Back to Journals » Risk Management and Healthcare Policy » Volume 16
Impacts of Outpatient Payment Reforms on Volume and Expenditures in Public Hospitals: Evidence from a Quasi-Experimental Analysis in Zhejiang, China
Authors Zhang T, Lu B, Song Y, Chen M
Received 6 December 2022
Accepted for publication 6 March 2023
Published 16 March 2023 Volume 2023:16 Pages 415—424
DOI https://doi.org/10.2147/RMHP.S400385
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jongwha Chang
Tao Zhang,1 Beiyin Lu,1 Yang Song,2 Minyan Chen3
1Department of Health Policy and Management, School of Public Health, Hangzhou Normal University, Hangzhou, People’s Republic of China; 2Department of Health Information Management, School of Medicine and Health Management, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 3Medical Insurance Department, Hangzhou Ninth People’s Hospital, Hangzhou, People’s Republic of China
Correspondence: Yang Song; Minyan Chen, Email [email protected]; [email protected]
Purpose: China developed an innovative episode-based payment scheme for outpatient care, namely “Ambulatory Patient Groups (APGs) + capitation” payment, to constrain inflation in outpatient expenditures. This study aimed to assess the effects of this payment method on volume and expenditures in Chinese public hospitals.
Methods: A quasi-experimental study was conducted with 7 municipal and 12 county hospitals from Jinhua as the intervention group and 15 municipal and 24 county hospitals from three neighbouring cities as the control group. The payment reform was introduced to municipal and county hospitals in the intervention group in January 2020 and January 2021, respectively. Monthly data on volumes and outpatient expenditures were collected from each hospital from January 2019 to December 2021. Controlled interrupted time-series analyses were performed to determine the effects of the funding reforms.
Results: Outpatient visits in municipal hospitals decreased by 1417.54 (p=0.048) per month on average compared with control ones after the reform was implemented, whilst that in county hospitals increased by 1058.04 (p=0.041) per month on average. The trend of drug expenditures (β7=− 1.41, p=0.019) in municipal hospitals dropped, which was accompanied by an immediate reduction in consumable expenditures (β6 =− 6.89, p=0.044). The funding reform also led to the significant declines in drug (β6=− 10.96, p=0.009) and consumable (β6=− 4.78, p=0.041) expenditures in county hospitals. Municipal hospitals experienced the drop in the trend of total outpatient expenditures (β7=− 3.99, p=0.018) over the same period.
Conclusion: The strength of the “AGPs + capitation” payment for outpatient care lies in its ability to control the excessive growth of medical expenses through correcting inappropriate incentives. However, minimising potential cost-shifting and risk-shifting to uninsured service items should be given attention.
Keywords: Ambulatory Patient Groups, capitation, public hospital, outpatient care, China
Introduction
Designing appropriate payment schemes has been the top priority in the health system reforms in developing and developed countries. China is no exception. Over the past decade, healthcare expenditures in China have increased by more than 200%, and they are growing at a rate of more than 10% per year.1 Fee-for-service (FFS) should take important responsibility. In FFS arrangements, providers charge payers based on the volume of services or intensity of resources used for providing healthcare. Providers have every incentive to offer more services. As a result, FFS payments led to soaring healthcare costs, unnecessary healthcare provision and production inefficiencies.2 Changing FFS to the new payment system is attracting an increasing attention.
In 2019, the National Medical Insurance Administration selected 30 cities in China to pilot diagnosis-related groups (DRGs) payment, and it plans to roll out this case-based payment nationwide.3 The DRGs-payment pilot in China has shown its potential to reduce health expenditures and out-of-pocket (OOP) costs in inpatient setting.4,5 However, unintended consequences were also reported. For example, the cost-shifting from the inpatient to outpatient setting was found.6 For a long time, FFS for outpatient care has been adopted in China and no financial incentives have been provided to control utilisation of services in outpatient setting.6 Physicians had strong incentives to increase the volume of procedures and drug prescriptions. Data showed that outpatient expenditures per visit increased faster than that in the inpatient setting from 233.9 yuan in 2015 to 324.4 yuan in 2020 in China.7 After the DRGs system was adopted, shifting more inpatients to outpatient settings might accelerate this growth trend.
