | |
Huo R, Du T, Xu Y, et al. Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: a meta-analysis. Eur J Clin Nutr. 2014. Epub 2014 Nov 6. | |
Brinkworth GD, Noakes M, Keogh JB, Luscombe ND, Wittert GA, Clifton PM. Long-term effects of a high-protein, low-carbohydrate diet on weight control and cardiovascular risk markers in obese hyperinsulinemic subjects. Int J Obes Relat Metab Disord. 2004;28(5):661–670. | |
Stubbs RJ, Harbron CG, Murgatroyd PR, Prentice AM. Covert manipulation of dietary fat and energy density: effect on substrate flux and food intake in men eating ad libitum. Am J Clin Nutr. 1995;62(2):316–329. | |
Jebb SA, Prentice AM, Goldberg GR, Murgatroyd PR, Black AE, Coward WA. Changes in macronutrient balance during over- and underfeeding assessed by 12-d continuous whole-body calorimetry. Am J Clin Nutr. 1996;64(3):259–266. | |
Flatt JP, Ravussin E, Acheson KJ, Jéquier E. Effects of dietary fat on postprandial substrate oxidation and on carbohydrate and fat balances. J Clin Invest. 1985;76(3):1019–1024. | |
Shetty PS, Prentice AM, Goldberg GR, et al. Alterations in fuel selection and voluntary food intake in response to isoenergetic manipulation of glycogen stores in humans. Am J Clin Nutr. 1994;60(4):534–543. | |
Cottrell RR. Weight Control. Guilford, CT: Dushkin Publishing Group; 1992. | |
Vander Wal JS, Marth JM, Khosla P, Jen KL, Dhurandhar NV. Short-term effect of eggs on satiety in overweight and obese subjects. J Am Coll Nutr. 2005;24(6):510–515. | |
Latner JD, Schwartz M. The effects of a high-carbohydrate, high-protein or balanced lunch upon later food intake and hunger ratings. Appetite. 1999;33(1):119–128. | |
Barkeling B, Rossner S, Bjorvell H. Effects of a high-protein meal (meat) and a high-carbohydrate meal (vegetarian) on satiety measured by automated computerized monitoring of subsequent food intake, motivation to eat and food preferences. Int J Obes. 1990;14(9):743–751. | |
Poppitt SD, McCormack D, Buffenstein R. Short-term effects of macronutrient preloads on appetite and energy intake in lean women. Physiol Behav. 1998;64(3):279–285. | |
Porrini M, Santangelo A, Crovetti R, Riso P, Testolin G, Blundell JE. Weight, protein, fat, and timing of preloads affect food intake. Physiol Behav. 1997;62(3):563–570. | |
Rolls BJ, Hetherington M, Burley VJ. The specificity of satiety: the influence of foods of different macronutrient content on the development of satiety. Physiol Behav. 1988;43(2):145–153. | |
Johnson J, Vickers Z. Effects of flavor and macronutrient composition of food servings on liking, hunger and subsequent intake. Appetite. 1993;21(1):25–39. | |
Gogebakan O, Kohl A, Osterhoff MA, et al. Effects of weight loss and long-term weight maintenance with diets varying in protein and glycemic index on cardiovascular risk factors: the diet, obesity, and genes (DiOGenes) study: a randomized, controlled trial. Circulation. 2011;124(25):2829–2838. | |
Atkins R. Dr Atkins’ New Diet Revolution. Rev. ed. New York: Avon Books; 1998. | |
Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med. 2003;348(21):2082–2090. | |
Samaha FF, Iqbal N, Seshadri P, et al. A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med. 2003; 348(21):2074–2081. | |
Stern L, Iqbal N, Seshadri P, et al. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med. 2004;140(10):778–785. | |
Hussain TA, Mathew TC, Dashti AA, Asfar S, Al-Zaid N, Dashti HM. Effect of low-calorie versus low-carbohydrate ketogenic diet in type 2 diabetes. Nutrition. 2012;28(10):1016–1021. | |
Krebs JD, Bell DA, Hall R, et al. Improvements in glucose metabolism and insulin sensitivity with a low-carbohydrate diet in obese patients with type 2 diabetes. J Am Coll Nutr. 2013;32(1):11–17. | |
Boden G, Sargrad K, Homko C, Mozzoli M, Stein TP. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Intern Med. 2005;142(6):403–411. | |
Hession M, Rolland C, Kulkarni U, Wise A, Broom J. Systematic review of randomized controlled trials of low-carbohydrate vs low-fat/low-calorie diets in the management of obesity and its comorbidities. Obes Rev. 2009;10(1):36–50. | |