Jinhua, an economically developed city located in south-eastern China, designed a mixed payment scheme, namely, “Ambulatory Patient Groups (APGs) + capitation” payment, to address the aforementioned issues. Under this payment system, reimbursement for hospital outpatient costs is divided into two parts: 1) capitation prepayment for those signing a contract with hospitals and () APGs-based payment for those not signing a contract with hospitals.8 Figure 1 sketches the core design components of this new payment system. A detailed introduction is provided in the Institutional Background section. Obviously, financial incentives for providers have changed after this new case-based payment scheme has been introduced. Providers can gain surplus from reducing unnecessary practices in care provision and making the costs lower than the expected payment per case rather than overtreatments.
 |
Figure 1 Core components of “APGs + capitation” payment for outpatient care. |
Actually, APGs-based payment method has been used in western countries. For example, Medicare and Medicaid Services programmes replaced the prior cost-based system for reimbursing hospital outpatient services with APGs-based system under the Outpatient Prospective Payment System in 2000.9 Capitation-based reimbursement for primary care was also often introduced in the payment reforms of the UK, Australia, the Netherlands, Italy and Canada.10,11 In terms of the impacts of these payment schemes, some studies have provided considerable evidence, such as decreasing outpatients and expenditures.12,13 However, their effects on the Chinese healthcare system separating insurance reimbursements for outpatient and inpatient care remain unknown. The scheme taken in China also differs from the schemes taken elsewhere in that the payments for each APG group are determined by its average cost relative to average cost of all cases rather than setting the fixed payment level for each group.8 Another gap that needs to be filled is uncertain conclusions on the causation and lasting effects of payment reforms due to cross-sectional data used in prior studies.
By using monthly data points from public hospital in Jinhua, this study aims to investigate the effects of “APGs + capitation” payment scheme on service volume and care expenditures of municipal and county hospitals compared with neighbouring cities by employing an interrupted time series analysis (ITSA). Our study made the following contributions: 1) we provided the first empirical evidence on hospital response to this innovative payment for outpatient care in China; 2) ITSA with an independent control was used to estimate a more accurate longitudinal effects of payment reforms; and 3) our results yield important policy implications for establishing the value-based payment system for outpatient care in developing countries.
Institutional Background
In January 2020, Jinhua selected all municipal hospitals to employ the “APGs + capitation” reimbursement scheme for outpatient services. After a 1-year pilot, this new payment method was expanded to the county hospitals. The social health insurance programmes calculated regional global budget for outpatient care based on the outpatient expenditures over the previous year.8 Thereafter, this fixed funding budget is divided into two parts (Figure 1).
The first part is capitation-based prepayment for outpatients who sign a contract with the hospital. Funding was pre-packaged to the hospitals, and it covers total outpatient insurance payments for contracted patients. Unspent funds are kept by the hospital, but overspending was not subsidised by the insurance programmes. Specifically, the total of weights of contracted patients in medical insurance payments was firstly calculated to reflect the share of insurance claims for these patients. It equals to the cumulative sum of insurance payment for each patient in the previous year multiplied by the reimbursement ratio of this patient. Then, insurance payment for each weight equals to the predetermined funding budgets divided by the total weight values calculated in the previous step. Lastly, insurance payments for each contracted patient equals to insurance payment for each weight multiplied by the reimbursement ratio of this patient.
The second part is APGs-based payment for outpatients who do not have a contract with the hospital. Similar to DRGs system, an outpatient classification system is developed to serve as the basic unit of payment. In Jinhua, APGs have three categories: procedure, internal medical and ancillary group. Patients in each APG have similar clinical characteristics, resource use and costs. After classification, each APG group is assigned a certain number of points to reflect the relative resource utilisation. The specific point volume for each APG group is determined by the average expenditure per case in this APG group relative to the average expenditure per case in all APG groups. Monetary payments for one-point equals to the predetermined funding budgets divided by the point sum of all cases in APG groups rendered by all hospitals. As a result, the actual reimbursements for each hospital depend on the total points of outpatient services rendered by itself and each point value. Different from the usual practice of the case-base payment pre-setting the fixed reimbursements for each case, insurance payment for outpatient in each APG is floating.
Materials and Methods
Study Design and Setting
A quasi-experimental study design with ecologically controlled ITSA was employed. ITSA allowed us to determine the effects of “APGs + capitation” payment scheme through secular time trends by testing their differences before and after the implementation of the reform. Using a concurrent control group (those that had not yet been exposed to this funding reforms) helped control the unmeasured time-varying confounding effect.