Castaneda-Gonzalez LM, Bacardi Gascon M, Jimenez Cruz A. Effects of low carbohydrate diets on weight and glycemic control among type 2 diabetes individuals: a systemic review of RCT greater than 12 weeks. Nutr Hosp. 2011;26(6):1270–1276. | |
Gannon MC, Nuttall FQ. Effect of a high-protein, low-carbohydrate diet on blood glucose control in people with type 2 diabetes. Diabetes. 2004;53(9):2375–2382. | |
Nuttall FQ, Gannon MC. The metabolic response to a high-protein, low-carbohydrate diet in men with type 2 diabetes mellitus. Metab Clin Exp. 2006;55(2):243–251. | |
Nuttall FQ, Schweim K, Hoover H, Gannon MC. Effect of the LoBAG30 diet on blood glucose control in people with type 2 diabetes. Br J Nutr. 2008;99(3):511–519. | |
Westman EC, Yancy WS Jr, Mavropoulos JC, Marquart M, McDuffie JR. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab (Lond). 2008;5:36. | |
Davis NJ, Tomuta N, Schechter C, et al. Comparative study of the effects of a 1-year dietary intervention of a low-carbohydrate diet versus a low-fat diet on weight and glycemic control in type 2 diabetes. Diabetes Care. 2009;32(7):1147–1152. | |
Shai I, Schwarzfuchs D, Henkin Y, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008; 359(3):229–241. | |
Tay J, Luscombe-Marsh ND, Thompson CH, et al. A very low-carbohydrate, low-saturated fat diet for type 2 diabetes management: a randomized trial. Diabetes Care. 2014;37(11):2909–2918. | |
Tay J, Luscombe-Marsh ND, Thompson CH, et al. Comparison of low- and high-carbohydrate diets for type 2 diabetes management: a randomized trial. Am J Clin Nutr. 2015;102(4):780–790. | |
Skov AR, Toubro S, Ronn B, Holm L, Astrup A. Randomized trial on protein vs carbohydrate in ad libitum fat reduced diet for the treatment of obesity. Int J Obes Relat Metab Disord. 1999;23(5):528–536. | |
Weigle DS, Breen PA, Matthys CC, et al. A high-protein diet induces sustained reductions in appetite, ad libitum caloric intake, and body weight despite compensatory changes in diurnal plasma leptin and ghrelin concentrations. Am J Clin Nutr. 2005;82(1):41–48. | |
Due A, Toubro S, Skov AR, Astrup A. Effect of normal-fat diets, either medium or high in protein, on body weight in overweight subjects: a randomised 1-year trial. Int J Obes Relat Metab Disord. 2004; 28(10):1283–1290. | |
Luscombe ND, Clifton PM, Noakes M, Parker B, Wittert G. Effects of energy-restricted diets containing increased protein on weight loss, resting energy expenditure, and the thermic effect of feeding in type 2 diabetes. Diabetes Care. 2002;25(4):652–657. | |
Brinkworth GD, Noakes M, Parker B, Foster P, Clifton PM. Long-term effects of advice to consume a high-protein, low-fat diet, rather than a conventional weight-loss diet, in obese adults with type 2 diabetes: one-year follow-up of a randomised trial. Diabetologia. 2004;47(10):1677–1686. | |
Krebs JD, Elley CR, Parry-Strong A, et al. The Diabetes Excess Weight Loss (DEWL) Trial: a randomised controlled trial of high-protein versus high-carbohydrate diets over 2 years in type 2 diabetes. Diabetologia. 2012;55(4):905–914. | |
Larsen RN, Mann NJ, Maclean E, Shaw JE. The effect of high-protein, low-carbohydrate diets in the treatment of type 2 diabetes: a 12 month randomised controlled trial. Diabetologia. 2011;54:731–740. | |
Layman DK, Evans EM, Erickson D, et al. A moderate-protein diet produces sustained weight loss and long-term changes in body composition and blood lipids in obese adults. J Nutr. 2009;139(3):514–521. | |
Raben A, Agerholm-Larsen L, Flint A, Holst JJ, Astrup A. Meals with similar energy densities but rich in protein, fat, carbohydrate, or alcohol have different effects on energy expenditure and substrate metabolism but not on appetite and energy intake. Am J Clin Nutr. 2003;77(1):91–100. | |
Sargrad KR, Homko C, Mozzoli M, Boden G. Effect of high protein vs high carbohydrate intake on insulin sensitivity, body weight, hemoglobin A1c, and blood pressure in patients with type 2 diabetes mellitus. J Am Diet Assoc. 2005;105(4):573–580. | |
Noakes M, Keogh JB, Foster PR, Clifton PM. Effect of an energy-restricted, high-protein, low-fat diet relative to a conventional high-carbohydrate, low-fat diet on weight loss, body composition, nutritional status, and markers of cardiovascular health in obese women. Am J Clin Nutr. 2005;81(6):1298–1306. | |
Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM. Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA. 2007;298(3):309–316. | |
Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA. 2007;298(3):299–308. | |
Evangelista LS, Heber D, Li Z, Bowerman S, Hamilton MA, Fonarow GC. Reduced body weight and adiposity with a high-protein diet improves functional status, lipid profiles, glycemic control, and quality of life in patients with heart failure: a feasibility study. J Cardiovasc Nurs. 2009;24(3):207–215. | |
Gannon MC, Nuttall FQ, Saeed A, Jordan K, Hoover H. An increase in dietary protein improves the blood glucose response in persons with type 2 diabetes. Am J Clin Nutr. 2003;78(4):734–741. | |
Hodgson JM, Burke V, Beilin LJ, Puddey IB. Partial substitution of carbohydrate intake with protein intake from lean red meat lowers blood pressure in hypertensive persons. Am J Clin Nutr. 2006;83(4):780–787. | |
Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365(9468):1415–1428. | |
Layman DK, Boileau RA, Erickson DJ, et al. A reduced ratio of dietary carbohydrate to protein improves body composition and blood lipid profiles during weight loss in adult women. J Nutr. 2003; 133(2):411–417. | |
Layman DK, Evans E, Baum JI, Seyler J, Erickson DJ, Boileau RA. Dietary protein and exercise have additive effects on body composition during weight loss in adult women. J Nutr. 2005;135(8):1903–1910. | |
Westerterp-Plantenga MS, Lejeune MP, Nijs I, van Ooijen M, Kovacs EM. High protein intake sustains weight maintenance after body weight loss in humans. Int J Obes Relat Metab Disord. 2004;28(1):57–64. | |
Merchant AT, Anand SS, Vuksan V, et al. Protein intake is inversely associated with abdominal obesity in a multi-ethnic population. J Nutr. 2005;135(5):1196–1201. | |
Eaton SB, Konner M. Paleolithic nutrition. A consideration of its nature and current implications. N Engl J Med. 1985;312(5):283–289. | |
Konner M, Eaton SB. Paleolithic nutrition: twenty-five years later. Nutr Clin Pract. 2010;25(6):594–602. | |
Cordain L, Eaton SB, Sebastian A, et al. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. 2005;81(2):341–354. | |
Boers I, Muskiet FA, Berkelaar E, et al. Favourable effects of consuming a Palaeolithic-type diet on characteristics of the metabolic syndrome: a randomized controlled pilot-study. Lipids Health Dis. 2014;13:160. | |
Mellberg C, Sandberg S, Ryberg M, et al. Long-term effects of a Palaeolithic-type diet in obese postmenopausal women: a 2-year randomized trial. Eur J Clin Nutr. 2014;68(3):350–357. | |
Lindeberg S, Jonsson T, Granfeldt Y, et al. A Palaeolithic diet improves glucose tolerance more than a Mediterranean-like diet in individuals with ischaemic heart disease. Diabetologia. 2007;50(9):1795–1807. | |
Bligh HF, Godsland IF, Frost G, et al. Plant-rich mixed meals based on Palaeolithic diet principles have a dramatic impact on incretin, peptide YY and satiety response, but show little effect on glucose and insulin homeostasis: an acute-effects randomised study. Br J Nutr. 2015; 113(4):574–584. | |
World Health Organisation. Guideline – Sugars Intake for Adults and Children. Geneva: World Health Organisation; 2015. | |
Bray GA, Popkin BM. Dietary sugar and body weight: have we reached a crisis in the epidemic of obesity and diabetes?: Health be damned! Pour on the sugar. Diabetes Care. 2014;37(4):950–956. | |
Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev. 2013;14(8):606–619. | |
Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2013;346:e7492. | |
Te Morenga LA, Howatson AJ, Jones RM, Mann J. Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. Am J Clin Nutr. 2014;100(1):65–79. | |
Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA. 2004;292(8):927–934. | |
Palmer JR, Boggs DA, Krishnan S, Hu FB, Singer M, Rosenberg L. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch Intern Med. 2008; 168(14):1487–1492. | |
de Koning L, Malik VS, Rimm EB, Willett WC, Hu FB. Sugar-sweetened and artificially sweetened beverage consumption and risk of type 2 diabetes in men. Am J Clin Nutr. 2011;93(6):1321–1327. | |
McCulloch DK, Mitchell RD, Ambler J, Tattersall RB. A prospective comparison of ‘conventional’ and high carbohydrate/high fibre/low fat diets in adults with established type 1 (insulin-dependent) diabetes. Diabetologia. 1985;28(4):208–212. | |
Bernstein RK. Virtually continuous euglycemia for 5 yr in a labile juvenile-onset diabetic patient under noninvasive closed-loop control. Diabetes Care. 1980;3(1):140–143. | |
Nielsen JV, Gando C, Joensson E, Paulsson C. Low carbohydrate diet in type 1 diabetes, long-term improvement and adherence: a clinical audit. Diabetol Metab Syndr. 2012;4(1):23. | |
Nielsen JV, Jonsson E, Ivarsson A. A low carbohydrate diet in type 1 diabetes: clinical experience – a brief report. Ups J Med Sci. 2005; 110(3):267–273. | |
Krebs JD, Parry-Strong A, Cresswell P, Reynolds AN, Hanna A, Haeusler S. A randomised trial of the feasibility of a low carbohydrate diet vs standard carbohydrate counting in adults with type 1 diabetes taking body weight into account. Asia Pac J Clin Nutr. 2016;25(1):78–84. | |
The DAFNE Study Group; Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ. 2002;325(7367):746. | |
Goksen D, Atik Altinok Y, Ozen S, Demir G, Darcan S. Effects of carbohydrate counting method on metabolic control in children with type 1 diabetes mellitus. J Clin Res Pediatr Endocrinol. 2014;6(2):74–78. | |
Smart CE, Ross K, Edge JA, King BR, McElduff P, Collins CE. Can children with Type 1 diabetes and their caregivers estimate the carbohydrate content of meals and snacks? Diabet Med. 2010; 27(3):348–353. | |
Spiegel G, Bortsov A, Bishop FK, et al. Randomized nutrition education intervention to improve carbohydrate counting in adolescents with type 1 diabetes study: is more intensive education needed? J Acad Nutr Diet. 2012;112(11):1736–1746. | |
Lawton J, Rankin D, Cooke DD, et al. Dose Adjustment for Normal Eating: a qualitative longitudinal exploration of the food and eating practices of type 1 diabetes patients converted to flexible intensive insulin therapy in the UK. Diabetes Res Clin Pract. 2011;91(1):87–93. | |
Bernstein RK. The Diabetes Diet. New York: Little, Brown and Company; 2005. | |
Gibson AA, Seimon RV, Lee CM, et al. Do ketogenic diets really suppress appetite? A systematic review and meta-analysis. Obes Rev. 2015;16(1):64–76. | |
Silva FM, Kramer CK, Crispim D, Azevedo MJ. A high-glycemic index, low-fiber breakfast affects the postprandial plasma glucose, insulin, and ghrelin responses of patients with type 2 diabetes in a randomized clinical trial. J Nutr. 2015;145(4):736–741. | |
Lousley SE, Jones DB, Slaughter P, Carter RD, Jelfs R, Mann JI. High carbohydrate-high fibre diets in poorly controlled diabetes. Diabet Med. 1984;1(1):21–25. | |
Clifton PM. Protein and coronary heart disease: the role of different protein sources. Curr Atheroscler Rep. 2011;13(6):493–498. | |
Fung TT, van Dam RM, Hankinson SE, Stampfer M, Willett WC, Hu FB. Low-carbohydrate diets and all-cause and cause-specific mortality: two cohort studies. Ann Intern Med. 2010;153(5):289–298. | |
Krebs JD, Parry-Strong A. Is there an optimal diet for patients with type 2 diabetes? Yes, the one that works for them! Br J Diabet Vasc Dis. 2013;13(2):60–66. | |
American Diabetes Association Resources for Health Professionals. 2015 [cited June 30, 2015]. Available from: http://professional.diabetes.org/resourcesforprofessionals.aspx?cid=84160. | |
Diabetes UK Evidence-Based Nutrition Guidelines. 2011 [cited June 30, 2015]. Available from: https://www.diabetes.org.uk/nutrition-guidelines. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