We conducted the study in Zhejiang Province in eastern China. The “APGs + capitation” payment reform started in Jinhua City, located in central Zhejiang. Thus, Jinhua was selected as the intervention group. Considering their comparable socioeconomic status and health resources (Table 1), three neighbouring cities (Taizhou, Huzhou and Quzhou) were recruited as the control group.14 We searched the important health policies implemented by the sample cities during the study period. Some health policies (eg, the price reform of medical services and the integrated county healthcare consortium) that may influence the outcome indicators were introduced in such period. However, the control and intervention groups were selected from Zhejiang Province, and they all implemented these policies. This way ensures the comparability of the control and intervention groups.
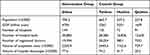 |
Table 1 Socioeconomic Status and Health Resources of Intervention and Control Cities in 2020 |
Data Source
The data used in this study were extracted from the Zhejiang Public Hospital Reform Monitoring System. This system covered approximately 70% of all public hospitals in Zhejiang, and each hospital needs to report monthly data regarding service delivery and associated revenues and expenses. The reporting system adopted logical verification and some quality control indicators to identify and manage missing or incorrect data for ensuring completeness and accuracy of the reported data.
All general public hospitals in sample cities were selected. As a result, 19 hospitals in Jinhua (7 municipal hospitals and 12 county hospitals), 14 hospitals in Taizhou (6 municipal hospitals and 8 county hospitals), 15 hospitals in Huzhou (5 municipal hospitals and 10 county hospitals) and 10 hospitals in Quzhou (4 municipal hospitals and 6 county hospitals) were included. For each hospital, monthly data points were collected for 36 consecutive months from January 2019 to December 2021. A total of 2088 complete observation points were included in the analysis.
Outcome Variables
Based on the purpose of this study and availability of data, the effects of “APGs + capitation” payment scheme were measured by two sets of outcome indicators in line with the literature:15,16 service volume and care expenditures. The outpatient visit was used to measure service volumes. The care expenditures were measured by five types of expenditures per outpatient visit: total expenditures, OOP payments, drug expenditures, consumable expenditures and examination expenditures.
Data Analysis
Monthly mean values and standard deviations (SDs) of the outcome variables were calculated and compared between the pre-and post-intervention period using Student’s t-tests.
The ITSA with control group was performed to compare the outcome variables between the intervention and control groups and between the pre- and post-intervention periods.17,18 Given the strong quasi-experimental research design, the ecological controlled ITSA model used a comparison group not exposed to the intervention to alleviate the validity concerns. This way also provides the evaluation on the longitudinal effects of health policies. The model employs the following equation:
where Yt represents outcome variables measured at each monthly time point t. Tt is continuous variable representing the months since the start of observation. Xt is a dummy variable, with assignment of 0 and 1 representing before and after intervention, respectively. Z is also a dummy variable, with 0 for the control group and 1 for the intervention group. XtTt, ZTt and ZXtTt represent all interaction terms of these variables. β0 is the intercept of the control group before intervention. β1 and β3 represent the slope of the control group in pre- and post-intervention period, respectively. β2 is the change in trend of the control group after intervention. β4 and β5 are differences in the intercepts and slopes between intervention and control groups prior to the intervention; β6 and β7 indicate the differences in level and slope changes after intervention between intervention and control groups. The effects of payment reform were identified by observing whether β6 and β7 are statistically significant. If p<0.05 for β6 and β7, then the “APGs + capitation” payment scheme has a significant effect on outcome variables Yt.
ITSA was conducted in municipal and county hospitals separately. January 2020 and January 2021 were set as cut-off time points for municipal and county hospitals, respectively. Given that the policy effects on the outcome indicators may take some time to occur, we performed sensitivity analyses to observe ITSA results using February instead of January as a cut-off time point. The results remain largely changed (Supplementary File 1). Considering that autocorrelation of the data must be considered, ordinary least square (OLS) regression using Newey–West standard errors was adopted to handle autocorrelation and potential heteroskedasticity.18 All statistical analyses were performed using Stata 14.0.
Results
Characteristics of Outcome Variables
Table 2 reports the monthly mean (SD) values of outcome variables in intervention and control groups by municipal and county hospitals. Prior to the reform, the intervention group had similar characteristic compared with the control group in the six outcome variables. After the intervention, the outpatient visits in municipal hospitals for intervention and control groups appeared to be decreased, but that in the county hospitals seemed to be increased. In terms of healthcare expenditures, the total and drug expenditures per visit slightly declined in the intervention group compared with that in the control group. However, consumable and examination expenditures per visit increased in the intervention and control groups from pre-intervention to post-intervention. The data also showed that the intervention group experienced a drop in OOP payments per outpatient visit compared with an increase in the control ones.
 |
Table 2 Monthly Mean (SD) Values of Outcome Variables in Intervention and Control Groups |
Effects of the Payment Reform on Municipal Hospitals
Table 3 and Figure 2 report the difference-in-difference results through ITSA for municipal hospitals. Prior to the payment reform, differences in outcome measures in the levels and slopes between intervention and control groups were insignificant except for consumable expenditures per outpatient visit (β4=−13.68, p=0.021). It means two groups are comparable prior to the policy intervention.
 |
Table 3 Effects of “APGs + Capitation” Payment Scheme in Municipal Hospitals |
In the post-intervention period, the trend of outpatient visits in the intervention group experienced a drop compared with that in the control ones (β7=−1417.54, p=0.048). The reform also led to a significant decline in the trend of total expenditures (β7=−3.99, p=0.018) and drug expenditures per visit (β7=−1.41, p=0.019), as well as the level of consumable expenditures per outpatient visit (β6=−6.89, p=0.044). However, the changes in examination expenditures and OOP payments per outpatient visit were not remarkable.
Effects of the Payment Reform on County Hospitals
Table 4 and Figure 3 provide the controlled ITSA results for county hospitals. County hospitals in the intervention and control groups showed similar pre-intervention levels and trends of outcomes, which indicates that the two groups are sufficiently comparable. After the introduction of the new payment method, the intervention group had a higher increasing trend of outpatient visits than the control group (β7=1058.04, p=0.041). The reform also caused the immediate declines in drug (β6=−10.96, p=0.009) and consumable expenditures per outpatient visit (β6=−4.78, p=0.041), whereas the changes in other indicators on hospital expenditures were insignificant.
 |
Table 4 Effects of “APGs+ Capitation” Payment Scheme in County Hospitals |
Discussion
To our knowledge, this study is the first to employ a quasi-experimental design for examining the effects of “APGs + capitation” payment scheme for outpatient care in China. Our study shows that this innovative payment has the potential to constrain rapid growth of outpatient expenditures, but some unexpected consequences need to be prevented.
The decrease in outpatient visits in municipal hospitals and increase in that in county hospitals reflect that the hospitals are very responsive to the funding reform. The “APGs + capitation” payment can motivate providers to reduce cost per case and avoid unnecessary medical service provision.9,15 Thus, those with mild conditions are not financially beneficial to municipal hospitals because medical insurance payment for those outpatients is relatively low. By contrast, they are encouraged to seek healthcare services from the county hospitals, which is usually cheaper than that delivered in municipal hospitals. This consequence is in line with the expectations of establishing the hierarchical medical system in China, which assigns mild patients at the primary care setting and severe patients at higher level hospitals.19
As expected, the growth trend of outpatient expenditures per visit reduced significantly after the funding reform. Previous study showed patient and cost-shifting from inpatient to outpatient setting with the adoption of DRGs system, which resulted in a rapid growth of outpatient expenditures.6,20 Encouragingly, this innovative payment scheme corrected the aforementioned unwanted responses. The unit of reimbursement under APGs system, as a case-based payment method, is similar to that under the DRGs. Hospitals are highly incentivised to deliver more cost-effective services, and inefficient and unnecessary practices are reduced to minimise the cost in each APG case.21 Similarly, the retention for surplus and the non-replenishment for overspending under capitation-based payment also generated strong financial incentives for providers to control the increase in medical expenditures.22
From further observing the changes in different types of expenditures in outpatient setting after the “APGs + capitation” payment scheme was introduced, we found that the decrease in outpatient expenditures might attribute to the drop in drug and consumable expenditures. Obviously, incentive transformation from FFS to this new case-based payment means over prescription and consumable use in care provision need to be reduced to gain profits rather than increasing the service volume.13 However, the change in outpatient examination expenditures was not apparent after policy intervention. One possible explanation is that reimbursement of medical insurance for outpatient examinations is very low in China, and patients nearly pay for these services by themselves, such as computed tomography and magnetic resonance imaging.23 Insurance payment under this case-based system does not involve reimbursements for outpatient examination, which results in the limited effect of the reform in containing this part of expenditures.24 The finding reminds policymakers that insurance reimbursements for outpatient service items should be further expanded to prevent cost-shifting from insured to uninsured services.25,26
Notably, OOP payments in municipal and county hospitals presented an insignificant decrease after the implementation of new payment method. In Chinese medical insurance system, the hospital expenditure consists of insurance payment and OOP payments.27 The current “APGs + capitation” payment system for outpatient care is only applied to insurance payment but not to the total expenditures. Thus, the risk of cost-shifting to OOP payments might occur to compensate the potential revenue loss in the hospital.24 However, this strategic behaviour in response to the new case-based payment need to be further investigated by observing the long-term change trend in OOP payments. From a policy perspective, this result provides the practical implication that redesigning the current payment scheme in outpatient settings should consider OOP payments and strengthen the supervision risk-shifting behaviours.
Several limitations in this study should be noted. Firstly, the impacts of APGs-based payment and capitation funding were not analysed separately. Consequently, we do not know which payment method is responsible for the observed results. Secondly, limited outcome indicators were used in current study, which resulted in the fact that our data only captured the part of picture on the effect of payment reforms. Future study should consider adding other outcome variables to comprehensively reflect the reform effects. Thirdly, caution should be exercised in generalising the empirical findings of this study because we collected the data from only one pilot city. Fourthly, the longer-term effect of this new case-based payment scheme needs to be followed up because only 3 years of observation data were used in this study. Fifthly, although intervention and control groups were affected by some health policies (eg the price reform of medical services and the reform of integrated medical system) and the COVID-19 pandemic in the study period, their responses may be different, which resulted in the deviation in the estimation of the impacts of outpatient payment reforms.
Conclusions
The “APGs + capitation” payment scheme for outpatient care generates positive effects on constraining drug, consumable and total outpatient expenditures. It also alleviates the rapidly rising outpatient volume in Chinese municipal hospitals. However, the findings that outpatient examination expenditures and OOP payments have not changed significantly after the reform remind policy makers to prevent cost-shifting and risk-shifting to uninsured service items when expanding this innovative episode-based payment method to more regions.
Abbreviations
APGs, Ambulatory Patient Groups; FFS, fee-for-service; DRGs, diagnosis-related groups; ITSA, interrupted time-series analysis; OOP, out-of-pocket; SDs, standard deviations; OLS, ordinary least squares; CT, computed tomography; MRI, magnetic resonance imaging.
Data Sharing Statement
The datasets used and analysed in the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Ethics Committee of Hangzhou Normal University, and managers in sample hospitals gave their written informed consent.
Acknowledgments
We thank the managers in the sample hospitals for their help in collecting the data.
Funding
This study was supported by the Soft Science Research Program of Zhejiang Province (NO. 2023C35034) and the Scientific Research Foundation for Scholars of HZNU (NO. 4265C50221204120).
Disclosure
The authors declare no competing interests in this work.
References
1. China NBoSo. China Statistical Yearbook. Beijing: China Statistics Press; 2019.
2. Gao C, Xu F, Liu GG. Payment reform and changes in health care in China. Soc Sci Med. 2014;111:10–16. doi:10.1016/j.jval.2013.03.1002
3. Council TGOotS. Guidance for the basic health insurance on further deepening reform on provider payment; 2017. Available from: http://www.gov.cn/zhengce/content/2017-06/28/content_5206315.htm.
4. Zou K, Li HY, Zhou D, Liao ZJ. The effects of diagnosis-related groups payment on hospital healthcare in China: a systematic review. BMC Health Serv Res. 2020;20(1):1–11. doi:10.1186/s12913-020-4957-5
5. Ghazaryan E, Delarmente BA, Garber K, Gross M, Sriudomporn S, Rao KD. Effectiveness of hospital payment reforms in low- and middle-income countries: a systematic review. Health Policy Plan. 2021;36:1344–1356. doi:10.1093/heapol/czab050
6. Zhang T, Lu B, Yan Z, Huang X, Lu W. Impacts of a new episode-based payment scheme on volume, expenditures, and efficiency in public hospitals: a quasi-experimental interrupted time-series study in Jinhua, China. Risk Manag Healthc Policy. 2022;15:1659–1669. doi:10.2147/RMHP.S376516
7. China NBoSo. China Statistical Yearbook. Beijing: China Statistics Press; 2021.
8. Administration JHS. The outpatient payment method of basic medical insurance in Jinhua; 2020. Available from: http://ybj.jinhua.gov.cn/art/2022/6/8/art_1229240961_1775851.html.
9. Goldfield N, Averill R, Eisenhandler J, Grant T. Ambulatory patient groups, version 3.0—a classification system for payment of ambulatory visits. J Ambulat Care Manage. 2008;31(1):2–16. doi:10.1097/01.jac.0000304091.21087.08
10. Tsiachristas A, Dikkers C, Boland MRS, Rutten-van Molken M. Exploring payment schemes used to promote integrated chronic care in Europe. Health Policy (New York). 2013;113(3):296–304. doi:10.1016/j.healthpol.2013.07.007
11. Glazier RH, Green ME, Frymire E, et al. Do incentive payments reward the wrong providers? A study of primary care reform in Ontario, Canada. Health Aff. 2019;38(4):624–632. doi:10.1377/hlthaff.2018.05272
12. Amico P, Pope GC, Meadow A, West P. Episode-based payment for the medicare outpatient therapy benefit. Arch Phys Med Rehabil. 2016;97(8):1323–1328. doi:10.1016/j.apmr.2016.02.028
13. Atkinson G, Murray R. The use of ambulatory patient groups for regulation of hospital ambulatory surgery revenue in Maryland. J Ambulat Care Manage. 2008;31(1):17–23. doi:10.1097/01.JAC.0000304092.28711.e2
14. Bureau ZS. Zhejiang Statistical Yearbook-2020. Beijing: China Statistics Press; 2020.
15. He DF, Mellor JM. Hospital volume responses to Medicare’s Outpatient Prospective Payment System: evidence from Florida. J Health Econ. 2012;31(5):730–743. doi:10.1016/j.jhealeco.2012.06.001
16. Yuan BB, He L, Meng QY, Jia LY. Payment methods for outpatient care facilities. Cochrane Database Syst Rev. 2017;(1):CD011865. doi:10.1002/14651858.CD011153.pub2
17. Linden A, Adams JL. Applying a propensity score‐based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011;17(6):1231–1238. doi:10.1111/j.1365-2753.2010.01504.x
18. Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015;15(2):480–500. doi:10.1177/1536867X1501500208
19. Zhou ZL, Zhao YX, Shen C, Lai S, Nawaz R, Gao JM. Evaluating the effect of hierarchical medical system on health seeking behavior: a difference-in-differences analysis in China. Soc Sci Med. 2021;268. doi:10.1016/j.socscimed.2020.113372
20. Kim SJ, Han KT, Kim W, Kim SJ, Park EC. Early impact on outpatients of mandatory adoption of the diagnosis-related group-based reimbursement system in Korea on use of outpatient care: differences in medical utilization and presurgery examination. Health Serv Res. 2018;53(4):2064–2083. doi:10.1111/1475-6773.12749
21. He D, Mellor JM. Do changes in hospital outpatient payments affect the setting of care? Health Serv Res. 2013;48(5):1593–1616. doi:10.1111/1475-6773.12069
22. Xu GC, Luo Y, Li Q, Wu MF, Zhou ZJ. Standardization of type 2 diabetes outpatient expenditure with bundled payment method in China. Chin Med J. 2016;129(8):953–959. doi:10.4103/0366-6999.179796
23. Lu G, Ls B, Qmc D, Xk E, Mg F, Feng LF. Effect of healthcare system reforms on public hospitals’ revenue structures: evidence from Beijing, China. Soc Sci Med. 2021;283:114210. doi:10.1016/j.socscimed.2021.114210
24. He DF, Mellor JM. Medicare payment and hospital provision of outpatient care to the uninsured. Health Serv Res. 2016;51(4):1388–1406. doi:10.1111/1475-6773.12433
25. Pauly M, Town R. Maryland exceptionalism? All-payers regulation and health care system efficiency. J Health Polit Policy Law. 2012;37(4):697–707. doi:10.1215/03616878-1597502
26. Murray R. The case for a coordinated system of provider payments in the United States. J Health Polit Policy Law. 2012;37(4):679–695. doi:10.1215/03616878-1597493
27. Xu J, Jian W, Zhu K, Kwon S, Fang H. Reforming public hospital financing in China: progress and challenges. BMJ. 2019;365:l4015. doi:10.1136/bmj.l4015
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.